Abstract
Asynchronous rotational-speed modulation of a continuous-flow left ventricular assist device (LVAD) can increase pulsatility; however, the feasibility of hemodynamic modification by asynchronous modulation of an LVAD has not been sufficiently verified. We evaluated the acute effect of an asynchronous-modulation mode under LVAD support and the accumulated effect of 6 consecutive hours of driving by the asynchronous-modulation mode on hemodynamics, including both ventricles, in a coronary microembolization-induced acute-myocardial injury sheep model. We evaluated 5-min LVAD-support hemodynamics, including biventricular parameters, by switching modes from constant-speed to asynchronous-modulation in the same animals (“acute-effect evaluation under LVAD support”). To determine the accumulated effect of a certain driving period, we evaluated hemodynamics including biventricular parameters after weaning from 6-hour (6 h) LVAD support by constant-speed or asynchronous-modulation mode (“6h-effect evaluation”). The acute-effect evaluation under LVAD support revealed that, compared to the constant-speed mode, the asynchronous-modulation mode increased vascular pulsatility but did not have significantly different effects on hemodynamics, including both ventricles. The 6 h-effect evaluation revealed that the hemodynamics did not differ significantly between the two groups except for some biventricular parameters which did not indicate negative effects of the asynchronous-modulation mode on both ventricles. The asynchronous-modulation mode could be feasible to increase vascular pulsatility without causing negative effects on hemodynamics including both ventricles. Compared to the constant-speed mode, the asynchronous-modulation mode increased pulsatility during LVAD support without negative effects on hemodynamics including both ventricles in the acute phase. Six hours of LVAD support with the asynchronous-modulation mode exerted no negative effects on hemodynamics, including both ventricles, after weaning from the LVAD.





Similar content being viewed by others
References
Mancini, D., and P. C. Colombo. Left ventricular assist devices: a rapidly evolving alternative to transplant. J. Am. Coll. Cardiol. 65:2542–2555, 2015.
Purohit, S. N., W. K. Cornwell 3rd., J. D. Pal, J. Lindenfeld, and A. V. Ambardekar. Living Without a pulse: the vascular implications of continuous-flow left ventricular assist devices. Circ. Heart Fail.11:e004670, 2018.
Muthiah, K., D. Conno, K. Ly, et al. Longitudinal changes in hemostatic parameters and reduced pulsatility contribute to non-surgical bleeding in patients with centrifugal continuous-flow left ventricular assist devices. J. Heart Lung Transplant. 35:743–751, 2016.
Kataria, R., and U. P. Jorde. Gastrointestinal bleeding during continuous-flow left ventricular assist device support: state of the field. Cardiol. Rev. 27:8–13, 2019.
Cowger, J., F. D. Pagani, J. W. Haft, M. A. Romano, K. D. Aaronson, and T. J. Kolias. The development of aortic insufficiency in left ventricular assist device-supported patients. Circ. Heart Fail. 3:668–674, 2010.
Mudd, J. O., J. D. Cuda, M. Halushka, K. A. Soderlund, J. V. Conte, and S. D. Russell. Fusion of aortic valve commissures in patients supported by a continuous axial flow left ventricular assist device. J. Heart Lung Transplant. 27:1269–1274, 2008.
Witman, M. A., R. S. Garten, J. R. Gifford, et al. Further peripheral vascular dysfunction in heart failure patients with a continuous-flow left ventricular assist device: the role of pulsatility. JACC Heart Fail. 3:703–711, 2015.
Amir, O., B. Radovancevic, R. M. Delgado 3rd., et al. Peripheral vascular reactivity in patients with pulsatile vs. axial flow left ventricular assist device support. J. Heart Lung Transplant. 25:391–394, 2006.
Soucy, K. G., G. A. Giridharan, Y. Choi, et al. Rotary pump speed modulation for generating pulsatile flow and phasic left ventricular volume unloading in a bovine model of chronic ischemic heart failure. J. Heart Lung Transplant. 34:122–131, 2015.
Umeki, A., T. Nishimura, M. Ando, et al. Alteration of LV end-diastolic volume by controlling the power of the continuous-flow LVAD, so it is synchronized with cardiac beat: development of a native heart load control system (NHLCS). J. Artif. Organs. 15:128–133, 2012.
Arakawa, M., T. Nishimura, Y. Takewa, et al. Alternation of left ventricular load by a continuous-flow left ventricular assist device with a native heart load control system in a chronic heart failure model. J. Thorac. Cardiovasc. Surg. 148:698–704, 2014.
Ising, M. S., M. A. Sobieski, M. S. Slaughter, S. C. Koenig, and G. A. Giridharan. Feasibility of pump speed modulation for restoring vascular pulsatility with rotary blood pumps. ASAIO J. 61:526–532, 2015.
Naito, N., T. Nishimura, K. Iizuka, et al. Rotational speed modulation used with continuous-flow left ventricular assist device provides good pulsatility. Interact. Cardiovasc. Thorac. Surg. 26:119–123, 2018.
Kishimoto, Y., Y. Takewa, M. Arakawa, et al. Development of a novel drive mode to prevent aortic insufficiency during continuous-flow LVAD support by synchronizing rotational speed with heartbeat. J. Artif. Organs. 16:129–137, 2013.
Cox, L. G., S. Loerakker, M. C. Rutten, B. A. de Mol, and F. N. van de Vosse. A mathematical model to evaluate control strategies for mechanical circulatory support. Artif. Organs. 33:593–603, 2009.
Chassagne, F., M. Miramontes, V. K. Chivukula, et al. In vitro investigation of the effect of left ventricular assist device speed and pulsatility mode on intraventricular hemodynamics. Ann. Biomed. Eng. 49:1318–1332, 2021.
Chen, Z., S. K. Jena, G. A. Giridharan, et al. Shear stress and blood trauma under constant and pulse-modulated speed CF-VAD operations: CFD analysis of the HVAD. Med. Biol. Eng. Comput. 57:807–818, 2019.
Ortiz, S., V. Vu, R. Montes, and K. May-Newman. Left ventricular flow dynamics with the HeartMate3 left ventricular assist device: effect of inflow cannula position and speed modulation. ASAIO J. 67:1301–1311, 2021.
Tuzun, E., K. Chorpenning, M. Q. Liu, et al. The effects of continuous and intermittent reduced speed modes on renal and intestinal perfusion in an ovine model. ASAIO J. 60:19–24, 2014.
Vandenberghe, S., P. Segers, J. F. Antaki, B. Meyns, and P. R. Verdonck. Hemodynamic modes of ventricular assist with a rotary blood pump: continuous, pulsatile, and failure. ASAIO J. 51:711–718, 2005.
Shimamura, J., T. Mizuno, Y. Takewa, et al. Miniaturized centrifugal ventricular assist device for bridge to decision: preclinical chronic study in a bovine model. Artif. Organs. 43:821–827, 2019.
Tanaka, S., T. Nishinaka, A. Umeki, et al. Coronary microembolization sheep model by adjusting the number of microspheres based on coronary blood flow. Artif. Organs. 47:138–147, 2022.
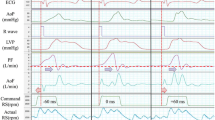
Soucy, K. G., S. C. Koenig, G. A. Giridharan, M. A. Sobieski, and M. S. Slaughter. Defining pulsatility during continuous-flow ventricular assist device support. J. Heart Lung Transplant. 32:581–587, 2013.
Krabatsch, T., M. Schweiger, M. Dandel, et al. Is bridge to recovery more likely with pulsatile left ventricular assist devices than with nonpulsatile-flow systems? Ann. Thorac. Surg. 91:1335–1340, 2011.
Kato, T. S., A. Chokshi, P. Singh, et al. Effects of continuous-flow versus pulsatile-flow left ventricular assist devices on myocardial unloading and remodeling. Circ. Heart Fail. 4:546–553, 2011.
Amacher, R., A. Weber, H. Brinks, et al. Control of ventricular unloading using an electrocardiogram-synchronized Thoratec paracorporeal ventricular assist device. J. Thorac. Cardiovasc. Surg. 146:710–717, 2013.
Amacher, R., G. Ochsner, and M. Schmid Daners. Synchronized pulsatile speed control of turbodynamic left ventricular assist devices: review and prospects. Artif. Organs. 38:867–875, 2014.
Tran, T., A. Muralidhar, K. Hunter, et al. Right ventricular function and cardiopulmonary performance among patients with heart failure supported by durable mechanical circulatory support devices. J. Heart Lung Transplant. 40:128–137, 2021.
Bouwmeester, J. C., J. Park, J. Valdovinos, and P. Bonde. Wave intensity analysis of right ventricular function during pulsed operation of rotary left ventricular assist devices. ASAIO J. 65:465–472, 2019.
Kaul, S. The interventricular septum in health and disease. Am. Heart J. 112:568–581, 1986.
Klima, U. P., M. Y. Lee, J. L. Guerrero, P. J. Laraia, R. A. Levine, and G. J. Vlahakes. Determinants of maximal right ventricular function: role of septal shift. J. Thorac. Cardiovasc. Surg. 123:72–80, 2022.
Moon, M. R., A. F. Bolger, A. DeAnda, et al. Septal function during left ventricular unloading. Circulation. 95:1320–1327, 1997.
Houston, B. A., K. B. Shah, M. R. Mehra, and R. J. Tedford. A new “twist” on right heart failure with left ventricular assist systems. J. Heart Lung Transplant. 36:701–707, 2017.
Topilsky, Y., J. K. Oh, D. K. Shah, et al. Echocardiographic predictors of adverse outcomes after continuous left ventricular assist device implantation. JACC Cardiovasc Imaging. 4:211–222, 2011.
Sack, K. L., Y. Dabiri, T. Franz, et al. Investigating the role of interventricular interdependence in development of right heart dysfunction during LVAD support: a patient-specific methods-based approach. Front Physiol. 9:520, 2018.
Anne Dual, S., A. Nayak, Y. Hu, et al. Does size matter for female continuous-flow LVAD recipients? A translational approach to a decade long question. ASAIO J. 68:21–27, 2022.
Acknowledgements
This work was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI Grant Number JP21K08853 and Nipro Corporation. We would like to thank KN International and Editage for English proofreading.
Author information
Authors and Affiliations
Contributions
ST, TN, AU, TT, TM, and MO substantially contributed to the study’s conception and design. ST, TN, AU, TM, SI, TM, and TT contributed to the data acquisition. All authors contributed to the data analysis and interpretation. ST drafted the manuscript, and all authors revised it. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Tomohiro Nishinaka reports collaborative research agreements with Nipro Corporation and Senko Medical Instrument Mfg. Co., Ltd. The other authors have no conflicts of interest to declare.
Additional information
Associate Editor Ender A. Finol oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tanaka, S., Nishinaka, T., Umeki, A. et al. Hemodynamic Evaluation of Asynchronous Speed Modulation of a Continuous-Flow Left Ventricular Assist Device in an Acute-Myocardial Injury Sheep Model. Ann Biomed Eng 52, 364–375 (2024). https://doi.org/10.1007/s10439-023-03383-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-023-03383-y