Abstract
Aim
In community-based prevention, adopting an evidence-based strategy is known to predict prevention success. Evidence-based prevention includes a theoretical framework, empirical assessment, effective programs, and monitoring of community efforts and outcomes. This study aims to examine the extent to which community capacity explains variation in evidence-based prevention, a known predictor of community-based prevention success.
Subject and methods
The present study is a secondary data analysis based on a survey of 182 key informants in 38 communities. To determine the validity of the measurement, structural validity, internal consistency, and inter-rater agreement were assessed. Associations between adoption of evidence-based prevention and ten domains of community capacity (participation, knowledge & skills, resources, leadership, community power, collaboration consisting of prevention collaboration and sectoral-collaboration, sense of community, critical awareness & problem solving, and community structure) were investigated at the community level using logistic regression models.
Results
Most findings of the validation analysis indicate that the community capacity domains could be reliably measured using key informant reports. Results of logistic regression models indicate that adopting evidence-based prevention is related to increased sense of community (OR 6.62; 95 % CI 2.39-18.39), prevention collaboration (OR 26.05; 95 % CI 5.98-13.39), sectoral-collaboration (OR 10.49; 95 % CI 4.04-27.25), community power (19.29; 1.74-28.12), and community structure (OR 4.79; 95 % CI 1.85-12.43). Availability of leadership was predictive of higher chances of adopting evidence-based prevention (OR 5.21; 95 % CI 1.93-14.02).
Conclusion
Our findings suggest that communities with higher community capacity have increased chances of adopting an evidence-based prevention strategy.
Trial registration
This study was registered with German Clinical Trial Register: DRKS00022819 on Aug 18, 2021.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
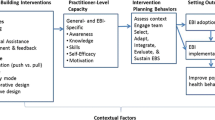
In 1986, the Ottawa Charter marked a paradigm shift in public health by promoting setting-based health promotion, community action and the establishment of health-promoting environments (WHO 1986). In this context, community interventions are emphasized as an health promotion and prevention approach as individuals cannot be considered separately from their social and environmental context (Stokols 1996). Although community-based models provide valuable frameworks for addressing community health issues, in general these interventions have produced only modest effects in changing population health (Feinleib 1996; Schooler et al. 1997; Cheadle et al. 1997). This is attributed to the fact that communities often lack knowledge about evidence-based prevention and thus select and implement prevention programs and strategies that show no or limited effectiveness or have not yet been evaluated. In addition, lack of positive effects of community prevention interventions are linked to unsustainable implementation of prevention strategies or programs (Collins et al. 2007; Botvin 2004; Fixsen et al. 2005; Brownson et al. 2018). Theories of community change emphasize that an evidence-based prevention strategy should include a theoretical framework about risk and protective factors, empirical assessment of prevention needs, use of tested and effective prevention programs, and monitoring of community prevention efforts and outcomes. Within this context, the role of community capacity, understood as the development and sustained implementation of structural capacity (i.e., the availability of resources, structures, and workforce), has gained prominence as a prerequisite for initiating, implementing, and sustaining evidence-based prevention strategies (Beitsch et al. 2010; Baker et al. 2009; Labonte and Laverack 2001). Community capacity can thus be distinguished from similar concepts, such as community readiness, which focus primarily on the initiation of community interventions (Harris et al. 2019). Theories of community change highlight capacity building as an essential step in a sequential process through which community-based interventions lead to desired health outcomes (see Fig. 1) (Easterling et al. 1998; Catalano and Hawkins 1996). In this model, community capacity is required to mobilize community members and organizations, develop opportunities for collaborative partnerships (e.g., through participation in prevention coalitions and work groups), and provide skills for constructive engagement (e.g., in the use of epidemiologic data on risk and protective factors to guide prevention activities) (Beitsch et al. 2010; Baker et al. 2009). An evidence-based strategy is hypothesized to promote the selection and implementation of evidence-based prevention programs that target the needs of the respective community, thereby leading to positive behavioral outcomes that are associated with the health of children and adolescents.
Communities That Care (CTC), a systemic prevention strategy, combines capacity building with the development of evidence-based prevention and has proven effective in reducing adverse health behaviors in children and adolescents (Hawkins et al. 2012). CTC trains communities throughout a five-phase cycle to (1) build capacity for prevention, (2) adopt evidence-based prevention, (3) assess the prevention needs of adolescents living in the community, (4) select, and (5) implement evidence-based programs according to their needs (Rogers 1995). The U.S. Community Youth Development Study (CYDS) found that the positive effects of CTC on adverse health behaviors are mediated by the adoption of an evidence-based prevention strategy promoted by CTC (Brown et al. 2007). These findings provide empirical support for the hypothesized link between evidence-based community prevention efforts and improved population health (Hawkins et al. 2008). However, although all intervention communities in the CYDS implemented CTC with high fidelity (Fagan et al. 2008), the degree to which communities adopted evidence-based prevention varied (Shapiro et al. 2013). Although community capacity building is considered a key element in the recognition, adoption, and implementation of evidence-based prevention (Merzel and D'Afflitti 2003), it lacks on studies examining whether respectively which specific domains of community capacity can facilitate the adoption of an evidence-based prevention strategy in communities. Despite theoretical explanations and case studies addressing community capacity (Goodman et al. 1998; Lempa et al. 2008), community capacity is still is poorly understood and has been associated with various meanings and underlying domains (Banks and Shenton 2001; Crisp 2000; Hawe et al. 1998; Labonte and Laverack 2001). As such, we conducted a scoping review in which we identified domains emphasized for prevention and health promotion prior to this study: community participation, knowledge & skills, resources, leadership, community power, sense of community, collaboration, critical awareness & problem-solving, and community structure. This scoping review provides definitions for each of the capacity domains (Birgel et al. 2023).
To improve the effectiveness of communities in their prevention work, understanding how differences in the capacity of communities may affect their ability to adopt evidence-based prevention is an important step. To contribute to this goal, this study examines the extent to which nine domains of community capacity affects community-wide adoption of an evidence-based prevention strategy, as reported by community leaders. We hypothesize that higher levels of community capacity are associated with a stronger adoption of evidence-based prevention.
Methods
Design
This study is based on baseline data from the study on the effectiveness of the community-based prevention system Communities That Care in Germany (CTC-EFF) (Röding et al. 2021). CTC-EFF is a non-randomized cluster-controlled study.
Sample and data collection
44 small towns, rural communities, or districts of large communities across four German states (Bavaria, Lower Saxony, Rhineland-Palatinate, and Baden-Wuerttemberg) were recruited for this study. A total of 38 communities are included in the current analysis. Three communities dropped out during the recruitment process, and three communities were not included in the analysis because only one person could be interviewed in these communities.
The data collection was based on a translated and German context-adapted version of the Community Key Informant Interview obtained from the Community Youth Development Study (CYDS) (Hawkins et al. 2008). The conceptualized survey is based on the 2009 version of the Community Key Informant Interview (CKI) provided by the Social Development Research Group (SDRG) (SDRG 2009). The translated and abbreviated version underwent cognitive pretesting and multiple loops of revision and initial validation analyses (Röding et al. 2023). Drawing on CYDS, a two-stage process was used to generate a sample of leaders in each of these communities (e.g., mayors, school principals, police officers, youth work leaders, or health officials). First, the research team identified individuals who held formal leadership positions and invited them to participate in the survey. Each surveyed key leader was then asked to identify two individuals in the community thought to be most knowledgeable about current prevention efforts. These individuals were also invited to participate. Data collection was conducted from May to July 2022, with a target of an average of 10 key individuals in each community. For sample-size calculation, see Röding et al. 2021 (Röding et al. 2021). Our sampling strategy yielded 879 community leaders, of whom 196 (22%) participated. Of the 196 respondents, 14 (7.1%) were dropped because the respondents could not provide information about the community. This deletion yielded 182 complete surveys, ranging from 2 to 10 per community, with an average number of 5.6 key informants per community. Data collection was primarily by computer-assisted telephone interview (CATI). As an alternative, a digital form of the instrument was offered as a self-administered survey.
Measures
At the individual level, the constructs presented below represent how key informants in the community rate their community. Based on intersubjective assessments by experts at the community level, they provide an indication of the (approximate) actual status of the community. A measure for the community level is calculated using the mean value of the respective individual-level measures for the community.
Dependent variable
The measure of adoption of evidence-based prevention is conceptually based on the diffusion of innovation metric (Rogers 1995; Arthur et al. 2005). This measure consists of 20 closed questions (e.g., Were risk and protective factors prioritized in your community to be addressed with prevention measures? Did your community decide which programs to implement based on this prioritization? Have prevention programs changed as a result of the evaluation? Has your community made funding decisions based on program evaluations?). An overview of all items is provided in Additional file 1. A total score between zero and five was calculated for each respondent. Thus, this value indicates one of the six levels of adoption of evidence-based prevention (Table 1) and provides a measure of how the respondent ranks their community in terms of adopting a evidence-based prevention (Arthur et al. 2005).
Independent variables
Based on a previously conducted scoping review (Birgel et al. 2023), we identified nine commonly used domains to assess capacity for prevention and health promotion initiatives. On the basis of the definitions of these domains, it was possible to identify items from the CKI that allow measurement of each domain, notwithstanding that the CKI was not originally designed for comprehensive community capacity measurement. Nine domains of community capacity were assessed: (1) Community participation is an average of two items (agree to disagree) that ask community leaders if community members are committed to addressing community issues and believe that they could influence drug, alcohol, and tobacco abuse in the community. Response options for each item consisted of a 4-point scale (agree, somewhat agree, somewhat disagree, and disagree). (2) The construct knowledge & skills is an average of four items (agree to disagree on a 4-pointed Likert-Scale) that capture the knowledge and skills of community members to accomplish positive community development (e.g., My community never seems to be able to accomplish much at all. Generally, people in my community are knowledgeable about local prevention efforts.). (3) Resources is an average of four items. Three items were used to assess the impact of deficiencies in several resource areas. This included a lack of financial resources, lack of human resources, and lack of support in the community. Additionally, leaders were asked if current financial conditions pose a problem for community members. The four items were averaged and measured on a 4-point Likert scale ranging from very much to not at all. (4) Leadership was measured based on one item determining whether a lack of leaders constituted a problem for prevention work (1-4; a lot to not at all). (5) Community power is measured as the community's ability to develop plans that reflect community needs. A dichotomous scale was used to ask whether the community selects new prevention activities to address community needs. (6) Sense of community consists of the average of three items measuring the extent to which community members care about their community, whether the community is tight-knit, and whether most people in the community have a feeling of belonging (1-4; a lot to not at all). (7) Collaboration is measured using two validated multi-item scales. The first scale, consisting of nine items, assesses the quality of prevention collaboration (e.g., There is a network of people involved in prevention and/or health promotion who are in contact with each other. Prevention providers rarely coordinate their activities with each other. In your community, each organization has a clear role in implementing the local prevention plan.) (Brown et al. 2008). The item response scale is four-point: agree, tend to agree, tend to disagree, disagree. For each respondent, a mean is calculated from their responses to these items. We recoded the items so that lower values represent better collaboration. The second construct, sectoral-collaboration, assesses the degree of interagency collaboration perceived by community leaders across the ten community sectors voluntary groups, human service agencies, schools, businesses, social or cultural groups, youth recreation, law enforcement, juvenile justice, media, and religious organizations. This index consisted of responses to the question “In the past year, how much has [your organization] collaborated with [each sector] regarding prevention issues?” with response options coded: 0 = None, 1 = Some, 2 = A little, 3 = A lot. An overall score for each respondent was calculated by averaging responses across all ten sectors. (8) Critical awareness & problem-solving consists of the average of four items concerning the ability and capacity of the community to work together to identify and solve problems (e.g., In the last year, my community has been successful at addressing social problems. This community is willing to try new ideas to solve community problems. Community conflicts are usually resolved in a manner that is respectful of and satisfactory for the people involved.). (9) Community structure is measured as the proportion of individuals from diverse ethnic and cultural backgrounds participating in prevention planning and implementation (1-4; a lot to not at all). An overview of all capacity constructs and related items is provided in Additional file 2.
Confounders
Several possible individual-level confounders were captured in the CKI. Gender was assessed using the categories male, female, and non-binary. Current age was collected as well as migration background. Response categories are: Yes, I was not born in Germany. Yes, at least one parent is not from Germany. No. The respondents' educational status was collected according to the "Demographische Standards" (Beckmann et al. 2016). To have test criteria to determine whether the respondents were actually n the respective study community, it was asked: how many years have you lived in [community]? One answer option was: live elsewhere. This asked whether the person lived in the study community and, if so, how many years already. Furthermore, it was asked: How many years have you been working (including interruptions, if applicable) in [community]? One response option was: I do not work in the community. This question was used to assess whether the person works in the study community and, if so, how many years they have worked there. To have an indicator whether respondents are familiar with the main topic of the survey, it was asked: thinking about your previous professional and volunteer activities, have you worked in the prevention and health promotion field children and adolescents? Response options are: yes, no, and don't know. Respondents who answered yes to this were considered to have experience in this area.
Community-level characteristics potentially related to the adoption of evidence-based prevention were obtained from 2019 data provided by the Federal Institute for Research on Building, Urban Affairs, Spatial Development and consisted of (a) the total population of the community, (b) community fiscal power in € per inhabitant, and (c) the community type (very central, central, peripheral, very peripheral) (BBSR 2019).
Missing data
For the capacity constructs and the adoption score, the item non-response rate was, on average, in the higher single-digit percentage range. Details are shown in Additional file 3. These missing values were replaced in each case by the community-specific mean value of the item. For categorical data, this imputed value was commercially rounded to a whole number.
Analysis strategy
All analyses were conducted using SPSS 27.0 (IBM, Corp., Armonk, NY, USA). Confirmatory factor analysis was performed with the add-on SPSS2LAVAAN package.
To explore the measurement properties of the measures, structural validity, internal consistency, inter-rater agreement, and concurrent construct validity were examined. At this point, it should be noted that the measurement of the adoption of evidence-based prevention has already been validated in the U.S. CYDS (Arthur et al. 2005). As we conceptualized the capacity domains as unidimensional latent constructs, the capacity items were analyzed using confirmatory factor analysis (CFA). The calculation of a CFA is only appropriate for the six capacity domains that consist of more than two items. Evidence of structural validity would be realized if item-factor loadings for the indicator variables were large (i.e., ≥.50), statistically significant (p < 0.05), and if the overall factor model fit the data well. Five model fit indices were used to determine overall model fit: (a) nonsignificant X2, (b) comparative fit index (CFI) greater than .95, (c) Tucker-Lewis fit index (TLI) greater than .95, and (d) root mean square error of approximation (RMSEA) less than .06 (Hu and Bentler 1999; Kline 2015). No covariances between items were allowed. To measure internal consistency of the scales, Cronbach's alpha, McDonald's Omega (Hayes and Coutts 2020), and on the community level O'Brien's (1990) generalizability coefficient were calculated (O'Brien 1990). A 0.6 criterion was used to indicate acceptable internal reliability, with the understanding that constructs with low coefficients will need to be carefully evaluated for the potential of attenuated relationships with other variables (Schmitt 1996; O'Brien 1990). To assess inter-rater reliability the intraclass correlation coefficient (ICC) was determined based on unconditional 2-level hierarchical linear models (HLM) with random intercept (Sampson et al. 1997; Garner and Raudenbush 1991; Raudenbush and Bryk 2002). Additionally, we included the listed possible confounders as macro-regressors in the HLM to test whether they have an effect on the dependent or independent variables (Baltes-Götz n.d.).
The relationship between community capacity and community-wide adoption of an evidence-based prevention strategy was examined using logistic regression models. As the capacity dimensions and the adoption score are characteristics of communities and not individuals, this analysis was conducted at the community level. Therefore, the ratings of the key informants within each community were aggregated into a mean value for each community. For this analysis, the level of adoption of evidence-based prevention was dichotomized into 0 = level zero to level two, and 1 = level three or higher. The capacity dimensions were dichotomized into 0 = below average and 1= above average. In this analysis, confounders that are statistically significant in the previously calculated HLM models will be controlled for.
Results
Sample description
The key informants interviewed are on average 49.6 years old, 48.6% are female, 90.7% have higher education, 6.6% have an immigrant background, 54.5% lived and 83% work in their respective communities, and 69% have experience in the field of prevention (Table 2).
The included communities had an average population (2019 Census data) of 15,984 (range = 2,920 to 55,984) (BBSR 2019).
The mean values, standard deviations, and response range for the capacity subscales and the adoption score before and after missing values were imputed is shown in Additional file 3. The adoption of evidence-based prevention and community collaboration had more missing data than the other scales based on the relatively high number of items comprising the scale. Imputation of the missing values resulted in mainly small changes (changes of a maximum of 0.05 units).
Measurement properties
Using confirmatory factor analysis (CFA) structural validity were tested for the following multi-item-scales: knowledge & skills (4 items), resources (4 items), sense of community (3 items), prevention collaboration (9 items), sectoral-collaboration (8 items), and critical awareness & problem solving (4 items). The CFA model provided a good fit, χ2 (73, n = 182) = 275.70, p = .138, CFI = .96, TLI = .96, RMSEA = .03. Two items from prevention collaboration were removed because this improved the model fit and supported the factorial validity of the measure. The remaining items and their factor loadings are shown in Additional file 4.
With regard to the reliability analysis, we found moderate to good (0.62 to 0.84) internal consistency for the multi-item-scales on the individual level (see Additional file 5). At the community level, the internal consistency of the measures is insufficient to moderate (0.31 to 0.72). The intraclass correlation coefficient ranges from 0.14 to 0.54, indicating that between 14% and 54% of the variance in the measurements is due to differences between communities rather than differences in key informants' ratings of their community (see Additional file 5). Additionally, we ran adjusted HLM with the result that the tested confounders on the individual and community level were not relevant to these models. Accordingly, these measures were not considered for the subsequent logistic regression models.
Community capacity and adoption of evidence-based prevention
Based on unadjusted binary logistic regression models — one for each capacity dimension — odds ratios were calculated as a measure of effect size (see Table 3). Logistic regressions were calculated unadjusted because the previously conducted HLM models revealed that none of the tested individual- or community-level characteristics were significant predictors. It was found that the likelihood of being in stage 3 or higher of adopting evidence-based prevention was significantly greater with above average community power (odds ratio (OR) 19.29; 95 % confidence interval (CI) 1.74-28.12), sense of community (OR 6.62; 95 % CI 2.39-18.39), prevention collaboration (OR 26.05; 95 % CI 5.98-13.39), sectoral-collaboration (OR 10.49; 95 % CI 4.04-27.25), and community structure (OR 4.79; 95 % CI 1.85-12.43). Furthermore, the availability of leadership was found to be predictive of being in stage 3 or higher of adopting evidence-based prevention (OR 5.21; 95 % CI 1.93-14.02).
Discussion
Evidence-based public health (EBPH) emphasizes the adoption of an evidence-based prevention strategy in communities to improve population health (Brownson et al. 2018). However, to recognize and deliver community-based evidence-based prevention, communities need sufficient capacity (Merzel and D'Afflitti 2003).
The present study is a secondary data analysis based on data from Community Key Informant Interviews of CTC-EFF-Study. At community level associations between adoption of evidence-based prevention and ten dimensions of community capacity for prevention were investigated.
In a first step, we assessed the reliability and validity of the investigated constructs. Regarding the structural validity of the six multi-item capacity scales, a CFA show a good model fit. Reliability analyses of this multi-item scales show good to moderate internal consistency at the individual level (0.62 to 0.84). Furthermore, we assessed internal consistency at the community level (O'Brien 1990) for all capacity domains and the adoption of evidence-based prevention finding values from 0.31 to 0.72. In the CYDS for adoption of evidence-based prevention values of 0.71 and 0.75 were found (Arthur et al. 2005). Examination of the variance components of the community capacity measures indicated that variation in the capacity subscales was, for most scales, to a considerable extent due to differences between communities (14-54%). Our values are comparable to or higher than those of studies in which community experts were surveyed (Shapiro et al. 2015; Arthur et al. 2005; Sampson et al. 1997). These results were not found to be dependent on characteristics of the respondents in the community or on characteristics of the communities themselves.
Results of the logistic regression models indicate that community capacity is predictive of adopting evidence-based prevention in communities. All capacity domains showed a positive association with the adoption of evidence-based prevention, with seven (leadership, community power, sense of community, prevention collaboration, sectoral-collaboration, critical awareness & problem-solving, community structure) of ten associations being statistically significant.
Leadership is recognized as important for coordinating and developing community programs and evidence-based program selection. Other studies found that a lack of leadership is associated with unsustainability of implemented programs (Bjärås 1991; Kostadinov et al. 2016). In line with these studies, the present study found that the availability of leadership is associated with higher levels of the adoption of evidence-based prevention. Community power, as an indicator of whether the community can develop plans that address the community's needs, was a predictor of the adoption of evidence-based prevention. Future measures of community power could build on this measure and broaden it to include indicators related to the power to sustain these plans. While current research indicates that a sense of community is an important contextual factor associated with health-behavior (Hystad and Carpiano 2012), this study found that a sense of community is also associated with community prevention work. Previous studies found that communities that worked together to address health problems were more likely to achieve positive health behaviors (Underwood et al. 2012; Kim et al. 2020). Both, prevention collaboration and sectoral-collaboration are predictive of an evidence-based prevention strategy. Furthermore, critical awareness & problem-solving, referring to the ability of the community to work together to identify and solve problems, correlated significantly with the stage of the adoption of evidence-based prevention on the community level. Community structure, defined as how much individuals from diverse ethnic and cultural backgrounds participate in prevention planning and implementation, have a positive statistically significant effect on adopting evidence-based prevention.
These findings have important implications for prevention and health promotion. While public health researchers and practitioners have advocated capacity building as essential for improving community health outcomes, there have been few approaches to linking community capacity with the adoption of a evidence-based prevention strategy (Shapiro et al. 2015; Duffy et al. 2012; Lesesne et al. 2008; Brownson et al. 2018). Before introducing an evidence-based prevention strategy, it is important to examine and, if necessary, increase community capacity for prevention. The present findings suggest that capacity building efforts should focus on education in prevention evidence, strengthen leadership, build intersectoral networks of collaboration, enhance problem-solving skills and critical awareness, establish an ethnically and culturally diverse network for prevention work, and capture community needs.
Limitations
Some limitations in this study are worth highlighting. First, as our study was cross-sectional, it is not possible to ascertain a true cause and effect relationship. Therefore, the upcoming waves of the CTC-EFF study should be used to investigate a temporal relationship between the dependent and independent variables. Second, the target sample size of n=10 could not be achieved in all participating communities. A larger sample size would have provided more accurate mean values. However, a sample size of N=182 was considered sufficient for the conducted analyses. But, it was not possible to use multilevel procedures to impute missing values, as these require a higher sample size with a large number of clusters (Donner and Klar 2000; Campbell et al. 2000; Wears 2002). The imputation procedure we used considers the data's cluster structure but not the respondents' characteristics, so individual-level confounders could not be controlled for. Given that our measured constructs exclusively pertain to community characteristics and not to individuals, and that our imputation process only resulted in minor changes to mean and standard deviation, we presume any biases introduced would be minor. A noteworthy consideration is our decision in our study was the need to dichotomize the independent and dependent variables for analysis due to the small community sample size. While dichotomization was necessary and beneficial, it is important to consider that such dichotomization could potentially inflate effect sizes, especially in relation to Odds Ratios (MacCallum et al. 2002). Another limitation is that the communities do not represent a random selection of communities, which may limit the generalizability of findings from this study. A further constraint is relying exclusively on self-report survey data from key community leaders. We note, however, that key informant survey data have been used widely in community research (Brown et al. 2014; Shinn 1990).
Conclusion
This study provides evidence that most domains of community capacity predict the adoption of evidence-based prevention. Before implementing evidence-based prevention strategies, community capacity should therefore be assessed and, if necessary, improved beforehand.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available as they contain information that could comprise research participant privacy.
Code availability
Not applicable.
References
Arthur MW, Glaser RR, Hawkins JD (2005) Steps Toward Community-Level Resilience. In: Peters RD, Leadbeater B, McMahon RJ (eds) Resilience in Children, Families, and Communities. Springer, US, pp 177–194
Baker EA, Brownson RC, Dreisinger M, McIntosh LD, Karamehic-Muratovic A (2009) Examining the role of training in evidence-based public health: a qualitative study. Health Prom Pract 10(3):342–348. https://doi.org/10.1177/1524839909336649
Baltes-Götz B (n.d.) Analyse von hierarchischen linearen Modellen mit SPSS. https://www.uni-trier.de/fileadmin/urt/doku/hlm/hlm.pdf. Accessed 14 December 2022
Banks S, Shenton F (2001) Regenerating Neighbourhoods: A Critical Look at the Role of Community Capacity Building. Local Econ 16(4):286–298. https://doi.org/10.1080/02690940110078265
BBSR (2019) Indicators and maps of spatial and urban development. https://www.inkar.de/. Accessed 14 December 2022
Beckmann K, Glemser A, Heckel C, von der Heyde C, Hoffmeyer-Zlotnik JHP, Hanefeld U, Herter-Eschweiler R, Kühnen C (2016) Demographische Standards Ausgabe 2016. Eine gemeinsame Empfehlung des ADM Arbeitskreis Deutscher Markt- und Sozialforschungsinstitute e.V., der Arbeitsgemeinschaft Sozialwissenschaftlicher Institute e.V. (ASI) und des Statistischen Bundesamtes. https://www.statistischebibliothek.de/mir/receive/DEMonografie_mods_00003695
Beitsch LM, Leep C, Shah G, Brooks RG, Pestronk RM (2010) Quality improvement in local health departments: results of the NACCHO 2008 survey. J Public Health Manag Pract JPHMP 16(1):49–54. https://doi.org/10.1097/phh.0b013e3181bedd0c
Birgel V, Decker L, Röding D et al (2023) Community capacity for prevention and health promotion: a scoping review on underlying domains and assessment methods. Syst Rev 12:147. https://doi.org/10.1186/s13643-023-02314-1
Bjärås G (1991) The need of leadership for motivation of participants in a community intervention programme. Scand J Soc Med 19(3):190–198. https://doi.org/10.1177/140349489101900309
Botvin GJ (2004) Advancing prevention science and practice: challenges, critical issues, and future directions. Prev Sci Off J Soc Prev Res 5(1):69–72. https://doi.org/10.1023/b:prev.0000013984.83251.8b
Brown EC, Hawkins JD, Arthur MW, Briney JS, Abbott RD (2007) Effects of Communities That Care on prevention services systems: findings from the community youth development study at 1.5 years. Prev Sci 8(3):180–191. https://doi.org/10.1007/s11121-007-0068-3
Brown EC, Hawkins JD, Arthur MW, Abbott RD, van Horn ML (2008) Multilevel analysis of a measure of community prevention collaboration. Am J Commun Psychol 41(1-2):115–126. https://doi.org/10.1007/s10464-007-9154-8
Brown EC, Hawkins JD, Rhew IC, Shapiro VB, Abbott RD, Oesterle S, Arthur MW, Briney JS, Catalano RF (2014) Prevention system mediation of communities that care effects on youth outcomes. Prev Sci 15(5):623–632. https://doi.org/10.1007/s11121-013-0413-7
Brownson CA, Allen P, Yang SC, Bass K, Brownson RC (2018) Scaling Up Evidence-Based Public Health Training. Prev Chronic Disease 15:E145. https://doi.org/10.5888/pcd15.180315
Campbell MK, Mollison J, Steen N, Grimshaw JM, Eccles M (2000) Analysis of cluster randomized trials in primary care: a practical approach. Family Pract 17(2):192–196. https://doi.org/10.1093/fampra/17.2.192
Catalano RF, Hawkins JD (1996) The social development model: A theory of antisocial behaviour. In: Hawkins JD (ed) Delinquency and crime: Current theories. Cambridge University Press, New York, pp 149–197
Cheadle A, Beery W, Wagner E, Fawcett S, Green L, Moss D, Plough A, Wandersman A, Woods I (1997) Conference Report: Community-Based Health Promotion—State of the Art and Recommendations for the Future. Am J Prev Med 13(4):240–243. https://doi.org/10.1016/S0749-3797(18)30169-7
Collins C, Phields ME, Duncan T (2007) An agency capacity model to facilitate implementation of evidence-based behavioral interventions by community-based organizations. J Public Health Manag Pract JPHMP Suppl:S16-23. doi:https://doi.org/10.1097/00124784-200701001-00005
Crisp BR (2000) Four approaches to capacity building in health: consequences for measurement and accountability. Health Prom Int 15(2):99–107. https://doi.org/10.1093/heapro/15.2.99
Donner A, Klar N (2000) Design and analysis of cluster randomization trials in health research. John Wiley & Sons, Ltd, Chichester
Duffy JL, Prince MS, Johnson EE, Alton FL, Flynn S, Faye AM, Padgett PE, Rollison C, Becker D, Hinzey AL (2012) Enhancing teen pregnancy prevention in local communities: capacity building using the interactive systems framework. Am J Commun Psychol 50(3-4):370–385. https://doi.org/10.1007/s10464-012-9531-9
Easterling D, Gallagher K, Drisko J, Johnson T (1998) Promoting Health by Building Capacity: Evidence and Implications for Grantmakers. The Colorado Trust:1–24
Fagan AA, Hanson K, Hawkins JD, Arthur MW (2008) Bridging science to practice: achieving prevention program implementation fidelity in the community youth development study. Am J Commun Psychol 41(3-4):235–249. https://doi.org/10.1007/s10464-008-9176-x
Feinleib M (1996) New directions for community intervention studies. Am J Public Health 86(12):1696–1698. https://doi.org/10.2105/AJPH.86.12.1696
Fixsen D, Naoom S, Blase K, Friedman R, Wallace F (2005) Implementation research: a synthesis of the literature. University of South Florida, Louis de la Parte Florida Mental Health Institute, National Implementation Research Network, Tamps
Garner CL, Raudenbush SW (1991) Neighborhood Effects on Educational Attainment: A Multilevel Analysis. Sociol Educ 64(4):251. https://doi.org/10.2307/2112706
Goodman RM, Speers MA, McLeroy KR, Fawcett S, Kegler MC, Parker E, Smith SR, Sterling TD, Wallerstein N (1998) Identifying and defining the dimensions of community capacity to provide a basis for measurement. Health Educ Behavior 25(3):258–278. https://doi.org/10.1177/109019819802500303
Harris KJ, Brown B, Shankle L, Tryon M, Pedersen M, Panarella SK, Swaney G (2019) Community Readiness Model for Prevention Planning: Addressing Childhood Obesity in American Indian Reservation Communities. J Racial Ethnic Health Disparities 6(6):1144–1156. https://doi.org/10.1007/s40615-019-00616-6
Hawe P, King L, Noort M, Gifford SM, Lloyd B (1998) Working Invisibly: Health Workers Talk About Capacity-Building in Health Promotion. Health promotion international 13(4):285–295. https://doi.org/10.1093/heapro/13.4.285
Hawkins JD, Catalano RF, Arthur MW, Egan E, Brown EC, Abbott RD, Murray DM (2008) Testing communities that care: the rationale, design and behavioral baseline equivalence of the community youth development study. Prev Sci 9(3):178–190. https://doi.org/10.1007/s11121-008-0092-y
Hawkins JD, Oesterle S, Brown EC, Monahan KC, Abbott RD, Arthur MW, Catalano RF (2012) Sustained decreases in risk exposure and youth problem behaviors after installation of the Communities That Care prevention system in a randomized trial. Arch Pediatr Adolescent Med 166(2):141–148. https://doi.org/10.1001/archpediatrics.2011.183
Hayes AF, Coutts JJ (2020) Use Omega Rather than Cronbach’s Alpha for Estimating Reliability. But…. Commun Methods Measures 14(1):1–24. https://doi.org/10.1080/19312458.2020.1718629
Hu L, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Eq Model: A Multidisciplin J 6(1):1–55. https://doi.org/10.1080/10705519909540118
Hystad P, Carpiano RM (2012) Sense of community-belonging and health-behaviour change in Canada. J Epidemiol Commun Health 66(3):277–283. https://doi.org/10.1136/jech.2009.103556
Kim JM, Lee H, Cho E, Lee KH, Park CG, Cho B-H (2020) Multilevel Effects of Community Capacity on Active Aging in Community-Dwelling Older Adults in South Korea. Asian Nurs Res 14(1):36–43. https://doi.org/10.1016/j.anr.2020.01.001
Kline RB (2015) Principles and Practice of Structural Equation Modeling, 4th edn. Guilford Press
Kostadinov I, Daniel M, Jones M, Cargo M (2016) Assessing change in perceived community leadership readiness in the Obesity Prevention and Lifestyle program. Health Prom J Australia 27(3):208–214. https://doi.org/10.1071/HE16050
Labonte R, Laverack G (2001) Capacity building in health promotion, Part 1: for whom? And for what purpose? Critical Public Health 11(2):111–127. https://doi.org/10.1080/09581590124801
Lempa M, Goodman RM, Rice J, Becker AB (2008) Development of scales measuring the capacity of community-based initiatives. Health Educ behavior 35(3):298–315. https://doi.org/10.1177/1090198106293525
Lesesne CA, Lewis KM, White CP, Green DC, Duffy JL, Wandersman A (2008) Promoting science-based approaches to teen pregnancy prevention: proactively engaging the three systems of the interactive systems framework. Am J Commun Psychol 41(3-4):379–392. https://doi.org/10.1007/s10464-008-9175-y
MacCallum RC, Zhang S, Preacher KJ, Rucker DD (2002) On the practice of dichotomization of quantitative variables. Psychol Methods 7(1):19–40. https://doi.org/10.1037/1082-989X.7.1.19
Merzel C, D'Afflitti J (2003) Reconsidering community-based health promotion: promise, performance, and potential. Am J Public Health 93(4):557–574. https://doi.org/10.2105/AJPH.93.4.557
O'Brien RM (1990) Estimating the Reliability of Aggregate-Level Variables Based on Individual-Level Characteristics. Sociol Methods Res 18(4):473–504. https://doi.org/10.1177/0049124190018004004
Raudenbush SW, Bryk AS (2002) Hierarchical Linear Models: Applications and data analysis methods, 2nd edn. Sage Publications, Inc, Thousand Oaks
Röding D, Soellner R, Reder M, Birgel V, Kleiner C, Stolz M, Groeger-Roth F, Krauth C, Walter U (2021) Study protocol: a non-randomised community trial to evaluate the effectiveness of the communities that care prevention system in Germany. BMC Public Health 21(1):1927. https://doi.org/10.1186/s12889-021-11935-x
Röding D, Birgel V, Walter U (2023) Validation of an instrument to measure community capacity building for prevention. J Public Health. https://doi.org/10.1007/s10389-023-01905-5
Rogers E (1995) Diffusion of innovations, 4th edn. Free Press, New York
Sampson RJ, Raudenbush SW, Earls F (1997) Neighborhoods and violent crime: a multilevel study of collective efficacy. Science (New York, N.Y.) 277(5328):918–924. doi:https://doi.org/10.1126/science.277.5328.918
Schmitt N (1996) Uses and abuses of coefficient alpha. Psychol Assess 8(4):350–353. https://doi.org/10.1037/1040-3590.8.4.350
Schooler C, Farquhar JW, Fortmann SP, Flora JA (1997) Synthesis of findings and issues from community prevention trials. Annals Epidemiol 7(7):S54–S68. https://doi.org/10.1016/S1047-2797(97)80008-7
SDRG (2009) Community Youth Development Study. Community Key Informant Survey, Seattle
Shapiro VB, Hawkins JD, Oesterle S, Monahan KC, Brown EC, Arthur MW (2013) Variation in the Effect of Communities That Care on Community Adoption of a Scientific Approach to Prevention. J Soc Social Work Res 4(3). https://doi.org/10.5243/jsswr.2013.10
Shapiro VB, Hawkins JD, Oesterle S (2015) Building Local Infrastructure for Community Adoption of Science-Based Prevention: The Role of Coalition Functioning. Prev Sci 16(8):1136–1146. https://doi.org/10.1007/s11121-015-0562-y
Shinn M (1990) Mixing and matching: Levels of conceptualization, measurement, and statistical analysis in community research. In: Tolan P, Keys C, Chertok F, Jason LA (eds) Researching community psychology: Issues of theory and methods. American Psychological Association, Washington, pp 111–126
Stokols D (1996) Translating social ecological theory into guidelines for community health promotion. Am J Health Prom AJHP 10(4):282–298. https://doi.org/10.4278/0890-1171-10.4.282
Underwood C, Boulay M, Snetro-Plewman G, Macwan'gi M, Vijayaraghavan J, Namfukwe M, Marsh D (2012) Community capacity as means to improved health practices and an end in itself: evidence from a multi-stage study. Int Quart Commun Health Educ 33(2):105–127. https://doi.org/10.2190/IQ.33.2.b
Wears RL (2002) Advanced statistics: statistical methods for analyzing cluster and cluster-randomized data. Acad Emerg Med Off J Soc Acad Emerg Med 9(4):330–341. https://doi.org/10.1111/j.1553-2712.2002.tb01332.x
WHO (1986) Ottawa charter for health promotion. https://www.who.int/teams/health-promotion/enhanced-wellbeing/frst-global-conference. Accessed 09 February 2023. Accessed 09 February 2023
Acknowledgements
We would like to thank former and current members of the Social Development Research Group at Washington University for their guidance in conducting the study and John and Danielle Woodward, University of Washington, for the survey instruments and other materials from the youth community development study. We would also like to thank the Verwey-Jonker Instituut Netherlands, for supporting our study. We acknowledge the support of the German Research Foundation and the Open Access Publishing Fund Hannover Medical School.
Funding
Open Access funding enabled and organized by Projekt DEAL. The Federal Ministry of Education and Research (BMBF) supported the current project (funding number: 01EL2006A). None of the funders were involved in the study design, manuscript writing, or data collection. The funders will not be involved in data analysis or interpretation and manuscript writing in the future.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception, design, and adaptation of the instrument. VB and DR performed data collection, analysis and interpretation. The first draft of the manuscript was written by VB and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The questionnaire and methodology for this study was approved by the Hannover Medical School’s ethics committee (Ethics approval number: 9739_BO_K_2021). All participating communities completed an informed consenting process with a research team member. Written informed consent was obtained from all individual participants included in the study. The respondents were informed that their inclusion in the study was voluntary, and that they were free to withdraw from the study if they were not willing to participate. To ensure respondents’ confidentiality, their names were stored in separate, protected files, and the anonymity of the respondents was maintained.
Ethics approval
This study was approved by the Hannover Medical School’s ethics committee (9739_BO_K_2021).
Consent to participate
All participating communities completed an informed consenting process with a research team member. Written informed consent was obtained from all individual participants included in the study. The respondents were informed that their inclusion in the study was voluntary, and that they were free to withdraw from the study if they were not willing to participate. To ensure respondents’ confidentiality, their names were stored in separate, protected files, and the anonymity of the respondents was maintained.
Consent for publication
Not applicable.
Conflict of interest
The authors have no competing interests to declare relevant to the article’s content.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Birgel, V., Walter, U. & Röding, D. Relating community capacity to the adoption of an evidence-based prevention strategy: a community-level analysis. J Public Health (Berl.) (2023). https://doi.org/10.1007/s10389-023-02159-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-023-02159-x