Abstract
Background
Physical activity is particularly low in South Africa and contributes to chronic conditions. This study aimed to determine physical activity levels in a South African community, using the physical activity vital sign (PAVS), and identify associations between physical activity and key health outcomes.
Methods
A cross-sectional study used community health workers to collect PAVS data, blood pressure and self-reported medical history from 2282 participants living in Soweto, Johannesburg. Physical activity was defined as meeting or not meeting WHO guidelines of ≥ 150 min/week. Hypertension was defined according to the International Society of Hypertension guidelines.
Results
The study population included 1161 women and 1121 men. Administering the PAVS was quick (29.5 ± 43.4 s). Only 19.8% of the total population reported meeting the guidelines, and it was significantly lower in women (17.6%) compared with men (22.1%). The logistic regression models demonstrated significant association between not meeting physical activity guidelines and hypertension (adjusted odd ratio [AOR] 0.77, 95% CI 0.61–0.97, p = 0.032), current smoking (AOR 0.73, 95% CI 0.55–0.97, p = 0.030) and past smoking (AOR 0.61, 95% CI 0.44–0.83, p = 0.002).
Conclusions
This study demonstrates the validity of using the PAVS in an underserved community. The observed associations highlight the potential of advocating physical activity as a feasible intervention for improving the health of urban-dwelling Black South Africans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Physical inactivity is one of the leading causes of early mortality and morbidity globally (Katzmarzyk et al. 2022). This behaviour accounts for approximately 1.3 million deaths globally in individuals aged > 25 years (Milton et al. 2023). Physical inactivity has a strong positive association with disorders such as hypertension, which remains a heavy burden in South Africa (Kohli-Lynch et al. 2022). Conversely, being physically active has beneficial effects on reducing body fat and cardiometabolic disease risk factors (Gradidge et al. 2014). There are numerous questionnaires and survey tools available to measure individuals’ physical activity levels (including the commonly used global physical activity questionnaire (Chu et al. 2015), rapid assessment of physical activity (Topolski et al. 2006), CHAMPS Physical Activity Questionnaire (Hekler et al. 2012) and Physical Activity Questionnaire for Older Children (PAQ-C) and Adolescents (PAQ-A) (Kowalski et al. 2004)); however, few can be administered and scored rapidly by individuals without an in-depth background in physical activity (van Poppel et al. 2010) and completing the instruments can require an extended length of time for the patient and researcher. Instruments to quickly determine physical activity patterns in individuals with or at risk within under resourced health services are therefore urgently needed.
The Physical Activity Vital Sign (PAVS) is a simple self-reported instrument to determine whether adults over 18 years are meeting the physical activity guidelines of at least 150 min of moderate-to-vigorous physical activity weekly (Bull et al. 2020). PAVS has been validated in an American population (Greenwood et al. 2010; Coleman et al. 2012) and its use in clinical practice has been associated with significant weight loss in individuals with obesity (body mass index [BMI] ≥ 30 kg/m2) and improved glycaemic control in persons living with type 2 diabetes (Grant et al. 2014). The PAVS is significantly associated with cardiometabolic risk factors, BMI and patient disease burden (Young et al. 2014; McCarthy et al. 2021). However, the use of the PAVS has been limited primarily to health systems in the United States (Coleman et al. 2012; Greenwood et al. 2010; Vancampfort et al. 2016). Therefore, data on its use in both lower resource countries and in community settings with inadequate access to primary healthcare is limited.
Typically, insufficient primary healthcare services have suggested strategies such as task-shifting and increased community outreach through the utilisation of community health workers (CHWs) (Joshi et al. 2014). The integration of CHWs into the healthcare system for task-shifting purposes has been central to addressing health disparities in many low- and middle-income countries (LMICs) (Peer et al. 2021; Brady et al. 2022). CHWs provide a range of preventive health services, from health education to basic health screening, counselling, and referral services for maternal and child health and other chronic illnesses such as HIV/AIDS and tuberculosis (Thomas et al. 2021; Goudge et al. 2020). As a result, these frontline workers have contributed to improved health behaviour for many of their patients and local communities (Thomas et al. 2021; Goudge et al. 2020). While CHW intervention programmes have proved successful for primary healthcare service provision (Lewin et al. 2010; Ajisegiri et al. 2023; Rawal et al. 2020), such efforts require a change of focus from their historical roles in maternal and child health and infectious disease to now consider lifestyle behaviours associated with NCDs, assessing physical activity and providing basic physical activity counselling.
Therefore, the aims of this study were twofold: (1) determining the practicality of screening for physical activity using the PAVS administered by CHWs as a component of a home-based blood pressure screening programme; and (2) examining associations between physical activity levels, assessed through the PAVS, with other health outcome data collected during the home visit.
Methods
Study design, setting and participants
This study was conducted in Soweto, a historically disadvantaged urban township in Johannesburg, South Africa, with a population density of 4143 people per km2 (Bosire et al. 2020). This area is also reported to have a high prevalence of NCDs (i.e. hypertension, type 2 diabetes and mental health conditions) and comorbidities that impact the local population (Hopkins et al. 2021).
Participants for this study were identified during routine community and home-based health screening campaigns. CHWs went house-to-house over 4 months from 30 September 2021 to 28 January 2022 to conduct the health screening assessments. During the home visits, household members were informed of the study and assessed for eligibility to participate. To be eligible for inclusion, an individual had to be: (1) at least 18 years old; (2) willing and able to provide informed consent; (3) able to fully understand English; (4) not displaying any symptoms of COVID-19, including having a forehead temperature (using an infrared non-contact thermometer) of 37.5 ºC or above. The ethnicity of participants in this study was 99.5% Black Africans, and this is in line with the general population in Soweto (Stats 2012).
Ethical approval was obtained from the Human Research Ethics Committee (Medical) at the University of Witwatersrand [Ref. M200941 and M170334 renewed as M2203101]. All participants gave written informed consent prior to taking part in the study (consort diagram, Fig. 1), those not wishing to participate in the study were still offered the same health screening services as participants.
Study procedures
Following consent, participants were asked a series of questions to obtain sociodemographic data (age, sex and education level); self-reported medical history (including previous hypertension or diabetes diagnosis by a healthcare professional and medication use, history of heart attack, stroke and COVID-19 infection); and health behaviours (tobacco and alcohol use, COVID-19 vaccination). The questionnaire was developed by the International Society of Hypertension for the global May Measurement Month (MMM) initiative (Woodiwiss et al. 2020). Seated brachial blood pressure (BP) was measured using Omron automated devices (Omron M3 Connect, Kyoto, Japan) following the International Society of Hypertension (ISH) measurement guidelines (Unger et al. 2020) with BP and heart rate measured on the participants’ left and then right arm three times, with a 5-min rest period before measures and a 1-min rest interval between the measurements. The first BP measure on each arm was discarded and the second and third measures were averaged to get a final reading. If the difference between the second and third measures on either arm was greater than 5 mmHg, CHWs conducted a fourth measure so that the final average of the two readings was within a 5 mmHg range.
Self-reported physical activity data was then collected using the Physical Activity Vital Sign (PAVS) questionnaire consisting, of two questions: (1) “On average, how many days per week do you engage in moderate-to-vigorous physical activity (like a brisk walk)?” and (2) “On average, how many minutes do you engage in physical activity at this level?” (Greenwood et al. 2010). These responses are multiplied to give minutes per week of reported moderate-to-vigorous physical activity.
Data collection and analysis
The screening protocol was administered in English by the CHWs using tablets. Study data were collected and managed using REDCap electronic data capture tools hosted at The University of the Witwatersrand (Harris et al. 2009). The time to administer the PAVS questionnaire was taken from the electronic data capture timestamp at the start and end of the PAVS instrument. Statistical data analysis was conducted using SPSS 28.0 (IBM, Chicago, USA). For the measurements that were captured as continuous measures (age, years of education, systolic BP, diastolic BP, heart rate and physical activity), we reported the mean and the standard deviation. In accordance with World Health Organization physical activity guidelines, a participant was considered physically inactive if they did not report at least 150 min/week of moderate to vigorous physical activity (Bull et al. 2020).
Categorical variables (sex, years of education, medical history and lifestyle factors) were expressed as frequency and percentages. Hypertension was defined as a BP ≥ 140 mmHg systolic or ≥ 90 mmHg diastolic and/or currently taking anti-hypertensive medication according to the ISH guidelines (Unger et al. 2020). Physical activity was categorised into two groups: < 150 min/week and ≥ 150 min/week. Descriptive statistics were stratified both by gender and physical activity. Chi-square and independent T tests were performed to assess differences, respectively. Logistic regression was used to determine factors associated with physical activity. Univariate analysis and multiple logistic regression were fitted and results were reported as the odds ratio or adjusted odds ratio with the corresponding 95% confidence intervals and associated p values. The variables included in the multiple logistic regression were selected using step-wise variable selection and a liberal p value of 10%. The covariates considered in the multiple logistic regression were assessed for multicollinearity using the uncentred variance inflation factor (VIF). A mean VIF of 1.97 indicated that none of the covariates was collinear.
Results
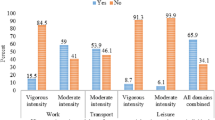
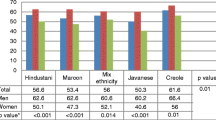
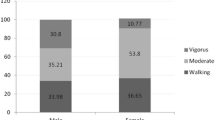
The final sample included 2282 participants, of which 50.9% were female (Table 1). The mean age of the total population was 43.3 ± 16.4 years. In the total population, 30.3% (n = 692) were classified as hypertensive. Median moderate-vigorous physical activity levels were 12, 6 and 24 min per week for the total sample, female and male participants, respectively (p = 0.0021 between males and females). Of the total population, female, and male participants, 19.8%, 17.6% and 22.1% reported ≥ 150 min/week of physical activity, respectively (p = 0.006 between males and females).
Table 2 presents characteristics of individuals categorised by physical activity status. The mean age of participants reporting ≥ 150 min/week of physical activity (42.7 years) did not differ significantly from those reporting < 150 min/week physical activity (44.2 years). More men reported ≥ 150 min/week physical activity than women (p = 0.006). Education levels were another significant predictor as individuals with > 12 years of education were significantly more likely to report achieving > 150 min/week of physical activity (p = 0.006). A greater proportion of individuals with hypertension reported < 150 min/week physical activity (31.5%) than reported ≥ 150 min/week physical activity (25.4%; p = 0.012).
In the univariate analysis (Table 3), significant positive associations were found between physical activity ≥ 150 min/week and male sex (odds ratio (OR) 1.33 (95%CI 1.08–1.64), p = 0.006); > 12 years of education (OR 1.74 (95%CI 1.04–2.94), p = 0.038); previous COVID diagnosis (OR 1.63 (95%CI 1.03–2.58), p = 0.036); COVID vaccination (OR 1.28 (95%CI 1.03–1.57), p = 0.022); alcohol consumption 1–6 times per week (OR 1.45 (95%CI 1.05–2.01), p = 0.023) and never consuming alcohol (OR 1.31 (95%CI 1.02–1.67) p = 0.037). A number of these relationships persisted in the adjusted analysis, including male sex (adjusted odd ratio (AOR) 1.58 (95%CI 1.25–2.01), p < 0.0001); previous COVID diagnosis (AOR 1.66 (95%CI 1.03–2.67), p = 0.039); COVID vaccination (AOR 1.29 (95%CI 1.03–1.59), p = 0.023); and alcohol consumption 1–6 times per week (AOR 1.41 (95%CI 1.01–1.96), p = 0.047). Significant negative associations were found between physical activity ≥ 150 min/week and hypertension (AOR 0.74 (95%CI 0.59–0.94), p = 0.038) and being a past smoker (AOR 0.62 (95%CI 0.46–0.84), p = 0.002). These relationships persisted in the adjusted analysis, hypertension (OR 0.77 (95%CI 0.61–0.97), p = 0.032) and being a past smoker (AOR 0.61 (95%CI 0.44–0.83), p = 0.002).
Discussion
In this study, we first examined the utility of screening for physical inactivity using the PAVS questionnaire administered by CHWs as a component of a home-based BP screening programme. We found that CHWs completed the PAVS questionnaire with participants in approximately 29.5 s, demonstrating the feasibility of using the tool as part of a larger screening assessment. We next explored the reported levels of physical activity and found that the overall percentage of the study population meeting physical activity guidelines was low but comparable with global trends (Guthold et al. 2018). Last, we examined associations between physical activity levels, socio-demographic characteristics and cardio-metabolic risk factors. We observed several significant associations between physical activity levels and cardiometabolic risk factors, such as hypertension, replicating previous findings involving the PAVS tool.
The PAVS tool meets several standards for healthcare screening tools, including that it is safe to administer, can be administered quickly and efficiently, and is cost-effective (Givler and Givler 2023), all of which are beneficial in low resource settings. All of the above characteristics highlight the PAVS as an ideal tool for mass community screenings, whether through home visits or at community events. When used as a basic screening tool, the PAVS identifies physically inactive individuals and starts a conversation about physical activity (Stoutenberg et al. 2017). The implementation of the PAVS tool in community settings allows CHWs to promptly identify and classify physical activity levels and inform referrals to appropriate interventions to promote physical activity and improve quality of life. Further, CHWs often live in or are from the communities which they serve, increasing the acceptability of home visits and increasing the reach of health services in under-resourced communities (Stoutenberg et al. 2023).
In South Africa, hypertension is a major contributor of NCDs and the leading cause of disability and death (Kandala et al. 2021). The prevalence of hypertension observed within the current study (30.2%) is in line with what has been previously reported in the May Measurement Month (MMM) South Africa screening in previous years (2017. 2018, and 2019) (Woodiwiss et al. 2021). Despite this, the 2019 MMM South Africa found that fewer than half of individuals with hypertension (42%) were aware of their condition (Woodiwiss et al. 2021). In this study, we found participants reporting physical activity ≥ 150 min/week were 23% less likely to be hypertensive, suggesting that PAVS may serve as an effective screening tool to identify those reporting physical activity below that of guidelines. Our findings of an inverse association between hypertension and physical activity ≥ 150 min/week correspond to those of Young et al., in an American population in which lower systolic and diastolic BPs were found in active compared to inactive women and lower diastolic BPs in active men than in inactive men assessed by exercise vital sign (Young et al. 2014).
The current study should be interpreted within the context of its strengths and limitations. The current study contributes to the limited evidence on the use of the PAVS questionnaire by CHWs in low resourced environments, demonstrating a minimal amount of time required to complete the survey as part of a larger community screening. The average time taken to complete the current PAVS questionnaire in this study demonstrates that it is a user-friendly and efficient screening tool. Furthermore, results from the PAVS are associated with several cardio-metabolic measures, highlighting the usefulness and efficiency of using the PAVS as an initial screening tool as a part of mass community screenings. The cross-sectional design limits the ability to determine causality between physical activity levels and health outcomes. A longitudinal or intervention study would provide stronger evidence. The PAVS questionnaire has some limitations as a self-report measure. Comparing it to an objective measurement of physical activity would strengthen validation. The lack of anthropometric measures is a limitation as they are often closely associated with physical activity and cardiometabolic risk. While various anthropometric measures (such as BMI) have been shown to serve as good markers of cardio-metabolic risk, we were unable to examine associations between PA levels and body weight/BMI, as reported in other investigations.
In conclusion, the PAVS should be considered as a viable tool for determining physical activity levels in underserved South African communities. This study demonstrated that the PAVS could be efficiently and effectively administered as a part of mass community screenings. Furthermore, activity levels assessed via the PAVS were associated with hypertension, further establishing the applicability of the tool. The study’s limitation is that it did not compare the results from the PAVS tool with an objective measurement of physical activity, which should be addressed in future research. However, this study provides initial evidence of the utility of incorporating the PAVS to determine physical activity levels in community health screenings, particularly in a low resource setting.
Data availability
The accessibility of data is constrained due to either ethical or privacy restrictions, thus rendering it inaccessible to the public.
References
Ajisegiri WS, Abimbola S, Tesema AG, Odusanya OO, Peiris D, Joshi R (2023) “We just have to help”: community health workers’ informal task-shifting and task-sharing practices for hypertension and diabetes care in Nigeria. Front Public Health 11:1038062. https://doi.org/10.3389/fpubh.2023.1038062
Bosire EN, Cohen E, Erzse A, Goldstein SJ, Hofman KJ, Norris SA (2020) “I’d say I’m fat, I’m not obese”: obesity normalisation in urban-poor South Africa. Public Health Nutr 23(9):1515–1526. https://doi.org/10.1017/s1368980019004440
Brady E, Castelli M, Walker R, Grayling M, Alaba O, Chola L (2022) The prevalence and social determinants of multimorbidity in South Africa. World Med Health Policy n/a (n/a). https://doi.org/10.1002/wmh3.557
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, Carty C, Chaput J-P, Chastin S, Chou R, Dempsey PC, DiPietro L, Ekelund U, Firth J, Friedenreich CM, Garcia L, Gichu M, Jago R, Katzmarzyk PT, Lambert E, Leitzmann M, Milton K, Ortega FB, Ranasinghe C, Stamatakis E, Tiedemann A, Troiano RP, van der Ploeg HP, Wari V, Willumsen JF (2020) World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 54(24):1451–1462. https://doi.org/10.1136/bjsports-2020-102955
Chu AHY, Ng SHX, Koh D, Müller-Riemenschneider F (2015) Reliability and validity of the self- and interviewer-administered versions of the Global Physical Activity Questionnaire (GPAQ). PLoS ONE 10(9):e0136944. https://doi.org/10.1371/journal.pone.0136944
Coleman KJ, Ngor E, Reynolds K, Quinn VP, Koebnick C, Young DR, Sternfeld B, Sallis RE (2012) Initial validation of an exercise “vital sign” in electronic medical records. Med Sci Sports Exerc 44(11):2071–2076. https://doi.org/10.1249/MSS.0b013e3182630ec1
Givler DN, Givler A (2023) Health screening. In: StatPearls. StatPearls, Treasure Island
Goudge J, de Kadt J, Babalola O, Muteba M, Tseng YH, Malatji H, Rwafa T, Nxumalo N, Levin J, Thorogood M, Daviaud E, Watkins J, Griffiths F (2020) Household coverage, quality and costs of care provided by community health worker teams and the determining factors: findings from a mixed methods study in South Africa. BMJ Open 10(8):e035578. https://doi.org/10.1136/bmjopen-2019-035578
Gradidge PJ-L, Crowther NJ, Chirwa ED, Norris SA, Micklesfield LK (2014) Patterns, levels and correlates of self-reported physical activity in urban black Soweto women. BMC Public Health 14(1):934. https://doi.org/10.1186/1471-2458-14-934
Grant RW, Schmittdiel JA, Neugebauer RS, Uratsu CS, Sternfeld B (2014) Exercise as a vital sign: a quasi-experimental analysis of a health system intervention to collect patient-reported exercise levels. J Gen Intern Med 29(2):341–348. https://doi.org/10.1007/s11606-013-2693-9
Greenwood JL, Joy EA, Stanford JB (2010) The physical activity vital sign: a primary care tool to guide counseling for obesity. J Phys Act Health 7(5):571–576. https://doi.org/10.1123/jpah.7.5.571
Guthold R, Stevens GA, Riley LM, Bull FC (2018) Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Health 6(10):e1077–e1086. https://doi.org/10.1016/s2214-109x(18)30357-7
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Hekler EB, Buman MP, Haskell WL, Conway TL, Cain KL, Sallis JF, Saelens BE, Frank LD, Kerr J, King AC (2012) Reliability and validity of CHAMPS self-reported sedentary-to-vigorous intensity physical activity in older adults. J Phys Act Health 9(2):225–236
Hopkins KL, Hlongwane KE, Otwombe K, Dietrich J, Cheyip M, Olivier J, van Rooyen H, Doherty T, Gray GE (2021) The substantial burden of non-communicable diseases and HIV-comorbidity amongst adults: screening results from an integrated HIV testing services clinic for adults in Soweto. South Africa Eclinicalmedicine 38:101015. https://doi.org/10.1016/j.eclinm.2021.101015
Joshi R, Alim M, Kengne AP, Jan S, Maulik PK, Peiris D, Patel AA (2014) Task shifting for non-communicable disease management in low and middle income countries–a systematic review. PLoS ONE 9(8):e103754. https://doi.org/10.1371/journal.pone.0103754
Kandala NB, Nnanatu CC, Dukhi N, Sewpaul R, Davids A, Reddy SP (2021) Mapping the burden of hypertension in South Africa: a comparative analysis of the national 2012 SANHANES and the 2016 demographic and health survey. Int J Environ Res Public Health 18 (10). https://doi.org/10.3390/ijerph18105445
Katzmarzyk PT, Friedenreich C, Shiroma EJ, Lee IM (2022) Physical inactivity and non-communicable disease burden in low-income, middle-income and high-income countries. Br J Sports Med 56(2):101. https://doi.org/10.1136/bjsports-2020-103640
Kohli-Lynch CN, Erzse A, Rayner B, Hofman KJ (2022) Hypertension in the South African public healthcare system: a cost-of-illness and burden of disease study. BMJ Open 12(2):e055621. https://doi.org/10.1136/bmjopen-2021-055621
Kowalski KC, Crocker PR, Donen RM (2004) The physical activity questionnaire for older children (PAQ-C) and adolescents (PAQ-A) manual, vol 87. College of Kinesiology, University of Saskatchewan, vol 1
Lewin S, Munabi‐Babigumira S, Glenton C, Daniels K, Bosch‐Capblanch X, van Wyk BE, Odgaard‐Jensen J, Johansen M, Aja GN, Zwarenstein M, et al. (2010) Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev (3). https://doi.org/10.1002/14651858.CD004015.pub3
McCarthy MM, Fletcher J, Heffron S, Szerencsy A, Mann D, Vorderstrasse A (2021) Implementing the physical activity vital sign in an academic preventive cardiology clinic. Prev Med Rep 23:101435. https://doi.org/10.1016/j.pmedr.2021.101435
Milton K, Gomersall SR, Schipperijn J (2023) Let’s get moving: the global status report on physical activity 2022 calls for urgent action. J Sport Health Sci 12(1):5–6. https://doi.org/10.1016/j.jshs.2022.12.006
Peer N, Uthman OA, Kengne A-P (2021) Rising prevalence, and improved but suboptimal management, of hypertension in South Africa: a comparison of two national surveys. Glob Epidemiol 3:100063. https://doi.org/10.1016/j.gloepi.2021.100063
Rawal LB, Kharel C, Yadav UN, Kanda K, Biswas T, Vandelanotte C, Baral S, Abdullah AS (2020) Community health workers for non-communicable disease prevention and control in Nepal: a qualitative study. BMJ Open 10(12):e040350. https://doi.org/10.1136/bmjopen-2020-040350
Stats SA (2012) Census 2011 statistical release. Statistics South Africa, Pretoria, South Africa
Stoutenberg M, Crouch SH, McNulty LK, Kolkenbeck-Ruh A, Torres G, Gradidge PJL, Ly A, Ware LJ (2023) Acceptability and feasibility of home-based hypertension and physical activity screening by community health workers in an under-resourced community in South Africa. Z Gesundh Wiss.https://doi.org/10.1007/s10389-023-01873-w
Stoutenberg M, Shaya GE, Feldman DI, Carroll JK (2017) Practical strategies for assessing patient physical activity levels in primary care. Mayo Clinic Proc: Innov Qual Outcomes 1(1):8–15. https://doi.org/10.1016/j.mayocpiqo.2017.04.006
Thomas LS, Buch E, Pillay Y (2021) An analysis of the services provided by community health workers within an urban district in South Africa: a key contribution towards universal access to care. Hum Resour Health 19(1):22. https://doi.org/10.1186/s12960-021-00565-4
Topolski TD, LoGerfo J, Patrick DL, Williams B, Walwick J, Patrick MB (2006) The Rapid Assessment of Physical Activity (RAPA) among older adults. Prev Chronic Dis 3(4):A118
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M, Wainford RD, Williams B, Schutte AE (2020) 2020 International society of hypertension global hypertension practice guidelines. Hypertension 75(6):1334–1357. https://doi.org/10.1161/hypertensionaha.120.15026
van Poppel MN, Chinapaw MJ, Mokkink LB, van Mechelen W, Terwee CB (2010) Physical activity questionnaires for adults: a systematic review of measurement properties. Sports Med 40(7):565–600. https://doi.org/10.2165/11531930-000000000-00000
Vancampfort D, Stubbs B, Probst M, De Hert M, Schuch FB, Mugisha J, Ward PB, Rosenbaum S (2016) Physical activity as a vital sign in patients with schizophrenia: evidence and clinical recommendations. Schizophr Res 170(2–3):336–340. https://doi.org/10.1016/j.schres.2016.01.001
Woodiwiss AJ, Gafane-Matemane LF, Norton GR, Uys L, Myburgh C, Nkeh-Chungag BN, Kruger L, Orchard A, Peterson VR, Kolkenbeck-Ruh A (2021) May measurement month 2019: an analysis of blood pressure screening results from South Africa. Eur Heart J Suppl 23 (Supplement_B):B134-B137
Woodiwiss AJ, Kruger R, Norton GR, Schutte AE, Myburgh C, Nkeh-Chungag B, Sewani-Rusike CR, Vally M, Jones E, Peterson V, Marsh J, Gafane-Matemane LF, Ahiante BO, Phalane E, Beaney T, Chis Ster A, Xia X, Poulter NR (2020) May measurement month 2018: an analysis of blood pressure screening results in South Africa. Eur Heart J Suppl 22(Suppl H):H115-h118. https://doi.org/10.1093/eurheartj/suaa043
Young DR, Coleman KJ, Ngor E, Reynolds K, Sidell M, Sallis RE (2014) Associations between physical activity and cardiometabolic risk factors assessed in a Southern California health care system, 2010–2012. Prev Chronic Dis 11:E219. https://doi.org/10.5888/pcd11.140196
Acknowledgements
The authors acknowledge the support of the Wits Health Hubb Health Advocates in the community health screening and the collection of this data.
Funding
Open access funding provided by University of the Witwatersrand. This study was supported by a strategic grant from the DSI-NRF Centre of Excellence in Human Development [STRATGNT2023-01], hosted by University of the Witwatersrand, Johannesburg. DPHRU is supported by the South African Medical Research Council. The Wits Health HUBB youth community health work training programme (https://www.witshealthhubb.org) is supported by Wits Health Consortium and through development funding from the Development Bank of Southern Africa. SHC is supported by the Joint Global Health Trials (UK). LJW is supported by the Wellcome Trust UK. PJG is supported by the South African National Research Foundation.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: study conception and design: PJG, GT, MS, and LJW; data collection and management: SHC and LGW; analysis and interpretation of results: ZMZ, SHC, PJG, GT, LJW, MS and MM; draft manuscript preparation: PJG, SHC, ZMZ, LJW, GT, MS and MM. Critical review of the manuscript: LJW, GT, LJW, MS, MM, AJW, JT and AK. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was obtained from the Human Research Ethics Committee (Medical) at the University of Witwatersrand [Ref. M200941 and M170334 renewed as M2203101].
Informed consent
All participants gave written informed consent prior to taking part in the study, those not wishing to participate in the study were still offered the same health screening services as participants.
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gradidge, P.JL., Crouch, S.H., Thornton, J. et al. Physical activity vital sign assessment and associated health outcomes in an underserved South African community. J Public Health (Berl.) (2024). https://doi.org/10.1007/s10389-024-02292-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-024-02292-1