Abstract
Aims
Language barriers significantly contribute to limited access and treatment quality in diabetic health care for ethnic minority groups. The study assesses the extent of linguistic resources and barriers in outpatient diabetes care in Germany.
Subject and methods
The questionnaire-based explorative cross-sectional study included all certified outpatient diabetological practices in Germany (N = 169), assessing, among other things, medical professionals’ (MP) language competencies, language barriers in treatment, use of and attitudes towards professional interpreters.
Results
One hundred and seven practices (63%) participated in the study, with an average of 16 MPs employed; of these, 47.2% spoke at least one other language than German, with 35.2% using their multilingual competencies actively for treating patients. Of all patients, 6.3% had German language skills which were insufficient for treatment situations, with this variable significantly predicted by the MPs’ multilingual treatment offers; 95.4% of the interpreter-assisted situations were supported by family members/friends. Among the clinicians, 86.0% appreciated a better participation for the patient being enabled by professional interpreters. The use of a professional interpreter in consultations was predicted by prior experience in working with interpreters.
Conclusion
The low proportion of patients with limited language proficiency suggests numerous barriers for patients to enter the outpatient diabetes care system. The multilingual capabilities among MPs do not cover the patients´ linguistic needs. Though MPs agree that professional interpreters are a good way to overcome language barriers, this study highlights obstacles that hinder clinicians from relying on professional interpreters.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
An estimated 537 million people worldwide are living with diabetes, and this number is predicted to rise to 643 million during the next 10 years (IDF 2021). Diabetes is a chronic disease, associated with acute as well as long-term complications and responsible for approximately 6.7 million deaths globally (IDF 2021), thus constituting a high burden for the health care system (Meetoo 2014). Studies show higher diabetes prevalences among migrants compared to their host population (Barnett et al. 2006; Kirk et al. 2006; Meeks et al. 2016), especially for migrants living in industrialized Western societies (Agyemang et al. 2006; Jenum et al. 2005; Uitewaal et al. 2004; Ujcic-Voortman et al. 2009).
However, ethnic minority groups have to face multiple access barriers to health care services (Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care 2003). Disparities in health and health care complicate the diagnosis and treatment process of diabetes in migrants (Cefalu and Golden 2005; Chow et al. 2012), resulting in, for exampe, higher rates of diabetes complications (Harris 2001).
Among other factors, language barriers contribute to this by hindering successful patient–clinician communication (Ali and Watson 2018; Kale and Syed 2010; Steinberg et al. 2016). They are associated with an increased risk of adverse medication reactions, reduced patient adherence, and limited understanding of the diagnosis and diabetes education (Karliner et al. 2007; Okrainec et al. 2015; Sohal et al. 2015; Wilson et al. 2005), which, in turn, has been shown to be a barrier to successful diabetes self-management (Nam et al. 2011). Furthermore, limited language proficiency has a proven negative effect on migrant patients’ glycemic control (American Diabetes Association 2019; Fernandez et al. 2011), whereas switching from a language-discordant to a language-concordant clinician has a significant positive effect on glycemic control among patients with limited language proficiency (Parker et al. 2017).
Though addressing language barriers is closely related to an improved performance of clinical care providers (American Diabetes Association 2019), not all practitioners make use of existing linguistic resources in outpatient care (Mösko et al. 2013). Although the use of professional medical interpreters proves superior to non-professionals such as relatives or friends (Karliner et al. 2007; Schenker et al. 2011), they are often underused in health care (Kale and Syed 2010) due to, among other factors, lack of access and lack of funding resources (Mayo et al. 2016).
In Germany, one-fourth of the population has a migration background, with 24.3% (20.2. million) people having their own migration history (Destatis 2023). The number is rising annually, thus making the provision of multilingual treatment options increasingly important. The aim of this study was to investigate the extent of existing linguistic resources and barriers in outpatient diabetes care, and also the clinicians’ attitude towards working with professional interpreters.
Methods
In order to evaluate multilingualism in outpatient diabetes care and to measure clinicians’ perception towards using professional interpreters, a cross-sectional study was conducted using a questionnaire developed by the authors (see Supplementary information).
Questionnaire development
As no appropriate scientifically sound instrument was found to measure the variables of interest, a new questionnaire was developed. Previous studies with a similar scope and the instruments they used served as a basis (Gogolin et al. 2017; Mösko et al 2013). Based on the results of a literature research, the items were developed by the author team and validated by three external experts.
The questionnaire contained 30 items and was divided into six sections, recording information on: a) the clinicians’ practice, b) language competencies of the clinical staff, c) language barriers in treatment, d) the use of professional interpreters, including attitudes towards them, using a 5-point Likert scale, e) needs for further training and materials, and f) general comments.
The scale measuring attitudes towards the work with interpreters (d) consisted of 12 items and was psychometrically tested. The Kaiser–Meyer–Olkin criterion was 0.777 and the Bartlett test for sphericity showed a highly significant result (p < 0.001) which permitted the conducting of a principal component analysis with varimax rotation. The number of selected factors was determined on the basis of the Kaiser–Guttmann criterion (eigenvalues > 1). The factor analysis extracted four factors, which explained 65.6% of the total variance. Since the extracted factors were heterogeneous in content, a meaningful interpretation was not possible. Further assessments were conducted instead on a single-item basis. The internal consistency of the scale (Cronbach's α = 0.799) was in an acceptable range.
Participants
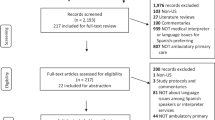
All certified outpatient diabetological practices in Germany are openly published on the website of the German Diabetes Society (n = 175). Out of this list, six practices had to be withdrawn from the list as in two cases the clinician had retired, in two cases the practice was part of a joint practice, and two cases were duplicates within the list. All remaining 169 practice owners were contacted.
Data acquisition
Data collection took place between September and December 2018. The questionnaire was sent to all identified heads of the practices by mail, including a cover letter, a stamped return envelope and a small incentive (candy). A reminder letter was sent after 4 weeks, accompanied by a reminder e-mail by the German Diabetes Society and one contact by phone.
Data evaluation
The collected data was analysed using the Statistical Package for the Social Sciences (SPSS, version 25.0). To ensure the quality of the analysis, data entry was randomly controlled by two auditors, both internal and external. A plausibility analysis was conducted.
For descriptive analyses, percentage frequencies, means, and standard deviations were calculated. Associations between different variables were calculated with Pearson correlation coefficients. A multiple linear regression analysis was computed for analyzing the predictive effect of MPs active offer of multilingual patient care, and its active advertisement on the treatment of patients with limited language skills. Logistic regression analyses were used to test for variables influencing the clinicians’ support of training for working with interpreters (predictors: MPs actively offering multilingual patient care, previous experience in working with interpreters, and patients’ limited language skills) as well as the use of professional interpreters (predictors: prior participation in a training program on how to work with professional interpreters, previous experience in working with interpreters, knowing how to contact professional interpreters, and MPs actively offering multilingual patient care). The effects of clinicians’ previous experiences in working with interpreters on their attitudes towards working with interpreters were investigated by conducting non-parametric Mann–Whitney U-tests, as prerequisites of normal distribution and homogeneity of variance were partly violated. All analyses were conducted at a significance level of p = 0.05 and, when necessary, Bonferroni–Holm-corrected.
Results
Sample
Data collection was closed with a response rate of 63.3%, with n = 107 practices participating in the study. Each practice had on average 1.741 patients with diabetes mellitus on file (SD = 855) and an average of 16 medical professionals (MPs), including all primary-care providers such as doctors, nurses, and any other clinical staff (SD = 8.5); 91.6% (n = 98) of the practices reported to primarily treat adults, 8.4% (n = 9) treated adults, adolescents, and children.
Linguistic resources among MPs
On average, 47.2% (n = 7.3, SD = 5.8) MPs per practice spoke at least one other language than the official language German, covering 29 languages in total. Most frequently mentioned were English (78.5%, n = 84), Turkish (43.9%, n = 47), French (27.1%, n = 29), Russian (23.4%, n = 25) and Polish (19.6%, n = 21). One third (35.2%, n = 5.3, SD = 4.3) of MPs reported that they actively used their multilingual skills in patient care. On average, each practice had linguistic resources that were actively used, covering almost three languages (mean = 2.63, SD = 1.75). Of those practices that reported to have at least one MP that actively uses multilingual skills in patient care (n = 98), only 31.6% (n = 32) publicly advertised this additional treatment offer.
Multilingual patient information
The vast majority of the practices (88.8%, n = 95) display multilingual patient information. Most commonly, this patient information is published in Turkish (55.1%, n = 52), Russian (50.0%, n = 48), English (41.1%, n = 39), Arabic (41.1%, n = 39) and Spanish (5.6%, n = 5).
Language barriers in treatment
On average, the clinicians indicated that 6.3% of their patients (n = 113) did not have sufficient German language skills for adequate diagnosis or treatment in the last quarter; 19.6% of clinicians reported to have had to reject treatment due to language barriers within the last quarter (n = 21).
In cases where communication with a patient was not possible, 92.5% (n = 99) of the clinicians reported tthat they had used external help such as family members, friends, or acquaintances interpreting, or a professionally trained interpreter to facilitate communication with a patient within the last quarter. In those cases, family and friends were almost always consulted (95.4%) compared to professional interpreters (4.6%). The average number of times an ad-hoc interpreter got involved during a treatment was 62.1, whereas the average number of times a professional interpreter was consulted was 2.8. Associations between linguistic resources among MPs, patients’ limited language skills and interpreter uses were calculated using the Pearson correlation coefficient (Table 1). Significant correlations were found between MPs’ linguistic resources, patients’ limited language skills, and the use of family/friends as interpreters: the more MPs proved multilinguistic skills and actively used them, the more patients with limited language skills were treated and the more often family members and friends functioned as interpreters. Active advertisement of multilingual treatment offers was associated with more patients with limited language skills as well as with more refusals of patients due to language barriers. Use of professional interpreters was not associated with any of the factors studied.
A multiple linear regression analysis [F (2,86) = 9.647, p < 0.001; R2 = 0.183] showed a significant influence of MPs' active offer of multilingual treatment on the number of patients with limited language skills (β = 0.436, p < 0.001), while the effect of its advertisement stayed insignificant (β = -−0.042, p = 0.674).
Working with professional interpreters
Eighty-one of the clinicians (75.7%) reported to have worked with a professional interpreter before. Thirty-five clinicians (32.7%) knew how to get in contact with them; 96 (94.1%) stated they would involve professional interpreters more often if the costs were covered by health insurances. Asked for their preferences, 94.2% (n = 98) would prefer on-site cooperation with interpreters, 4.0% (n = 5) video interpreting, and 1.0% (n = 1) phone-calls with the interpreter. Table 2 provides an overview of the clinicians’ attitudes towards working with professional interpreters.
Mann–Whitney U-tests were conducted for measuring for differences in attitudes between clinicians who had prior experiences with interpreters and those who had not (Table 3). Before Bonferroni–Holm correction, clinicians showed higher agreement on item 2 (“When a language barrier is present, the involvement of professional interpreters is the best way to ensure successful treatment outcome.”; z = -−2.261; p = 0.024). After Bonferroni–Holm correction, the difference stayed insignificant. The comparisons for all other items showed insignificant results.
The computation of a logistic regression analysis to search for factors predicting the clinicians’ use of professional interpreters yielded the following results. The overall model was significant: χ2 (4) = 24.532, p < 0.001 with –2LL = 105.16. The use of professional interpreters was significantly predicted by prior experience in working with them (p < 0.001). All results are shown in Table 4.
Training needs
Sixty-one (58.7%) of the clinicians rated the general offer of advanced training for working with professional interpreters as helpful. Nine (8.5%) had already participated in such training.
A logistic analysis revealed that neither the clinicians’ prior experience in working with an interpreter, nor MPs' multilingual treatment resources and the number of patients treated with limited language skills had a significant influence on the perceived training need: χ2 (3) = 3.608, p = 0.307.
Discussion
This study examined language barriers in diabetes treatment in Germany, and identified existing linguistic resources among MPs. Furthermore, clinicians’ use of and attitudes towards working with professional interpreters were assessed. We were able to achieve a response rate of 63.3%, this being slightly higher than the average response rates to mail surveys of physicians (Asch et al. 1997).
Encountering language barriers
The clinicians in the survey estimated that more than 6% of their patients do not possess sufficient language skills for adequate treatment. However, other studies in German outpatient oncological and psychiatric care reported an percentage of patients with limited German proficiency more than double the size (12.3%) (Mösko et al. 2018). According to the nationwide socio-economic panel, 15% of the migrants in Germany have “rather poor” or “no” German language skills even after 11 years of residence in Germany (Liebau and Romiti 2014).
As prevalence of type 2 diabetes is higher for ethnic minorities compared to the host country population (Meeks et al. 2016), the small numbers of patients with limited German proficiency found in this study most probably do not reflect the real amount of this target group. It is rather likely that a certain percentage of patients simply do not enter the outpatient diabetes care system due to numerous barriers (Titus and Kataoka-Yahiro 2019).
Almost one fifth of the clinicians reported that they had to reject patients due to language barriers within the last quarter. What happened with these patients and whether they were able to receive adequate treatment somewhere else still remains unclear.
Overcoming language barriers
Almost half of the MPs in the sample indicated that they were multilingual and spoke at least one other language than German. However, only one third used their skills actively when interacting with patients, and only one third of the practices actually advertised their language skills. As language concordance has an impact on quality of care and treatment outcomes for patients with limited proficiency in the official language (Diamond et al. 2019), future research should investigate this phenomenon of linguistic resources being left unused.
Overall, 29 languages were covered by the MPs in the nationwide sample, indicating a somewhat diverse spectrum. The representation of languages partly coincides with the representation of immigrant groups within the general German population in 2020, people with Turkish nationality being the biggest group, followed by people with Polish nationality (Destatis 2020). This fits with our finding that the number of MPs who actively used their multilingual skills significantly predicted the amount of patients with limited language skills that had been treated. However, while people with Syrian nationality were the third biggest immigrant group in Germany, Arabic was not among the most frequently mentioned languages used in patient care. As found in other outpatient settings (Mösko et al. 2013), the MPs’ language resources are one important factor for treating patients with limited language skills and might cover the patients’ linguistic need to certain extends, but are insufficient to cover all patients’ linguistic needs.
Using professional interpreters
This study confirms the common tendency of using ad-hoc interpreters such as family members and friends instead of professional interpreters in medical settings (Schenker et al. 2011). The number of patients with limited language skills was significantly associated with the use of ad-hoc interpreters but not with the use of professional ones. Given the administrative effort required for involving professional interpreters, this seems somewhat understandable; the majority of clinicians agreed that they would involve professional interpreters more often if coverage of costs was clearly regulated. Although three quarters stated that they had worked with a professional interpreter before, only one third knew how to get into contact with them. Besides underlining the clinicians’ predominant use of non-professional interpreters, this might indicate that frequently either the patients or third parties are the ones reaching out to professional interpreters. Whether this stems from a lack of information or responsibility on the MPs’ side or a deficit in the availability of professional interpreters remains unanswered.
However, as several studies have shown the translation quality to be significantly improved when using professional interpreters, and the risks of translation errors with potential medical consequences to be increased when relying on ad-hoc interpreters such as family and friends (Flores et al. 2012), fundamental changes in language interpretation practices in outpatient diabetes care in Germany are indispensible.
Attitudes towards professional interpreters
Although the majority of clinicians agreed that professional interpreters are the best way to overcome language barriers, this study highlights several obstacles that seem to hinder clinicians from actually relying on professional interpreters. Structural and financial issues in employing interpreters pose a known obstacle for clinicians, as in Germany the provision of interpreters is not covered by health insurances, so the costs have to be covered by the clinician or the patient. However, even if access or finances were more clearly regulated, almost one fourth of clinicians in our study would still refuse to work with an interpreter. A large body of clinicians indicated that interpreters would hinder the establishment of trust with the patient or would complicate their workflow. There might be various reasons explaining the clinicians’ hesitation to work with interpreters. This study proved that previous experience in working with a professional interpreter increases clinicians’ probability of doing so in the future as well, which is also supported by other studies (Bachmann, Mohwinkel & Mösko [in prep]). In a study among psychotherapists, Gartner and colleagues 2024 found out that participants without any experience in working with interpreters mentioned insecurities concerning the triadic situation. Although the comparison between clinicians’ attitudes towards the work with an interpreter, depending on their prior experiences, stayed insignificant in our sample after Bonferroni–Holm correction, there were descriptive differences, nevertheless, indicating more positive attitudes in clinicians with prior experiences in working with an interpreter. However, the questionnaire developed for this study did not differentiate the quality and quantity of the clinicians’ experience, which might be an explanation for the lack of significance. In addition, there are studies that have shown cultural racism to exist in health care services on an individual as well as an institutional level (Doran and Lawson 2021). As we did not include measures on xenophobic tendencies and/or attitudes, we cannot make a statement about their influence on clinicians’ hesitation towards the treatment of patients with limited language skills and the inclusion of professional interpreters. Therefore, future studies should further investigate the underlying issues that might explain this defensive attitude.
A majority of the sample welcomed the offer of advanced training for the work with professional interpreters. Since work experience with interpreters significantly predicted their future consultation, training clinicians for triadic work might be a relevant component for increasing the clinicians’ acceptance of professional interpreters.
Limitations
Although we achieved a higher-than-average response rate (Asch et al. 1997), a certain selectivity of the sample cannot be excluded. It could be the case, for example, that clinicians with more positive attitudes towards people with a migration history and the work with interpreters were more likely to participate in the survey. As the study did not aim to ask for attitudes towards cultural diversity or xenophobia, it is not possible to assess the representativeness of the sample with regard to this aspect, and future studies should address this issue.
Since no appropriate scientific instrument existed to measure the variables of interest, the authors decided on the development of a new questionnaire. The reliability of the resulting instrument was in an acceptable range; however, a comprehensive validation of the questionnaire is still pending. Furthermore, it was not possible to identify a meaningful factor structure for the scale on attitudes towards the work with professional interpreters. Thus, further assessments had to be conducted on a single-item basis instead, which limits the explanatory power of some results. As the integration of migrant patients into the health care system is a topic of increasing importance which necessarily includes the involvement of interpreters, the development of solutions for integrating professional interpreters into health care services has to be addressed by future research (Mösko 2022).
Moreover, to get a comprehensive and integrated view on the multilingual supply in outpatient diabetes care, future studies should also take the patients’ perspectives into account in order to be able to answer questions such as the care for patients who have been rejected due to language barriers. Finally, this survey did not differentiate between type 1 and type 2 diabetes. Since complexity and scope of the treatment differentiates depending on the diagnosis, language barriers might accordingly have different consequences. This also should be investigated by future research.
Conclusion
To conclude, this study provides a first overview of existing linguistic resources and barriers in outpatient diabetes care in Germany, surveying all certified practices. The reported low number of patients with limited language proficiency in outpatient diabetes care indicates a clear treatment gap for those patients, caused by multiple barriers. Although MPs have multilingual resources, they are not able to cover the patients’ linguistic needs to a full extent. Only a minority of MPs used and advertised their language skills actively. MPs agreed by a majority that in cases of language barriers the use of qualified interpreting is the best way to guarantee adequate treatment. However, our results showed various obstacles preventing the regular use of professional interpreting in outpatient diabetes care such as increased organizational efforts and unclear financing, as well as clinicians’ reservations about working with interpreters.
As a low language proficiency and language barriers are proven to have a negative impact the health and healthcare of patients with diabetes (American Diabetes Association 2019; Karliner et al. 2007), investing in the improvement of communication quality by promoting the use of linguistic resources and qualified interpreting is inevitable.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Agyemang C, Meeks K, Beune E et al (2006) Obesity and type 2 diabetes in sub-Saharan Africans — Is the burden in today’s Africa similar to African migrants in Europe? RODAM Study BMC Med 14(1):166. https://doi.org/10.1186/s12916-016-0709-0
Ali PA, Watson R (2018) Language barriers and their impact on provision of care to patients with limited English proficiency: nurses’ perspectives. J Clin Nurs 27(5–6):e1152–e1160. https://doi.org/10.1111/jocn.14204
American Diabetes Association (2019) 1. Improving care and promoting health in populations: Standards of Medical Care in Diabetes—2019. Diabetes Care 42(Supplement 1):S7–S12. https://doi.org/10.2337/dc19-S001
Asch DA, Jedrziewski MK, Christakis NA (1997) Response rates to mail surveys published in medical journals. J Clin Epidemiol 50(10):1129–1136. https://doi.org/10.1016/S0895-4356(97)00126-1
Barnett AH, Dixon AN, Bellary S et al (2006) Type 2 diabetes and cardiovascular risk in the UK South Asian community. Diabetologia 49(10):2234–2246. https://doi.org/10.1007/s00125-006-0325-1
Cefalu WT, Golden SH (2005) Innovative approaches to understanding and addressing health disparities in diabetes care and research. Diabetes Care 38(2):186–188. https://doi.org/10.2337/dc14-2748
Chow EA, Foster H, Gonzalez V, McIver L (2012) The disparate impact of diabetes on racial/ethnic minority populations. Clin Diabetes 30(3):130–133. https://doi.org/10.2337/diaclin.30.3.130
Destatis SB (2020) Ausländische Bevölkerung: Ergebnisse des Ausländerzentralregisters. Statistisches Bundesamt, Wiesbaden, Germany
Destatis SB (2023) 24.3% der Bevölkerung hatten 2022 eine Einwanderungsgeschichte. Statistisches Bundesamt, Wiesbaden, Germany. https://www.destatis.de/DE/Presse/Pressemitteilungen/2023/04/PD23_158_125.html. Accessed 11.11.2023
Doran JM, Lawson JL (2021) The impact of COVID-19 on provider perceptions of telemental health. Psychiatr Q 92(3):1241–1258. https://doi.org/10.1007/s11126-021-09899-7
Diamond L, Izquierdo K, Canfield D, Matsoukas K, Gany F (2019) A systematic review of the impact of patient–physician non-English language concordance on quality of care and outcomes. J Gen Intern Med 34(8):1591–1606. https://doi.org/10.1007/s11606-019-04847-5
Fernandez A, Schillinger D, Warton EM et al (2011) Language barriers, physician–patient language concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE). J Gen Intern Med 26(2):170–176. https://doi.org/10.1007/s11606-010-1507-6
Flores G, Abreu M, Barone CP, Bachur R, Lin H (2012) Errors of medical interpretation and their potential clinical consequences: a comparison of professional versus ad hoc versus no interpreters. Ann Emerg Med 60(5):545–553. https://doi.org/10.1016/j.annemergmed.2012.01.025
Gartner K, Mösko M, Becker JC, Hanft-Robert S (2024) Barriers to use of interpreters in outpatient mental health care: exploring the attitudes of psychotherapists. Trans Psychiat Jan 31:13634615241227337
Gogolin I, Androutsopoulos J, Bührig K et al (2017) Mehrsprachigkeit in der nachhaltigen Universität. Projektbericht. Universität Hamburg, Hamburg
Harris MI (2001) Racial and ethnic differences in health care access and health outcomes for adults with type 2 diabetes. Diabetes Care 24(3):454–459
IDF (2021) IDF Diabetes Atlas. 10th edition. International Diabetes Federation, Brussels. https://www.diabetesatlas.org
Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care (2003) Unequal treatment: confronting racial and ethnic disparities in health care. [Smedley BD, Stith AY, Nelson AR (eds)]. National Academies Press, Washington, DC
Jenum AK, Holme I, Graff-Iversen S, Birkeland KI (2005) Ethnicity and sex are strong determinants of diabetes in an urban Western society: implications for prevention. Diabetologia 48(3):435–439. https://doi.org/10.1007/s00125-005-1668-8
Kale E, Syed HR (2010) Language barriers and the use of interpreters in the public health services. A questionnaire-based survey. Patient Educ Couns 81(2):187–191. https://doi.org/10.1016/j.pec.2010.05.002
Karliner LS, Jacobs EA, Chen AH, Mutha S (2007) Do professional interpreters improve clinical care for patients with limited English proficiency? a systematic review of the literature. Health Serv Res 42(2):727–754. https://doi.org/10.1111/j.1475-6773.2006.00629.x
Kirk JK, D’Agostino RB, Bell RA et al (2006) Disparities in HbA levels between African-American and non-Hispanic White adults with diabetes: a meta-analysis. Diabetes Care 29(9):2130–2136. https://doi.org/10.2337/dc05-1973
Liebau E, Romiti A (2014) Bildungsbiografien von Zuwanderern nach Deutschland: Migranten investieren in Sprache und Bildung. IAB-Kurzbericht. Institut für Arbeitsmarkt- und Berufsforschung, Nürnberg, Germany
Mayo R, Parker VG, Sherrill WW et al (2016) Cutting corners: provider perceptions of interpretation services and factors related to use of an ad hoc interpreter. Hisp Health Care Int 14(2):73–80. https://doi.org/10.1177/1540415316646097
Meeks KA, Freitas-Da-Silva D, Adeyemo A et al (2016) Disparities in type 2 diabetes prevalence among ethnic minority groups resident in Europe: a systematic review and meta-analysis. Intern Emerg Med 11(3):327–340. https://doi.org/10.1007/s11739-015-1302-9
Meetoo D (2014) Diabetes: complications and the economic burden. British J Healthcare Manag 20(2):60–67. https://doi.org/10.12968/bjhc.2014.20.2.60
Mösko MO, Gil-Martinez F, Schulz H (2013) Cross-cultural opening in German outpatient mental healthcare service: an exploratory study of structural and procedural aspects. Clin Psychol Psychother 20(5):434–446. https://doi.org/10.1002/cpp.1785
Mösko M, Maggu J, Bührig K, Schulz H (2018) Multilingualism in the hospital in Germany — demands, resources and practices. Eur J Public Health 28(suppl_1):cky047.116. https://doi.org/10.1093/eurpub/cky047.116
Mösko M (2022) Integration of qualified interpreters into outpatient mental health care services: evaluation of a model project. World Congress of World Association of Cultural Psychiatry; Rotterdam, 16.09.2022
Nam S, Chesla C, Stotts NA, Kroon L, Janson SL (2011) Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract 93(1):1–9. https://doi.org/10.1016/j.diabres.2011.02.002
Okrainec K, Booth GL, Hollands S, Bell CM (2015) Impact of language barriers on complications and mortality among immigrants with diabetes: a population-based cohort study. Diabetes Care 38(2):189–196. https://doi.org/10.2337/dc14-0801
Parker MM, Fernández A, Moffet HH, Grant RW, Torreblanca A, Karter AJ (2017) Association of patient–physician language concordance and glycemic control for limited-English proficiency Latinos with Type 2 diabetes. JAMA Intern Med 177(3):380–387. https://doi.org/10.1001/jamainternmed.2016.8648
Schenker Y, Pérez-Stable EJ, Nickleach D, Karliner LS (2011) Patterns of interpreter use for hospitalized patients with limited English proficiency. J Gen Intern Med 26(7):712–717. https://doi.org/10.1007/s11606-010-1619-z
Sohal T, Sohal P, King-Shier KM, Khan NA (2015) Barriers and facilitators for type-2 diabetes management in South Asians: a systematic review. PLoS ONE 10(9):e0136202. https://doi.org/10.1371/journal.pone.0136202
Steinberg EM, Valenzuela-Araujo D, Zickafoose JS, Kieffer E, DeCamp LR (2016) The "battle" of managing language barriers in health care. Clin Pediatr (Phila.) 55(14):1318–1327. https://doi.org/10.1177/0009922816629760
Titus SK, Kataoka-Yahiro M (2019) A systematic review of barriers to access-to-care in Hispanics with type 2 diabetes. J Transcult Nurs 30(3):280–290. https://doi.org/10.1177/1043659618810120
Uitewaal PJ, Manna DR, Bruijnzeels MA, Hoes AW, Thomas S (2004) Prevalence of type 2 diabetes mellitus, other cardiovascular risk factors, and cardiovascular disease in Turkish and Moroccan immigrants in North West Europe: a systematic review. Prev Med 39(6):1068–1076. https://doi.org/10.1016/j.ypmed.2004.04.009
Ujcic-Voortman JK, Schram MT, Jacobs-van der Bruggen MA, Verhoeff AP, Baan CA (2009) Diabetes prevalence and risk factors among ethnic minorities. Eur J Public Health 19(5):511–515. https://doi.org/10.1093/eurpub/ckp096
Williams DR, Lawrence JA, Davis BA (2019) Racism and health: evidence and needed research. Annu Rev Public Health 40:105–125. https://doi.org/10.1146/annurev-publhealth-040218-043750
Wilson E, Chen AHM, Grumbach K, Wang F, Fernandez A (2005) Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med 20(9):800–806. https://doi.org/10.1111/j.1525-1497.2005.0174.x
Yabe M (2020) Healthcare providers’ and deaf patients’ interpreting preferences for critical care and non-critical care: video remote interpreting. Disabil Health J 13(2):100870. https://doi.org/10.1016/j.dhjo.2019.100870
Acknowledgements
The authors would like to thank the German Diabetes Society for supporting the nationwide survey among all certified outpatient diabetological practices in Germany.
Funding
Open Access funding enabled and organized by Projekt DEAL. This online survey was completed with funding from the Department of Medical Psychology of the University Medical Center Hamburg–Eppendorf.
Author information
Authors and Affiliations
Contributions
MM, BS, LB, AI, JA, FB, KB, JW, and HS were involved in the conception, design, and conducting of the study, LR, LB, VM, and MM conducted the analysis or interpretation of the results. LR, LB, VM, and MM drafted the manuscript and/or revised it critically. All authors edited, reviewed, and approved the final version of the manuscript. MM is the guarantor of this work and, as such, takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
According to the local Psychological Ethics Committee of the hospital to which the first author is affiliated to, an ethical approval was not necessary. No patient data was collected within the framework of the health services research study. Full information about the study was enclosed with the letter that was sent to the chief physician of each outpatient center.
Consent to publication
Not applicable.
Conflicts of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mösko, M., Raczek, L., Schilgen, B. et al. Language barriers in German outpatient diabetes care: a cross-sectional study on multilingual treatment and the use of interpreters. J Public Health (Berl.) (2024). https://doi.org/10.1007/s10389-024-02225-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-024-02225-y