Abstract
Purpose
Pancreatic cystic lesions (PCLs) include various types of cysts. Accurate preoperative diagnosis is essential to avoid unnecessary surgery on benign cysts. In this study, we aimed to identify the factors associated with misdiagnosis in preoperative endoscopic ultrasound (EUS) imaging and clinicopathological findings for PCLs.
Methods
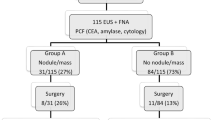
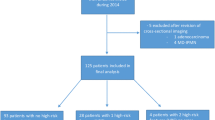
This study included 302 surgically resected patients with PCLs who underwent preoperative EUS. The preoperative EUS findings were re-evaluated and compared with the pathological diagnosis. Additionally, the factors associated with misdiagnosis of PCLs were investigated by multivariate analysis.
Results
The preoperative diagnoses of PCLs were intraductal papillary mucinous neoplasm (IPMN) in 213 patients (70.5%), mucinous cystic neoplasm (MCN) in 33 patients (10.9%), serous neoplasm (SN) in 7 patients (2.3%), cystic degeneration cyst of solid tumor in 46 patients (15.2%), and pancreatic cancer with cystic degeneration in three patients (1.0%). A discrepancy between preoperative and postoperative diagnosis was found in 47 patients (15.6%). Based on the pathological diagnosis, the sensitivity of preoperative EUS imaging was IPMN 97.6% (206/211), MCN 90.0% (18/19), cystic degeneration 87.1% (27/31), and SN 15.4% (2/13). Multivariate analysis revealed that main pancreatic duct (MPD) communication ( − ) (odds ratio (OR), 4.54; 95% confidence interval (CI) 1.29–15.9), honeycomb-like structure ( +) (OR, 14.7; 95% CI 2.61–83.3), and MPD size ≦ 2 mm (OR, 16.3; 95% CI 3.93–67.6) were independently associated with misdiagnosis.
Conclusion
For cases in which MCN and cystic degeneration of solid tumor are presumed based on preoperative EUS imaging and cases with PCLs with a honeycomb-like structure, diagnosis with multimodalities or fluid analysis with EUS-guided fine-needle aspiration should be considered.


Similar content being viewed by others
References
Zerboni G, Signoretti M, Crippa S, et al. Systematic review and meta-analysis: prevalence of incidentally detected pancreatic cystic lesions in asymptomatic individuals. Pancreatology. 2019;19:2–9.
Matsubara S, Tada M, Akahane M, et al. Incidental pancreatic cysts found by magnetic resonance imaging and their relationship with pancreatic cancer. Pancreas. 2012;41:1241–6.
Kromrey ML, Bülow R, Hübner J, et al. Prospective study on the incidence, prevalence and 5-year pancreatic-related mortality of pancreatic cysts in a population-based study. Gut. 2018;67:138–45.
Kneuertz PJ, Pitt HA, Bilimoria KY, et al. Risk of morbidity and mortality following hepato-pancreato-biliary surgery. J Gastrointest Surg. 2012;16:1727–35.
Probst P, Hüttner FJ, Meydan Ö, et al. Evidence map of pancreatic surgery-a living systematic review with meta-analyses by the international study group of pancreatic surgery (ISGPS). Surgery. 2021;170:1517–24.
Min JH, Kim YK, Kim SK, et al. Intraductal papillary mucinous neoplasm of the pancreas: diagnostic performance of the 2017 international consensus guidelines using CT and MRI. Eur Radiol. 2021;31:4774–84.
Ohno E, Hirooka Y, Kawashima H, et al. Endoscopic ultrasonography for the evaluation of pancreatic cystic neoplasms. J Med Ultrason. 2020;47:401–11.
Alkaade S, Chahla E, Levy M. Role of endoscopic ultrasound-guided fine-needle aspiration cytology, viscosity, and carcinoembryonic antigen in pancreatic cyst fluid. Endosc Ultrasound. 2015;4:299–303.
Singhi AD, McGrath K, Brand RE, et al. Preoperative next-generation sequencing of pancreatic cyst fluid is highly accurate in cyst classification and detection of advanced neoplasia. Gut. 2018;67:2131–41.
McCarty TR, Garg R, Rustagi T. Pancreatic cyst fluid glucose in differentiating mucinous from nonmucinous pancreatic cysts: a systematic review and meta-analysis. Gastrointest Endosc. 2021;94:698–712.
Hirooka Y, Goto H, Itoh A, et al. Case of intraductal papillary mucinous tumor in which endosonography-guided fine-needle aspiration biopsy caused dissemination. J Gastroenterol Hepatol. 2003;18:1323–4.
Yamabe A, Irisawa A, Shibukawa G, et al. Rare condition of needle tract seeding after EUS-guided FNA for intraductal papillary mucinous carcinoma. Endosc Int Open. 2016;4:E756–8.
Minaga K, Takenaka M, Katanuma A, et al. Needle tract seeding: an overlooked rare complication of endoscopic ultrasound-guided fine-needle aspiration. Oncology. 2017;93(Suppl 1):107–12.
Marchegiani G, Andrianello S, Crippa S, et al. Actual malignancy risk of either operated or nonoperated presumed mucinous cystic neoplasms of the pancreas under surveillance. Br J Surg. 2021;108:1097–104.
de Pretis N, Mukewar S, Aryal-Khanal A, et al. Pancreatic cysts: diagnostic accuracy and risk of inappropriate resections. Pancreatology. 2017;17:267–72.
Hijioka S, Hara K, Mizuno N, et al. Morphological differentiation and follow-up of pancreatic cystic neoplasms using endoscopic ultrasound. Endosc Ultrasound. 2015;4:312–8.
Tanaka M, Chari S, Adsay V, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006;6:17–32.
Tanaka M, Fernández-del Castillo C, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183–97.
Tanaka M, Fernández-Del Castillo C, Kamisawa T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017;17:738–53.
Yamao K, Yanagisawa A, Takahashi K, et al. Clinicopathological features and prognosis of mucinous cystic neoplasm with ovarian-type stroma: a multi-institutional study of the Japan pancreas society. Pancreas. 2011;40:67–71.
Kimura W, Moriya T, Hirai I, et al. Multicenter study of serous cystic neoplasm of the Japan pancreas society. Pancreas. 2012;41:380–7.
Terminology and Diagnostic Criteria Committee, Japan Society of Ultrasonics in Medicine. Ultrasonographic diagnostic criteria for pancreatic cancer. J Med Ultrason. 2013;40:497–504.
Khashab MA, Kim K, Lennon AM, et al. Should we do EUS/FNA on patients with pancreatic cysts? The incremental diagnostic yield of EUS over CT/MRI for prediction of cystic neoplasms. Pancreas. 2013;42:717–21.
Ridtitid W, Halawi H, DeWitt JM, et al. Cystic pancreatic neuroendocrine tumors: outcomes of preoperative endosonography-guided fine needle aspiration, and recurrence during long-term follow-up. Endoscopy. 2015;47:617–25.
Simons-Linares CR, Yadav D, Lopez R, et al. The utility of intracystic glucose levels in differentiating mucinous from nonmucinous pancreatic cysts. Pancreatology. 2020;20:1386–92.
Reid MD, Choi HJ, Memis B, et al. Serous neoplasms of the pancreas: a clinicopathologic analysis of 193 cases and literature review with new insights on macrocystic and solid variants and critical reappraisal of so-called “serous cystadenocarcinoma.” Am J Surg Pathol. 2015;39:1597–610.
Zhao P, deBrito P, Ozdemirli M, et al. Solid-pseudopapillary neoplasm of the pancreas: awareness of unusual clinical presentations and morphology of the clear cell variant can prevent diagnostic errors. Diagn Cytopathol. 2013;41:889–95.
Springer S, Wang Y, Dal Molin M, et al. A combination of molecular markers and clinical features improve the classification of pancreatic cysts. Gastroenterology. 2015;149:1501–10.
Yoon WJ, Daglilar ES, Pitman MB, et al. Cystic pancreatic neuroendocrine tumors: endoscopic ultrasound and fine-needle aspiration characteristics. Endoscopy. 2013;45:189–94.
Liu Y, Shi S, Hua J, et al. Differentiation of solid-pseudopapillary tumors of the pancreas from pancreatic neuroendocrine tumors by using endoscopic ultrasound. Clin Res Hepatol Gastroenterol. 2020;44:947–53.
Hashimoto S, Hirooka Y, Kawabe N, et al. Role of transabdominal ultrasonography in the diagnosis of pancreatic cystic lesions. J Med Ultrason. 2020;47:389–99.
Kosmahl M, Pauser U, Anlauf M, et al. Pancreatic ductal adenocarcinomas with cystic features: neither rare nor uniform. Mod Pathol. 2005;18:1157–64.
Youn SY, Rha SE, Jung ES, et al. Pancreas ductal adenocarcinoma with cystic features on cross-sectional imaging: radiologic-pathologic correlation. Diagn Interv Radiol. 2018;24:5–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical approval
This study was approved by the Institutional Review Board of Nagoya University Hospital (IRB approval No. 2015–0387) and was conducted in accordance with the provisions of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Ohno, E., Ishikawa, T., Mizutani, Y. et al. Factors associated with misdiagnosis of preoperative endoscopic ultrasound in patients with pancreatic cystic neoplasms undergoing surgical resection. J Med Ultrasonics 49, 433–441 (2022). https://doi.org/10.1007/s10396-022-01205-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-022-01205-7