Abstract
Aim
The increasing frequency of epidemic, climate, and political crisis situations, compounded by modern life stress, is associated with a rise in mental health problems. Unhealthy lifestyle, including unhealthy eating habits, insufficient sleep, and scarce physical activity, may further contribute to mental health problems, especially in young populations. The aim of the present longitudinal study is to examine the impact of eating habits, sleep, and physical activity on mental health problems during the COVID-19 pandemic as a crisis situation.
Subject and methods
We analyzed longitudinal self-report data collected at baseline (T1), 4 (T2), 8 (T3), and 12 months from 1029 participants aged 5 to 21 during the COVID-19 pandemic within the Corona Immunitas Ticino project.
Results
Repeated-measures ANOVA showed a significant decrease in mental health problems from T1 to T3, with a slight increase at T4. Hierarchical linear regression analysis revealed that a decrease in unhealthy eating habits together with an increase in physical activity from T1 to T4 were negatively correlated with mental health problems at T4. On the other hand, an increase in sleep time over the same study period was positively associated with mental health problems at T4. Among covariates, women and adolescents experienced more mental health problems.
Conclusion
The findings support previous research that highlights the role of a healthy lifestyle, including healthy eating and physical activity, in reducing mental health problems during difficult life circumstances exacerbated by crisis situations. Age- and gender-sensitive targeted interventions promoting healthy lifestyle behaviors are thus essential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The contemporary world is witnessing profound changes on various fronts. The rising frequency of epidemic outbreaks and climate crises (Ingle and Mikulewicz 2020), coupled with the volatile nature of political landscapes (2020), are shaping our collective experience through a series of interconnected challenges, including health problems, social inequalities, migration, population growth, environmental sustainability, and humanitarian crises. These multifaceted issues extend beyond their impact on physical well-being and significantly affect mental health. In recent years, there has been a growing recognition of how the convergence of these crises, combined with the stressors of modern life, has led to an increase in mental health problems, mostly among children and adolescents (Jenkins et al. 2011). Indeed, youth is a critical phase of development, characterized by substantial cognitive, emotional and physical changes that have implications for future mental health outcomes (Best and Ban 2021). Additionally, today’s children and adolescents will become tomorrow’s adults, and addressing mental health and well-being concerns during their youth is crucial to develop targeted public health strategies to foster a resilient society capable of effectively managing crisis situations in the future.
Let’s take the example of the COVID-19 pandemic, which has brought about unprecedented levels of stress, anxiety, and social isolation, especially among children and adolescents (Stavridou et al. 2020). These stressors are deemed to have long-lasting effects on mental health: Even after the pandemic, people may continue to struggle with the aftermath of the crisis (Mazza et al. 2022), particularly youth (Meherali et al. 2021). Furthermore, the changing climate patterns and escalating environmental crises pose significant challenges to human existence. The intensification of natural disasters, such as hurricanes, floods, and wildfires, has resulted in the displacement of communities, loss of livelihoods, and increased psychological distress (Cianconi et al. 2020). Climate change also brings forth additional mental health concerns, including eco-anxiety, a chronic fear and distress related to the impending environmental degradation and the future well-being of the planet (Ingle and Mikulewicz 2020). Such concerns are particularly prevalent in youth populations who will have to live with the long-term consequences of global warming (Lee et al. 2020). Moreover, economic and political crises as currently witnessed in the context of the Ukrainian war are complex events that can have profound implications for the mental health of those affected. During periods of economic instability, such as recessions or financial collapses, increased levels of stress, anxiety, and depression are observed among individuals experiencing job loss, debt, poverty, or financial uncertainty (Mucci et al. 2016). These factors can generate a sense of helplessness, despair, and social disintegration, fueling an unfavorable psychological climate which extends to children and adolescents who are either directly affected by their families’ economic instability (Frasquilho et al. 2016) and/or witnessing these problems at the societal level (Guerra and Eboreime 2021; Guerra et al. 2022). Similarly, political crises characterized by social tensions, conflicts or human rights violations can cause serious consequences on the mental health of those directly and indirectly affected (Puras and Gooding 2019). Trauma, constant fear, insecurity and the inability to freely express one’s opinions can lead to symptoms of anxiety, depression, post-traumatic stress disorder, and other mental health problems (Jenkins et al. 2011).
It is therefore crucial to understand how to promote mental health in children and adolescents. One approach is through the adoption of healthy lifestyle behaviors, which can be targeted with appropriate public health interventions to eventually mitigate the negative effects of crisis situations on young people’s mental health.
Lifestyle behaviors and mental health
Scientific evidence indicates that adopting a healthy lifestyle, including healthy dietary practices, physical exercise, and adequate sleep, can prevent physical ailments (Hu et al. 2011) and mental illnesses (Maenhout et al. 2020), while also promoting general well-being (Hosker et al. 2019; Wickham et al. 2020). In this study, we will analyze three lifestyle behaviors, i.e., nutrition, sleep, and physical activity, in correlation with mental health problems during the COVID-19 pandemic.
Nutrition is an essential aspect of maintaining good mental health. What we eat has a significant impact on our brain function and can have a profound effect on our mood, behavior, and cognitive abilities (Lachance and Ramsey 2015). Adequate nutrition is vital for the prevention and treatment of many mental health conditions, including depression, anxiety, schizophrenia, and bipolar disorder (Horn et al. 2022). Both cross-sectional and longitudinal studies have shown that a highly processed Western diet significantly increases the risk of developing mental disorders (Luppino et al. 2010; Coletro et al. 2022; Lane et al. 2022; Godos et al. 2023). In contrast, a healthy diet, including fruits and vegetables, whole grains, unsaturated fats, low-fat, and plant-based protein, protects against the development of a mental disorder (Owen and Corfe 2017). Moreover, it is not just about what we eat but also how. Eating regularly and avoiding skipping meals or fasting for extended periods can help regulate blood sugar levels, which eventually impact mood and behavior (Penckofer et al. 2012). Healthy eating may be heavily jeopardized by crisis situations such as the COVID-19 pandemic. Studies have evidenced that nutrition has deteriorated in both the quality (what) of the food chosen and the habits (how). During the pandemic, there was a greater consumption of sweets, processed foods and alcohol compared to before the pandemic (Segre et al. 2021; Czenczek-Lewandowska et al. 2021; González-Monroy et al. 2021). In addition to this, there was a shift toward modified eating behavior, characterized by more frequent snacking and irregular eating (Segre et al. 2021). Related to incorrect eating patterns that can lead to serious problems, the prevalence of eating disorders in Europe has increased by an average of 30% (Tavolacci et al. 2021; Sideli et al. 2021; Haddad 2022).
In addition to nutrition, sleep is a crucial aspect of maintaining good mental health (Scott et al. 2021). Several studies have shown that sleep deprivation and poor sleep quality can increase the risk of developing mental health conditions such as depression, anxiety, and bipolar disorder (Benca et al. 1992; Baglioni et al. 2011; Ghrouz et al. 2019; Scott et al. 2021). During sleep, the brain processes and consolidates information, which is essential for learning, memory, and emotional regulation. Lack of sleep can impact cognitive processes, such as attention, concentration, and decision-making abilities, which can negatively impact mental health (Kim et al. 2022). Sleep also plays a crucial role in regulating the emotional state. It helps process emotions and respond appropriately to stressful situations. Poor sleep quality can lead to increased irritability, anxiety, and mood swings (Qiu and Morales-Muñoz 2022). During the pandemic, sleep quality deteriorated (Czenczek-Lewandowska et al. 2021). Although there has generally been no change in sleep hours (Zhao et al. 2023), the quality was worse as sleep was often fragmented either during the day rather than during the night, leading to a disruption of the circadian rhythm (Ferreira-Souza et al. 2023). In addition to this, sleep disturbances, including poor sleep quality and insomnia, increased significantly during the pandemic (Jahrami et al. 2023; Uccella et al. 2023).
Physical activity is important for promoting mental health and more general well-being. Physical activity can help reduce symptoms of anxiety and depression, improve mood (Anderson and Shivakumar 2013), and enhance overall cognitive function (Reigal et al. 2020). Exercise also stimulates the release of endorphins, which can contribute to a sense of happiness and relaxation (Harber and Sutton 1984). Moreover, participating in physical activities provides opportunities for social interaction and engagement, fostering a sense of belonging and support (Bean et al. 2014). During the early phases of the COVID-19 pandemic, physical activity was heavily undermined by strict social distancing measures to contain the spread of the SARS-CoV-2 virus in the population. In many countries, including Switzerland, school and extra-curricular sports activities were interrupted, and outdoor activities forbidden to avoid contacts outside one’s own household (Bundesrat (BAG) 2020; Michelini et al. 2021; Pfefferbaum 2021). This led to a decrease in physical activity and an increase in sedentary behavior, including screen time, among children and adolescents (Peralta et al. 2022).
Study aim
The present study aims to examine the impact of nutrition, sleep, and physical activity on mental health in children and adolescents during the COVID-19 pandemic as an exemplary crisis situation. More precisely, we will analyze the change in these lifestyle behaviors as the pandemic evolved and the associations of this change with mental health outcomes, while also considering sociodemographic characteristics. Our study findings have the potential to inform public health policies and interventions aimed at mitigating the negative impact of future pandemics and similar crisis situations on the mental health of these vulnerable populations.
Methods
Participant recruitment and data collection
In the present study, we analyzed longitudinal data of children and adolescents collected within the Corona Immunitas Ticino (CIT) project between September 2020 and November 2021. CIT was a population-based prospective cohort study that investigated both the seroprevalence of SARS-CoV-2 and the impact of the COVID-19 pandemic on physical and mental health and lifestyle in the general population of the Canton of Ticino, in Italian-speaking Switzerland. CIT was part of a larger network of seroprevalence and impact studies conducted throughout Switzerland and across different age populations. The common aims, characteristics, and implications of these studies have been previously described by West et al. (2020). In August 2020, a representative sample of 4264 children and adolescents from Canton Ticino was invited to participate in CIT. Invited participants were allowed to nominate up to five household members, which led to the inclusion of 188 additional participants up to 19 years of age. For ethical, legal, and practical reasons, people not fluent in Italian, under guardianship, in an asylum procedure, or with a short-term residency permit (i.e., < 1 year) were excluded from the study. Of all invited, 1063 provided informed consent to participate in the study. For children aged 5 to 13 years, parents provided responses related to the invited child. For adolescents aged 14 to 19 years, survey responses were based on self-report. Upon study enrolment between September and November 2020, participants received a baseline questionnaire (T1), which solicited responses regarding their lifestyle behaviors at three time points, i.e., before, during, and after the initial COVID-19 lockdown period (March to May 2020). Subsequently, participants received regular follow-up questionnaires measuring lifestyle behaviors and mental health outcomes as the pandemic evolved. Questionnaires were administered digitally via email. A reminder was sent after approximately one week for each follow-up assessment. For the present study, we also considered the responses collected at three additional time points, i.e., at 4 (T2), 8 (T3), and 12 months (T4) after study enrolment.
Measures
For this study, we considered measures of mental health, lifestyle behaviors, and sociodemographics. Mental health was conceptualized as mental health problems. For the sake of consistency, and to facilitate the interpretation of our results, all lifestyle measures were considered in positive terms, i.e., absence of unhealthy eating habits, adequate sleep, and sufficient physical activity. This required recoding some of the lifestyle measures as explained in more detail hereafter. Notably, while lifestyle behaviors were assessed with reference to six time points (i.e., before, during, and after initial lockdown as well as at 4, 8, and 12 months from baseline assessment), retrospective questions regarding mental health problems prior to and during the initial lockdown between March and May 2020 were not assessed in the CIT project, as such questions could not be reliably answered retrospectively.
Mental health problems
Mental health problems were measured at all four assessment points (T1, T2, T3, T4) with 15 questions taken from the DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure (Clarke and Kuhl 2014) and then adapted respectively to the two age cohorts. The DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure is a widely used tool to assess a broad range of psycho-somatic symptoms. It is considered a reliable and valid instrument for measuring mental health and well-being (Bastiaens and Galus 2018). The adaptation of the tool for this study aimed to capture specific aspects of mental health problems relevant to the COVID-19 pandemic and its related social distancing measures (Ma et al. 2021). Items were measured on a scale from 1 (never) to 5 (almost every day). The average of the 15 responses was then taken, with higher values indicating a higher frequency of mental health problems.
Nutrition
Participants were asked to report how many days in a week, on average, they ate irregularly, e.g., by skipping a meal, overeating, or eating at inappropriate times such as at night. These eating habits were measured on a scale ranging from 0 (never) to 7 (every day). For the present study, the measure was recoded so that higher values indicated less frequent unhealthy eating habits.
Sleep
Two questions were included to evaluate participants’ sleep patterns: one related to the number of hours slept on weekdays and the other related to the number of hours slept on weekend days. Responses were collected on a continuous scale ranging from 0 to 24 h per day. Subsequently, an average was calculated from the hours slept during a weekday and during a weekend day with higher values indicating longer sleep time.
Physical activity
Physical activity was measured by asking study participants how much time, on average, during a week they engaged in moderate to vigorous physical activity, i.e., with at least light sweating. Items were measured on a scale from 0 to 168 h per week. Thus, higher values indicate more physical activity time.
Sociodemographics and BMI
Five sociodemographic characteristics were considered as covariates in the present study. They were all assessed once at T1 (baseline questionnaire) and dummy coded for further analysis. Gender was coded as 0 (male) and 1 (female). Age was coded as 0 (children aged 5–13) and 1 (adolescents aged 14–19). Family income was coded as 0 (more than enough to live) and 1 (just or not enough to live). Parents’ education was coded as 0 (some post obligatory education, including professional school or university) and 1 (only compulsory schooling). Nationality was coded in 0 (Swiss) and 1 (non-Swiss). Participants with double nationality were coded as 0 if one of the nationalities included Swiss. Moreover, we calculated participants body mass index (BMI) by dividing reported body weight in kilograms by height in meters squared. We used the WHO macro that generates age-specific z-scores (de Onis et al. 2007). The measures of family income, parents’ education, nationality, body weight and height included the answer options “I don’t know” and “I prefer not to answer”. These responses were considered as missing values.
Analytical plan
The survey responses were automatically captured in a web application for creating and managing online surveys called REDCap (Harris et al. 2009) and securely stored on servers of the host university. Once the data collection period was over, the data were exported from the survey platform to the statistical program SPSS version 26 for further analysis.
Outliers were identified across all variables by visual inspection of data using box plots and scatter plots. In addition, the distribution of each variable was assessed for normality using skewness and kurtosis values. Observations with a skewness greater than ± 3.5 and a kurtosis greater than ± 7.0 (Byrne 2010) were flagged as potential outliers. Once potential outliers were identified, further investigation was conducted to determine whether they were valid data points or errors. This involved a thorough review of original survey responses to ensure data accuracy and checking for any data entry errors. The sample size was adjusted by excluding the outliers according to the variables used in the ANOVA and regression analysis described hereafter.
Several missing data were observed in the study, with an increase in missingness over time. The reasons for missing data could be related to several factors, such as participant dropout due to lack of interest, inability to continue with the study due to health or personal circumstances, or technical difficulties that prevented participants from completing the measures at specific time points, despite study reminders. In addition, participants may have been less likely to complete the measures as the study progressed due to a deterioration in their health, which they wanted to avoid admitting and therefore preferred not to answer. To deal with these missing values, the expectation–maximization (EM) imputation method was used, an iterative method that estimates missing values by maximizing the likelihood of the observed data. EM imputation provides flexible and unbiased estimates, utilizes all available information, considers relationships among variables, and can handle various missing data mechanisms. This method was only used for the questions on mental health problems, nutrition, sleep and physical activity, where the missingness increased over time (range T1 0.5–2.5%, T2 20.1–29.0%, T3 46.1–49%, T4 58.1–67.4%). EM was not used for imputing missing data for sociodemographics and BMI measured at baseline, where missing values ranged between 0.6% and 11.3%.
Subsequently, for each lifestyle behavior, the difference (delta Δ) between T1 and T4 was calculated by subtracting T1 from T4 scores. A positive delta value indicates an increase in the frequency of the lifestyle behavior, while a negative value indicates a decrease. By calculating a delta, we considered changes in nutrition, sleep, and physical activity levels over the entire study period. Thus, we did not focus on a single time but on variation. Furthermore, this procedure led to a reduction in the dependence on initial measurements: everyone has different habits and consequently different subjective starting values, which are taken into account by means of the delta.
During preliminary analysis, a repeated-measures analysis of variance (ANOVA) with gender and age as interaction variables was performed to explore the evolution of all three lifestyle behaviors (before the pandemic to T4) and mental health problems (T1 to T4) over time (before pandemic—T4). Furthermore, a bivariate correlation matrix was created to explore the relationships between mental health problems at T1 and T4, the change in lifestyle behaviors between T1 and T4 (i.e., Δnutrition, Δsleep, Δphysical activity), and covariates (age, gender, BMI, parents’ education, family income, nationality) at T1.
For the main analysis, a hierarchical linear regression analysis was performed to assess the relationship between the changes in lifestyle behaviors between T1 and T4 (i.e., Δnutrition, Δsleep, Δphysical activity) and mental health problems at time 4. Three different models were constructed sequentially. Model 1 included only the covariates as predictors. Model 2 expanded upon model 1 by adding mental health problems at T1 as a predictor to consider autoregressive effects. Model 3 included the variations between the three lifestyle behaviors (Δ(T4–T1)), along with the covariates and mental health problems at T1. By using this hierarchical approach, the study aimed to evaluate the unique contribution of each added block in explaining mental health problems over time.
Results
Sample characteristics
A total of 1063 children (parent-report) and adolescents (self-report) answered the baseline questionnaire. From these, 16 participants were excluded because they had chronic physical or mental illnesses and 14 participants were eliminated because they did not indicate their gender and age, which was necessary to characterize them (sociodemographic characteristics were not imputed). In addition, four outlier cases were removed from the dataset. These outliners were removed because they had values that corresponded to the responses to sleep disturbances and unhealthy eating habits that were impossible. The final analytical sample was composed of 1029 participants (male n = 496 (48.2%); female n = 533; (51.8%)). Age ranged from 5 to 21 years old, with a median of 13 years. A total of 527 participants belong to the child cohort (5–13 years) and 502 to the adolescent cohort (14–21 years). Regarding the level of parents’ education, 67.5% attended a college or university, 26.8% had compulsory education, and 5.6% preferred not to answer. As far as family income is concerned, 86.2% reported to have enough to live, 2.5% reported to have just or not enough to live, and the remaining 11.3% preferred not to answer. Concerning nationality, 86.2% of the participants were Swiss, 13.2% had a non-Swiss nationality, and 0.6% preferred not to answer. The mean BMI was 18.82 kg/m2, the median 18.42 kg/m2 (range from 10.75 kg/m2 to 46.99 kg/m2). Furthermore, in order to satisfy the assumption of normality required for conducting the statistical tests, six outliers were excluded from the linear regression analysis (n = 1023), and an additional 28 outliers were excluded for the repeated measures ANOVA (n = 995).
Preliminary results
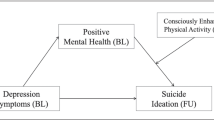
One-way repeated-measures ANOVA with gender and age cohort as interaction variables revealed that mental health problems decreased between T1 and T3, with a slight increase at T4, though. The variation over time was significant (Wilks’ Lambda = 0.85, F(3955) = 60.26, p < 0.001). The analysis revealed a significant interaction between time and gender for mental health problems (F(2995) = 36.65, p < 0.001). Across time, women had higher values of mental health problems compared to men. The interaction effect of age cohort was also significant (F(2955) = 198.22, p < 0.001), implying that adolescents had more mental health problems compared to children. Concerning lifestyle behaviors, the one-way repeated measures ANOVA revealed an increase in unhealthy eating habits from the pre-pandemic period to the lockdown between March and May 2020. After lockdown, the average number of days per week of unhealthy eating habits decreased again, though remained slightly higher compared to before the COVID-19 pandemic. The variation over time was significant (Wilks’ Lambda = 0.84, F(3955) = 50.24, p < 0.001), which was primarily due to the increase from the pre-lockdown to the lockdown period. The interaction with gender (F(2955) = 26.70, p < 0.001) and age cohort (F(2955) = 259.33, p < 0.001) was significant, indicating that men and children showed less frequently unhealthy eating habits than women and adolescents. The average number of hours slept increased during the initial COVID-19 lockdown between March and May 2020, with a steady decrease over the following pandemic year. The variation over time was significant (Wilks’ Lambda = 0.74, F(3955) = 70.56, p < 0.001), which was, once again, mainly due to the increase in sleep time from the pre-lockdown to the lockdown period. Significant interaction effects were also observed for both gender (F(2955) = 5.54, p = 0.019) and age cohort (F(2955) = 580.78, p < 0.001). Men showed slightly less often unhealthy eating habits than women, while children show considerably less often unhealthy eating habits than adolescents. The average number of hours of physical activity per week dropped by almost two hours during the lockdown between March and May 2020. With the loosening of strict containment measures in autumn 2020, they almost completely changed back to pre-lockdown measures, ranging between four and almost five hours. The variation over time was significant (Wilks’ Lambda = 0.77, F(3955) = 87.40, p < 0.001), primarily due to the stark drop during lockdown. The interaction effect with gender was significant (F(2955) = 12.39, p < 0.001), meaning that men tended to spend more time with physical activity than women. Eventually, the interaction with age cohort was also significant (F(2955) = 5.07, p = 0.025). Children spent more time engaging in physical activity compared to adolescents. Figure 1 shows the results of the repeated measures ANOVA for mental health problems and all three lifestyle behaviors, on the left side with gender and on the right side with age as the between group variable. More detailed information on means and standard deviations are available in the Supplement, Tables 1–4. Information about tests of between-subjects effects for mental health problems, nutrition, sleep, and physical activity with gender and age as between groups (n = 955) are also available in the Supplement, Tables 5–8. Additionally, precise information about missing values can be found in the Supplement, Tables 9–10.
Repeated measures ANOVA with gender (left) and age (right) as between group variables (n = 955). Note: before = before the pandemic, during = during initial lockdown between March and May 2020, T1 at baseline in autumn 2020, T2 at 4 months follow-up, T3 at 8 months follow-up, T4 at 12 months follow-up
Table 1 summarizes the Pearson’s correlation coefficients for bivariate associations between all study variables. Mental health problems at T1 and T4 were significantly and positively associated with being female, belonging to the adolescent age group, and a greater BMI. In addition, BMI was significantly and negatively associated with an increase in healthy eating habits and an increase in physical activity over the course of the pandemic, but not with an increase in sleep. In other words, as the pandemic evolved, participants with a greater BMI engaged less frequently in healthy eating habits and in physical activity compared to children and participants with a lower BMI. Moreover, being an adolescent was negatively associated with physical activity.
Hierarchical regression results
Three different regression models were constructed sequentially to discover the additional predictive value of the change in lifestyle behaviors from T1 to T4 on mental health problems at T4, controlling for sociodemographic characteristics and BMI as covariates and autoregressive effects of mental health at T1. The first model with only covariates as predictors explained 15.2% of the variance in mental health problems at T4. Adding the measure of mental health problems at T1, the second model explained 52.0% of the variance in the outcome variable. The third and final model, with the addition of changes in eating habits, sleep and physical activity over time (ΔT4–T1), explained 54.6% of the variance. All three models were statistically significant.
Table 2 summarizes the results of the three regression models, including the overall F-statistics and R-square change. In model 1, mental health problems at T4 were significantly predicted by being an adolescent (β = 0.338, p < 0.001) and female (β = 0.130, p < 0.001). Adding mental health problems at T1 decreased the predictive value of age (β = 0.180, p < 0.001) and gender (β = 0.055, p = 0.22), though both remained significant predictors. Furthermore, mental health problems at T1 significantly and positively predicted mental health problems at T4 (β = 0.647, p < 0.001). The third model including lifestyle behaviors shows that a change in nutrition (β = –0.118, p < 0.001) and physical activity (β = –0.102, p < 0.001) from T1 to T4 were negatively correlated with mental health problems at T4. In other words, children and adolescents who engaged less in unhealthy eating habits and spent more time with physical activity over the course of the pandemic year under consideration presented significantly lower levels of mental health problems at 12 months of assessment. At the same time, an increase in sleep duration was associated with significantly higher levels of mental health problems (β = 0.065, p = 0.006), Significant predictors in model 1 and 2 (i.e., gender, age, and mental health problems at T1) remained significant predictors in model 3 (gender β = 0.055, p = 0.020; age β = 0.176, p < 0.001; mental health problems at T1: β = 0.639, p < 0.001).
Discussion
The aim of this study was to investigate the influence of changes in three lifestyle behaviors, i.e., nutrition, sleep and physical activity, on mental health problems among children and adolescents during crisis situations such as the COVID-19 pandemic. To this end, we analyzed data collected longitudinally during 2020 and 2021 in Canton Ticino, Italian-speaking Switzerland, as part of the Corona Immunitas Ticino project. To the best of our knowledge, no longitudinal study to date has looked at these three lifestyle behaviors together, how these lifestyle behaviors and mental health changed over a time of more or less stringent confinement measures, and what impact the change in lifestyle behaviors had on mental health at the outset of the pandemic in a particularly vulnerable population such as children and adolescents.
Our study has four main findings: First, there were evident variations in mental health as well as the three investigated lifestyle behaviors as the pandemic evolved. We found a steady improvement in mental health among children and adolescents during the year following the initial COVID-19 lockdown between March and May 2020, despite a slight worsening at final assessment. These results align with previous studies showing that mental health improved after strict lockdown measures have been loosened and the roll-out of the vaccination campaign reduced the fear in the population of a severe course of the disease if infected (Bourmistrova et al. 2022; Wester et al. 2022). The slight worsening at 12 months follow-up (i.e., in autumn 2021) could suggest that the initial positive effects of public health strategies on the mental health of children and adolescents may not have been sustained over time and that additional support or interventions may be necessary to maintain or improve mental health outcomes (Meherali et al. 2021). Similar to mental health, all three examined lifestyle variables showed an evident change, especially when comparing the time before, during, and right after the strict lockdown between March and May 2020. During the lockdown, we observed a significant worsening of eating habits and a marked decrease in physical activity, alongside an increase in sleep time. These findings align with the results of systematic reviews (Dalekou et al. 2023; Zhao et al. 2023; Bozzola et al. 2023) and can be explained by the heavy impact of strict confinement measures put in place by public health authorities at the onset of the pandemic, which led to school closures, the interruption of extracurricular sports activities, and the need to organize a healthy routine at home. For many parents of children and adolescents, this was a major challenge as they had to balance childcare, domestic and work activities (Fadda et al. 2023; Blázquez-Fernández et al. 2023). The consequences were that children and adolescents were oftentimes left to themselves but did not yet have the means to effectively structure their day and care for themselves. After the initial lockdown, values tended to return to pre-pandemic levels. However, unhealthy eating habits and sleep set at moderately higher values compared to the pre-pandemic period, while physical activity returned to the same values. It is important to note though, that lifestyle behaviors before the pandemic and during the initial lockdown were assessed retrospectively. Thus, they may be subject to a recall bias (Cross et al. 2021).
Second, our study revealed that a change in all three examined lifestyle behaviors over the course of the pandemic was significantly associated with mental health problems at 12 months follow-up. More precisely, a decrease in unhealthy eating habits was related to better mental health outcomes as has also been shown in a systematic review that identified a significant relationship between unhealthy eating patterns and poorer mental health, especially depressive problems, in young people (Lassale et al. 2019; Coletro et al. 2022; Godos et al. 2023). Eating habits directly impact various biological systems and mechanisms underlying depression, including oxidative processes, immune system functioning and salient brain protein levels (O’Neil et al. 2014; Burnatowska et al. 2022). For example, regular meal consumption and sufficient chewing time reduce depression levels among girls (Sangouni et al. 2022). Although the topic is not widely investigated and further research is needed, the association between healthy eating and reduced mental problems is well established; therefore, intervening through the promotion of healthy nutrition is a valuable strategy to improve mental health in young people in times of a crisis (Wang et al. 2022). Furthermore, an increase in physical activity over the course of the COVID-19 pandemic was associated with less mental health problems at 12 months follow-up. Physical activity can help reduce stress, anxiety, and depressive symptoms due to the release of endorphins (Marconcin et al. 2022). In addition, regular physical activity can help improve cognitive functions, including attention, memory, learning, and executive skills (Mandolesi et al. 2018). Last but not least, physical activity, especially as part of extracurricular sports activities, is a moment of recreation and exchange and, after a particular period of crisis, where social contacts were reduced to a minimum, physical activity can be an efficient means to resume young people’s social life (Amati et al. 2018). Thus, physical activity integrated within a healthy lifestyle framework that encourages movement, enjoyment, and social engagement can help avoid mental health problems in children and adolescents during a crisis such as the COVID-19 pandemic. Concerning sleep, we found that an increase in sleep time over the course of the pandemic was associated with increased mental health problems at 12 months follow-up. This result may seem contradictory, but it is not. Too much sleep might be both a symptom and predictor of mental health problems. This has been amply demonstrated by systematic reviews and meta-analyses: adequate sleep (not oversleeping) is a protective factor for several mental health problems, particularly depression, anxiety, and mood disorders (Arora et al. 2022). The difference between quality and quantity of sleep is also very important. In the CIT project, the repeated surveys assessed how many hours children and adolescents slept on an average weekday and weekend day. However, reported sleep duration is not necessarily associated with good sleep quality (Scott et al. 2021), which should be integrated in future studies investigating the impact of sleep on mental health during a crisis situation.
Our third main results regard the autoregressive effect of mental health problems. Specifically, mental health problems assessed during autumn 2020 positively and significantly predicted mental health problems one year later. In other words, those children and adolescents who reported mental health problems were more likely to report these problems even after the COVID-19 pandemic in Italian-speaking Switzerland was almost over and life back to normal. Similar to our finding, a systematic review, analyzing the effect of the pandemic on mental health, concluded that the initial presence of a psychiatric problem is one of the major risk factors associated with psychological distress (Bourmistrova et al. 2022). One of the reasons is the lack of internal (i.e., resilience) and external (i.e., support) resources to manage stressful life situations exacerbated by a crisis such as a pandemic. It is therefore crucial that particularly vulnerable children and adolescents have access to the resources needed to manage their everyday life and mental health problems (Agbaria and Mokh 2022; Chin et al. 2023).
Fourth and last, among sociodemographic characteristics and BMI as covariates, we found that age and gender had a significant effect on mental health: Women and adolescents presented significantly worse mental health over the course of the pandemic compared to men and children. Women experience more frequently internalizing problems such as mental health issues, especially depression and anxiety (Tibubos et al. 2021). In contrast, men show more frequently externalizing problems such as substance abuse (Otten et al. 2021). Concerning the age effect, it is well-established that adolescence is a period of life that is characterized by significant changes, both physical and psychological, which puts this age group at greater risk of developing mental health problems (National Academies Press (US) 2019). As adolescents navigate the challenges of puberty and social development, they experience a range of emotions and behaviors that may be difficult to manage. Studies have shown that depression, anxiety, and other mental health issues increase during adolescence (Racine et al. 2021). This may be partly due to the hormonal changes that occur during puberty (Pfeifer and Allen 2021), as well as the stresses associated with school, family, and peer relationships. During crisis situations, where, among others, social contacts are potentially undermined, adolescents are more at risk of experiencing mental health problems and thus particularly need support and resources to manage these crisis situations.
Strengths and limitations
The current study has some limitations that should be considered when interpreting the study’s findings, and future studies should address these issues to provide more reliable and generalizable results. First, although the data stem from a prospective cohort study, our analyses focused on the association of changes in lifestyle behaviors and mental health problems. Future studies with larger samples and robust measures could further investigate reciprocal causality between all three lifestyle behaviors and mental health problems at the individual (i.e., within-person) level. Second, the sample size and sample attrition over time, requiring the imputation of missing data, might have affected the generalizability of the study findings. Future prospective cohort studies should make a concerted effort to increase the initial sample size and keep participation high, with a special focus on adolescents who are most likely to lose interest in study participation. Third, even small changes of lifestyle behaviors and mental health problems over a one-year time period during the COVID-19 pandemic might have been confounded by seasonal effects. It is thus not possible to fully relate lifestyle behaviors and mental health outcomes to the progress of the pandemic alone. Quasi-experimental studies may overcome this issue but are difficult to implement in worldwide crisis situations such as the COVID-19 pandemic. Fourth and last, lifestyle behaviors were assessed by combining different aspects of these behaviors (e.g., skipping meals and overeating) or by focusing on one aspect (e.g., sleep duration but not sleep quality). The use of single item and indicators and one-sided assessments of constructs of interest is common in large-scale studies with multiple research objectives, and more in-depth studies are needed to overcome this limitation.
However, it is also important to mention the strengths of the study. The longitudinal study design allows for sequential observation of the same participants while keeping the subjective variables constant. This is an important aspect of the study, as it provides a detailed and comprehensive understanding of the evolution of lifestyle behaviors and mental health problems over a prolonged period. Additionally, the study analyzed data from children and adolescents, which are particularly difficult to obtain over time and during a crisis situation given the practical challenges researchers have to face in recruitment and data collection involving these populations. Furthermore, the sample was heterogeneous because young people were randomly selected from the entire Ticino region, and there were no over-represented categories in terms of socio-demographic data such as gender, parental education, income, and nationality. This diversity in the sample enhances the generalizability of the study findings and makes it more representative of the wider population.
Conclusion and practical implications
In conclusion, the present study highlights the important role of lifestyle behaviors for mental health in children and adolescents during times of a crisis. Among lifestyle behaviors, a decrease in unhealthy eating habits and an increase in physical activity were found to be the main factors protecting from mental health problems. It is therefore critical that public health authorities and other relevant stakeholders take early action to promote these lifestyle behaviors and assure that they are maintained among young people. This should include health promotion activities addressed toward children and adolescents, e.g., through school-based interventions, and toward parents as important role models and decision makers, e.g., through targeted communication strategies in collaboration with parent organizations. In addition, awareness campaigns on (social) media can reach a wider audience to promote a healthy lifestyle. More precisely, public health authorities should collaborate with the media, nonprofit organizations, and advertising agencies to create campaigns that highlight the importance of mental health and promote a healthy lifestyle. These campaigns can spread positive messages, provide information about available resources, and encourage open dialogue about mental health. These promotion measures can eventually help reduce mental health problems in children and adolescents during crisis situations, especially considering that such crisis situations are likely in the future. In addition, more longitudinal as well as (quasi-)experimental research should be funded to deepen the understanding of the role of lifestyle behaviors for mental health and to identify specific effective intervention strategies. In addition, it is important to implement continuous population monitoring to assess the effectiveness of policies and initiatives that are already in place, allowing for constant adaptation and improvement. Ultimately, a future perspective based on an approach to mental health through the promotion of a healthy lifestyle can help mitigate the negative effects of crisis situations on young people’s mental health, and eventually contribute to a better quality of life and lasting well-being.
Availability of data and material
The dataset and additional material are available on the OSF platform: (https://osf.io/abux3/).
Code availability
Not applicable.
References
Agbaria Q, Mokh AA (2022) Personal and social resources in coping with coronavirus crisis among Israeli-Palestinian adults: explanatory study. Int J Ment Health Addict 20:1595. https://doi.org/10.1007/s11469-020-00465-z
Amati V, Meggiolaro S, Rivellini G, Zaccarin S (2018) Social relations and life satisfaction: the role of friends. Genus 74:7. https://doi.org/10.1186/s41118-018-0032-z
Anderson E, Shivakumar G (2013) Effects of exercise and physical activity on anxiety. Front Psychiat 4:27. https://doi.org/10.3389/fpsyt.2013.00027
Arora T, Grey I, Östlundh L et al (2022) A systematic review and meta-analysis to assess the relationship between sleep duration/quality, mental toughness and resilience amongst healthy individuals. Sleep Med Rev 62:101593. https://doi.org/10.1016/j.smrv.2022.101593
Baglioni C, Battagliese G, Feige B et al (2011) Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord 135:10–19. https://doi.org/10.1016/j.jad.2011.01.011
Bastiaens L, Galus J (2018) The DSM-5 self-rated level 1 cross-cutting symptom measure as a screening tool. Psychiatr Q 89:111–115. https://doi.org/10.1007/s11126-017-9518-7
Bean CN, Fortier M, Post C, Chima K (2014) Understanding how organized youth sport may be harming individual players within the family unit: a literature review. Int J Environ Res Public Health 11:10226–10268. https://doi.org/10.3390/ijerph111010226
Benca RM, Obermeyer WH, Thisted RA, Gillin JC (1992) Sleep and psychiatric disorders. A meta-analysis. Arch Gen Psychiat 49:651–668; discussion 669–670. https://doi.org/10.1001/archpsyc.1992.01820080059010
Best O, Ban S (2021) Adolescence: physical changes and neurological development. Br J Nurs Mark Allen Publ 30:272–275. https://doi.org/10.12968/bjon.2021.30.5.272
Blázquez-Fernández C, Lanza-León P, Cantarero-Prieto D (2023) A systematic review on suicide because of social isolation/and loneliness: does COVID-19 make a difference? J Public Health Oxf Engl fdad001. https://doi.org/10.1093/pubmed/fdad001
Bourmistrova NW, Solomon T, Braude P et al (2022) Long-term effects of COVID-19 on mental health: a systematic review. J Affect Disord 299:118–125. https://doi.org/10.1016/j.jad.2021.11.031
Bozzola E, Barni S, Ficari A, Villani A (2023) Physical activity in the COVID-19 Era and its impact on adolescents’ well-being. Int J Environ Res Public Health 20:3275. https://doi.org/10.3390/ijerph20043275
Bundesrat (BAG) (2020) Coronavirus: Bundesrat erklärt die «ausserordentliche Lage» und verschärft die Massnahmen. https://www.admin.ch/gov/de/start/dokumentation/medienmitteilungen.msg-id-78454.html. Accessed 13 Jun 2023
Burnatowska E, Surma S, Olszanecka-Glinianowicz M (2022) Relationship between mental health and emotional eating during the COVID-19 pandemic: a systematic review. Nutrients 14:3989. https://doi.org/10.3390/nu14193989
Byrne BM (2010) Structural equation modeling with amos: basic concepts, applications, and programming, 2nd edn. Taylor and Francis Group, New York
Chin J, Di Maio J, Weeraratne T et al (2023) Resilience in adolescence during the COVID-19 crisis in Canada. BMC Public Health 23:1097. https://doi.org/10.1186/s12889-023-15813-6
Cianconi P, Betrò S, Janiri L (2020) The impact of climate change on mental health: a systematic descriptive review. Front Psychiat 11
Clarke DE, Kuhl EA (2014) DSM-5 cross-cutting symptom measures: a step towards the future of psychiatric care? World Psychiatry 13:314–316. https://doi.org/10.1002/wps.20154
Coletro HN, de Mendonça R, D, Meireles AL, et al (2022) Ultra-processed and fresh food consumption and symptoms of anxiety and depression during the COVID - 19 pandemic: COVID Inconfidentes. Clin Nutr ESPEN 47:206–214. https://doi.org/10.1016/j.clnesp.2021.12.013
Cross TJ, Isautier JMJ, Stamatakis E, et al (2021) Self-reported physical activity before a COVID-19 ‘lockdown’: is it just a matter of opinion? BMJ open sport — Exerc Med 7:e001088. https://doi.org/10.1136/bmjsem-2021-001088
Czenczek-Lewandowska E, Wyszyńska J, Leszczak J et al (2021) Health behaviours of young adults during the outbreak of the Covid-19 pandemic - a longitudinal study. BMC Public Health 21:1038. https://doi.org/10.1186/s12889-021-11140-w
Dalekou S, Michaleas SN, Tsitsika AK, Karamanou M (2023) Comparative study of pandemics and their impact on children and adolescents: COVID-19 and Spanish Flu. Infez Med 31:131–139. https://doi.org/10.53854/liim-3102-1
de Onis M, Onyango AW, Borghi E et al (2007) Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 85:660–667. https://doi.org/10.2471/blt.07.043497
Fadda M, Melotto M, Caiata-Zufferey M et al (2023) Joys or sorrows of parenting during the COVID-19 lockdown: a scoping review. Public Health Rev 43:1605263. https://doi.org/10.3389/phrs.2022.1605263
Ferreira-Souza LF, Julianelli-Peçanha M, Coelho-Oliveira AC et al (2023) Impacts of COVID-19 pandemic on sleep quality evaluated by Wrist Actigraphy: a systematic review. J Clin Med 12:1182. https://doi.org/10.3390/jcm12031182
Frasquilho D, Matos MG, Salonna F et al (2016) Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health 16:115. https://doi.org/10.1186/s12889-016-2720-y
Ghrouz AK, Noohu MM, Dilshad Manzar M et al (2019) Physical activity and sleep quality in relation to mental health among college students. Sleep Breath Schlaf Atm 23:627–634. https://doi.org/10.1007/s11325-019-01780-z
Godos J, Bonaccio M, Al-Qahtani WH et al (2023) Ultra-processed food consumption and depressive symptoms in a mediterranean cohort. Nutrients 15:504. https://doi.org/10.3390/nu15030504
González-Monroy C, Gómez-Gómez I, Olarte-Sánchez CM, Motrico E (2021) Eating behaviour changes during the COVID-19 pandemic: a systematic review of longitudinal studies. Int J Environ Res Public Health 18:11130. https://doi.org/10.3390/ijerph182111130
Guerra O, Eboreime E (2021) The impact of economic recessions on depression, anxiety, and trauma-related disorders and illness outcomes—a scoping review. Behav Sci 11:119. https://doi.org/10.3390/bs11090119
Guerra O, Agyapong VIO, Nkire N (2022) A qualitative scoping review of the impacts of economic recessions on mental health: implications for practice and policy. Int J Environ Res Public Health 19:5937. https://doi.org/10.3390/ijerph19105937
Haddad J (2022) The impact of the COVID‐19 pandemic on eating disorders: Anorexia nervosa, bulimia nervosa and Binge-Eating. Bern
Haileamlak A (2022) Pandemics will be more frequent. Ethiop J Health Sci 32:228. https://doi.org/10.4314/ejhs.v32i2.1
Harber VJ, Sutton JR (1984) Endorphins and exercise. Sports Med 1:154–171. https://doi.org/10.2165/00007256-198401020-00004
Harris PA, Taylor R, Thielke R et al (2009) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Horn J, Mayer DE, Chen S, Mayer EA (2022) Role of diet and its effects on the gut microbiome in the pathophysiology of mental disorders. Transl Psychiatry 12:1–13. https://doi.org/10.1038/s41398-022-01922-0
Hosker DK, Elkins RM, Potter MP (2019) Promoting mental health and wellness in youth through physical activity, nutrition, and sleep. Child Adolesc Psychiatr Clin N Am 28:171–193. https://doi.org/10.1016/j.chc.2018.11.010
Hu FB, Liu Y, Willett WC (2011) Preventing chronic diseases by promoting healthy diet and lifestyle: public policy implications for China. Obes Rev off J Int Assoc Study Obes 12:552–559. https://doi.org/10.1111/j.1467-789X.2011.00863.x
Ingle HE, Mikulewicz M (2020) Mental health and climate change: tackling invisible injustice. Lancet Planet Health 4:e128–e130. https://doi.org/10.1016/S2542-5196(20)30081-4
Jahrami H, BaHammam AS, Bragazzi NL et al (2023) Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med 17:299–313. https://doi.org/10.5664/jcsm.8930
Jenkins R, Baingana F, Ahmad R et al (2011) Social, economic, human rights and political challenges to global mental health. Ment Health Fam Med 8:87
Kim T, Kim S, Kang J et al (2022) The common effects of sleep deprivation on human long-term memory and cognitive control processes. Front Neurosci 16:883848. https://doi.org/10.3389/fnins.2022.883848
Lachance L, Ramsey D (2015) Food, Mood, and brain health: implications for the modern clinician. Mo Med 112:111–115
Lane MM, Gamage E, Travica N et al (2022) Ultra-processed food consumption and mental health: a systematic review and meta-analysis of observational studies. Nutrients 14:2568. https://doi.org/10.3390/nu14132568
Lassale C, Batty GD, Baghdadli A et al (2019) Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatry 24:965–986. https://doi.org/10.1038/s41380-018-0237-8
Lee K, Gjersoe N, O’Neill S, Barnett J (2020) Youth perceptions of climate change: a narrative synthesis. Wires Clim Change 11:e641. https://doi.org/10.1002/wcc.641
Luppino FS, de Wit LM, Bouvy PF et al (2010) Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 67:220–229. https://doi.org/10.1001/archgenpsychiatry.2010.2
Ma S-J, Wang W-J, Tang M et al (2021) Evaluation of the construct reliability and validity of the DSM-5 self-rated level 1 cross-cutting symptom measure-Chinese version in maintenance hemodialysis patients. J Int Med Res 49:03000605211012661. https://doi.org/10.1177/03000605211012661
Maenhout L, Peuters C, Cardon G et al (2020) The association of healthy lifestyle behaviors with mental health indicators among adolescents of different family affluence in Belgium. BMC Public Health 20:958. https://doi.org/10.1186/s12889-020-09102-9
Mandolesi L, Polverino A, Montuori S et al (2018) Effects of physical exercise on cognitive functioning and wellbeing: biological and psychological benefits. Front Psychol 9:509. https://doi.org/10.3389/fpsyg.2018.00509
Marconcin P, Werneck AO, Peralta M et al (2022) The association between physical activity and mental health during the first year of the COVID-19 pandemic: a systematic review. BMC Public Health 22:209. https://doi.org/10.1186/s12889-022-12590-6
Mazza C, Ricci E, Colasanti M et al (2022) How has COVID-19 affected mental health and lifestyle behaviors after 2 years? The third step of a longitudinal study of Italian citizens. Int J Environ Res Public Health 20:759. https://doi.org/10.3390/ijerph20010759
Meherali S, Punjani N, Louie-Poon S et al (2021) Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int J Environ Res Public Health 18:3432. https://doi.org/10.3390/ijerph18073432
Michelini E, Bortoletto N, Porrovecchio A (2021) Outdoor physical activity during the first wave of the COVID-19 pandemic. A comparative analysis of government restrictions in Italy, France, and Germany. Front Public Health 9. https://doi.org/10.3389/fpubh.2021.615745
Mucci N, Giorgi G, Roncaioli M et al (2016) The correlation between stress and economic crisis: a systematic review. Neuropsychiatr Dis Treat 12:983–993. https://doi.org/10.2147/NDT.S98525
National Academies Press (US) (2019) The promise of adolescence: realizing opportunity for all youth. National Academies Press (US), Washington (DC)
O’Neil A, Quirk SE, Housden S et al (2014) Relationship between diet and mental health in children and adolescents: a systematic review. Am J Public Health 104:e31–e42. https://doi.org/10.2105/AJPH.2014.302110
Otten D, Tibubos AN, Schomerus G et al (2021) Similarities and differences of mental health in women and men: a systematic review of findings in three large German cohorts. Front Public Health 9:553071. https://doi.org/10.3389/fpubh.2021.553071
Owen L, Corfe B (2017) The role of diet and nutrition on mental health and wellbeing. Proc Nutr Soc 76:425–426. https://doi.org/10.1017/S0029665117001057
Penckofer S, Quinn L, Byrn M et al (2012) Does glycemic variability impact mood and quality of life? Diabetes Technol Ther 14:303–310. https://doi.org/10.1089/dia.2011.0191
Peralta GP, Camerini A-L, Haile SR et al (2022) Lifestyle behaviours of children and adolescents during the first two waves of the COVID-19 pandemic in Switzerland and their relation to well-being: an observational study. Int J Public Health 67:1604978. https://doi.org/10.3389/ijph.2022.1604978
Pfefferbaum B (2021) Challenges for child mental health raised by school closure and home confinement during the COVID-19 pandemic. Curr Psychiatry Rep 23:65. https://doi.org/10.1007/s11920-021-01279-z
Pfeifer JH, Allen NB (2021) Puberty initiates cascading relationships between neurodevelopmental, social, and internalizing processes across adolescence. Biol Psychiatry 89:99–108. https://doi.org/10.1016/j.biopsych.2020.09.002
Puras D, Gooding P (2019) Mental health and human rights in the 21st century. World Psychiatry 18:42–43. https://doi.org/10.1002/wps.20599
Qiu J, Morales-Muñoz I (2022) Associations between sleep and mental health in adolescents: results from the UK millennium cohort study. Int J Environ Res Public Health 19:1868. https://doi.org/10.3390/ijerph19031868
Racine N, McArthur BA, Cooke JE et al (2021) Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr 175:1142–1150. https://doi.org/10.1001/jamapediatrics.2021.2482
Reigal RE, Moral-Campillo L, de Mier RJ-R et al (2020) Physical fitness level is related to attention and concentration in adolescents. Front Psychol 11:110. https://doi.org/10.3389/fpsyg.2020.00110
Sangouni AA, Beigrezaei S, Akbarian S et al (2022) Association between dietary behaviors and depression in adolescent girls. BMC Public Health 22:1169. https://doi.org/10.1186/s12889-022-13584-0
Scott AJ, Webb TL, Martyn-St James M et al (2021) Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials. Sleep Med Rev 60:101556. https://doi.org/10.1016/j.smrv.2021.101556
Segre G, Campi R, Scarpellini F et al (2021) Interviewing children: the impact of the COVID-19 quarantine on children’s perceived psychological distress and changes in routine. BMC Pediatr 21:231. https://doi.org/10.1186/s12887-021-02704-1
Sideli L, Lo Coco G, Bonfanti RC et al (2021) Effects of COVID-19 lockdown on eating disorders and obesity: a systematic review and meta-analysis. Eur Eat Disord Rev J Eat Disord Assoc 29:826–841. https://doi.org/10.1002/erv.2861
Stavridou A, Stergiopoulou A, Panagouli E et al (2020) Psychosocial consequences of COVID-19 in children, adolescents and young adults: a systematic review. Psychiatry Clin Neurosci 74:615–616. https://doi.org/10.1111/pcn.13134
Tavolacci M-P, Ladner J, Déchelotte P (2021) Sharp increase in eating disorders among university students since the COVID-19 pandemic. Nutrients 13:3415. https://doi.org/10.3390/nu13103415
The Global Economy (2020) Available at https://www.theglobaleconomy.com/compare-countries/. Accessed 21 May 2023
Tibubos AN, Otten D, Ernst M, Beutel ME (2021) A systematic review on sex- and gender-sensitive research in public mental health during the first wave of the COVID-19 Crisis. Front Psychiatry 12:712492. https://doi.org/10.3389/fpsyt.2021.712492
Uccella S, Cordani R, Salfi F et al (2023) Sleep deprivation and insomnia in adolescence: implications for mental health. Brain Sci 13:569. https://doi.org/10.3390/brainsci13040569
Wang Y, Liu J, Compher C, Kral TVE (2022) Associations between dietary intake, diet quality and depressive symptoms in youth: a systematic review of observational studies. Health Promot Perspect 12:249–265. https://doi.org/10.34172/hpp.2022.32
West EA, Anker D, Amati R et al (2020) Corona immunitas: study protocol of a nationwide program of SARS-CoV-2 seroprevalence and seroepidemiologic studies in Switzerland. Int J Public Health 65:1529–1548. https://doi.org/10.1007/s00038-020-01494-0
Wester CT, Bovil T, Scheel-Hincke LL et al (2022) Longitudinal changes in mental health following the COVID-19 lockdown: results from the survey of health, ageing, and retirement in Europe. Ann Epidemiol 74:21–30. https://doi.org/10.1016/j.annepidem.2022.05.010
Wickham S-R, Amarasekara NA, Bartonicek A, Conner TS (2020) The big three health behaviors and mental health and well-being among young adults: a cross-sectional investigation of sleep, exercise, and diet. Front Psychol 11. https://doi.org/10.3389/fpsyg.2020.579205
Zhao Z, Li L, Sang Y (2023) The COVID-19 pandemic increased poor lifestyles and worsen mental health: a systematic review. Am J Transl Res 15:3060–3066
Acknowledgements
We acknowledge the “Corona Immunitas Ticino” study group: Emiliano Albanese, Rebecca Amati, Antonio Amendola, Anna Maria Annoni, Granit Baqaj, Kleona Bezani, Peter Buttaroni, Anne-Linda Camerini, Anna Paola Caminada, Elia Cattani, Alessandro Ceschi, Laurie Corna, Cristina Corti Fragoso, Luca Crivelli, Diana Sofia Da Costa Santos, Giorgio Dal Bo’, Gladys Delai Venturelli, Daniela Dordoni, Marta Fadda, Luca Faillace, Ilaria Falvo, Paolo Ferrari, Maddalena Fiordelli, Carolina Foglia, Giovanni Franscella, Sara Gamberoni, Roberta Gandolfi, Rosita Ghidossi, Daniele Giottonini, Paola Guglielmetti, Sandra Jovic, Franco Keller, Sara Levati, Isabella Martinelli, Federico Mele, Rosalba Morese, Anna Papis, Giovanni Piumatti, Greta Rizzi, Serena Sabatini, Federica Sallusto, Tatiana Terrot, and Mauro Tonolla. We thank all participants of “Corona Immunitas Ticino” for their essential contribution and the Swiss Federal Statistical Office for providing the randomized list of participants. This study would not have been possible without the collaboration of Ente Ospedaliero Cantonale, Institute of Microbiology SUPSI, Centro Medico, Centre Hospitalier Universitaire Vaudois, Institute for Research in Biomedicine, Uniti Health Services, Fondazione Sasso Corbaro, Tre Valli Soccorso, BeeCare, GIIPSI, Hannelore Pieroni Sagl, Protezione Civile, Corpo Pompieri Faido, Associazione Ridere per Vivere, and Migros Ticino. We are grateful for the invaluable work of all the collaborators, site investigators, and interviewers of Università della Svizzera italiana (USI) and University of Applied Sciences and Arts of Southern Switzerland (SUPSI). We also thank the Swiss School of Public Health and the Ceresio Foundation for their support in funding this project.
Funding
Open access funding provided by Università della Svizzera italiana The study was funded by Corona Immunitas, a public–private partnership supported by the Federal Office of Public Health, various cantons, companies, and private individuals in Switzerland.
Author information
Authors and Affiliations
Consortia
Contributions
Giovanna Pedroni: Methodology, Writing – Original draft preparation; Anne-Linda Camerini: Conceptualization, Methodology, Writing – Reviewing and Editing.
Corresponding author
Ethics declarations
Ethics approval
Corona Immunitas Ticino was approved by the Cantonal Ethics Committee of Ticino (BASEC 2020–01247) on 23 June 2020.
Consent to participate
The study participants provided informed consent prior to their participation in the study.
Consent for publication
Not applicable.
Conflicts of interest
The authors declare that they have no conflict of interest. The funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Membership of the Group/Team Name is provided in the Acknowledgments.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pedroni, G., Camerini, AL. & on behalf of the Corona Immunitas Ticino Study Group. The importance of a healthy lifestyle to prevent mental health problems during crisis situations: evidence from Corona Immunitas Ticino. J Public Health (Berl.) (2024). https://doi.org/10.1007/s10389-024-02263-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-024-02263-6