Abstract
Objective
This study aimed to explore the relationship between different complementary feeding (CF) indicators and coexisting forms of malnutrition (CFM) in Pakistan.
Methodology
This study involves secondary data analysis of eight national and regional datasets of Pakistan, which were retrieved from the Demographic Health Survey (DHS) and UNICEF. From these datasets, data of children aged between 6 to 23.9 months was analysed after excluding incomplete and/or invalid data related to their feeding practices and anthropometry. Thus, data of 30,097 Pakistani children between the ages of 6 to 23.9 months was analysed in this study using Jamovi software.
Results
The prevalence of CFM in this sample of children was 28.1%. Cereals and dairy were chiefly used for CF. With the exception of continuation of breastfeeding and coadministration of breastmilk with solid/semi-solid/soft food, adherence to all other CF indicators (minimum dietary diversity, minimum meal frequency, iron & folate consumption, egg & flesh food consumption, zero vegetable & fruit consumption) were associated with reduced odds of various forms of CFM.
Conclusion
Nutritional adversities in children may be prevented by improving the dietary diversity, meal frequency, protein consumption, iron & folic acid (IFA) use, and food fortification.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
The first thousand days of life, from conception to two years of age, are crucial for the growth and nourishment of a child (Bhutta et al. 2013; Jones et al. 2003). During this period, a child undergoes intra-natal as well as postnatal development, for which adequate nutrition is essential (Martorell 2017). Deficiency of any nutrients during this critical period puts children at risk of various communicable and non-communicable diseases, and nutrition-related disorders including coexisting forms of malnutrition (CFM) (Scott 2020). CFM represents the simultaneous presence of more than one type of nutritional disorder in an individual (Khaliq et al. 2021; Khaliq et al. 2022a, b). Certain nutritional interventions, such as food fortification, maternal supplementation with iron & folate and infant feeding practices such as exclusive breastfeeding (EBF) for the first six months of life and appropriate introduction to complementary feeding (CF) from six months to two years has the potential to avert certain types of nourishment disorders, including CFM (Bhutta et al. 2013; Jones et al. 2003).
Child feeding practices are influenced by their postnatal age. Thus, the World Health Organization (WHO) has separated feeding practices into two major divisions: Exclusive Breastfeeding (EBF) for children below 6 months, and Complementary feeding (CF) for children between 6 to 23.9 months (World Health Organization 2021). Feeding practices, when not followed appropriately may result in various types of health adversities, such as malnutrition, including CFM (Korir 2013). Worldwide, half of the deaths in children are due to various forms of malnutrition, including CFM (Dhami et al. 2019).
CFM refers to presence of more than one nutritional disorder in an individual irrespective of age, sex, geographical location, and assessment methods (Khaliq et al. 2021; Khaliq et al. 2022a, b). The Global Nutrition Report from 2018- 2019 (GNR) raised the concerns of CFM for the first time. The report presented the prevalence of two specific types of CFM: coexistence of wasting with stunting, and coexistence of stunting with overweight/obesity (Global nutrition report 2018, 2019, 2021; Khaliq et al. 2022a). In 2020, a report by WHO also raised concerns about CFM in underweight children, and their vulnerability to developing various forms of CFM, such as coexistence of underweight with wasting, underweight with stunting, and underweight with both wasting and stunting (World Health Organization 2020a). Children aged between 6 to 23.9 months are at higher risk of nutritional disorders (Khaliq et al. 2021; Sadhu and Hemangini 2020). Thus, it may be expected that children aged between six to 23.9 months will have high prevalence of CFM as well.
Pakistan is the second largest South Asian country, after India. The country has a history of high prevalence of various forms of malnutrition (United Nations Development Programme 2020). Over the last four decades, Pakistan showed either stagnant or only slight improvement in the nutritional profile of children aged under five years (National Institute of Population Studies (NIPS) 2019; United Nations Children Funds 2019). The continuing high prevalence of various forms of malnutrition in children of Pakistan might be attributable to poor feeding practices. The findings of our previous study demonstrated that in Pakistan the practice of supplementary breastfeeding (SBF) and complete weaning were two major barriers for exclusive breastfeeding (EBF) adherence in children below six months of age (Khaliq et al. 2022b). The non-adherence to EBF was associated with a two-fold increase in the odds of coexisting forms of undernutrition in children aged 0 to 6 months. Similarly, the adherence to CF indicators among under two-years children of Pakistan plunged down to 36% in National Nutrition Survey (NNS) of 2018 from 51% in NNS of 2011, which is around 1.5 folds lower than global CF practices (United Nations Children Funds 2019; World Health Organization 2020b). In the past, attempts were made to establish a connection between CF non-adherence and standalone forms of nutrition disorders, i.e., stunting, wasting, and underweight (Dagne et al. 2019; White et al. 2017; Zhou et al. 2012), but the relationship of CF indicators with various types of CFM is not yet known. This study primarily aims to examine the relationship of different CF indicators with various types of CFM in children aged between 6 to 23.9 months using datasets of Pakistan Demographic & Health Surveys (PDHS) and Multiple Indicator Cluster Surveys (MICS). This is the first study to examine the relationship between each individual CF indicator, including newly introduced CF indicators, such as Egg & Flesh food consumption (EFF) and Zero Vegetables & Fruits consumption (ZVF), and CFM. Findings can be used to guide policy makers, programme managers, clinicians, and caregivers about the role of each CF indicator and food group for the prevention and control of various forms of malnutrition, including CFM.
Methodology
Study setting and study design
This is a community-based study, which assessed the relationship between CFM and CF practices using eight cross-sectional surveys of national and regional level. A total of eight datasets: two from Pakistan Demographic and Health Surveys (PDHS) and six from Multiple Indicator Clusters Surveys (MICS) were used. The PDHS is the national representative dataset, and MICS is the regional representative dataset.
Study population and their eligibility criteria
This study measured the relationship of CFM with the CF practices of infants and young children from the PDHS and MICS datasets. Datasets which contain data related to the CF indicators were included. The PDHS datasets of 2012-2013 and 2017-2018, and MICS-5 (2014-2017) and MICS-6 (2017-2020) contain CF indicators aligned with the Infant and Young Child feeding (IYCF) guidelines for children aged between 6 months to 23.99 months (World Health Organization 2010). The PDHS and MICS datasets from before 2012 were excluded, because they were devoid of CF indicators matching the most recent IYCF guidelines (World Health Organization 1991, 2010). Data of all children aged between 6 to 23.9 months having valid and complete anthropometry was analysed. Moreover, data of children with incomplete feeding status was also excluded. The details regarding the eligibility criteria and targeted population of this study from each dataset is presented in Supplementary file 1.
Sampling methods and sample size
The data in each PDHS and MICS survey was collected from women aged between 15-49 years by adopting a multistage stratified cluster sampling technique (National Institute of Population Studies (NIPS) 2019). However, this study targeted children aged between six to 23.9 months. The data of all the children having age either below six months or over 24 months was excluded sequentially. Furthermore, data of all the children with incomplete and invalid anthropometry and incomplete feeding information was also excluded. After excluding the data of all the ineligible children’s data from 30,097 children were analysed (Supplementary file 1).
Measurement of study outcome
The nutrition status in each PDHS was assessed by two trained data collectors, who received three to four weeks training related to the survey ethics, interview technique, mock and actual field practice before actual project implementation. The trained data collectors measured the weight and length/height for each child. Child weight was recorded in kilograms, while length was recorded in centimetres. These anthropometric measurements, along with child sex and age were entered into the WHO AnthroCal® software to determine the following z-scores: WHZ (Weight for Height z-score), WAZ (Weight for Age z-score) and HAZ (Height for Age z-score). In this study, BAZ (BMI for age z-score) was excluded because it overestimates paediatric overweight/obesity level (Zhang et al. 2018). Based on WHZ, WAZ and HAZ scores, different types of standalone forms of malnutrition, such as wasting, overweight/obesity, underweight, and stunting were identified. Any child having WHZ, WAZ, and HAZ z-score less than -2.00, were identified as wasted, underweight, and stunted, respectively. Children having WAZ and HAZ z-score either equivalent to or more than -1.99 were classified as normal children. A child is referred to as normal if his/her WHZ z-scores ranged between -1.99 to +1.99, but if the z-score value exceeds +2.00 or more then he/she will be classified as overweight/obese. A coding system was designed for defining different types of coexisting forms of malnutrition. Four different types of CFM were identified, of which three represent coexisting forms of undernutrition (coexistence of underweight with stunting, coexistence of underweight with wasting, and coexistence of underweight with stunting and wasting both), and one represents contrasting forms of malnutrition (coexistence of stunting with overweight/obesity).
Conceptual framework
For assessing the relationship of CFM with CF of children, we proposed a conceptual framework after a thorough review of the literature (De-Vries et al. 2014; Goday et al. 2019; Korir 2013; Martorell 2017; Neu 2007). According to our proposed conceptual framework, complementary feeding practices of a child are influenced by child age, health and medical condition, exposure to different types of foods, interaction of a child with caregiver, and accessibility and affordability of food.
The IYCF guidelines advised CF for children aged between 6 to 23.9 months, because children below six-months of age have an immature gastrointestinal tract (Neu 2007; World Health Organization 2021). Early initiation of CF in neonates and infants before six-months of age may result in several types of gastrointestinal complaints, including nausea & vomiting, indigestion, diarrhoea, or constipation (Neu 2007). Certain medical conditions, such as presence of oesophageal atresia, laryngeal anomality, and oropharyngeal anomality, and cleft palate drastically influences child feeding behaviour, thereby leading to malnutrition (De-Vries et al. 2014; Goday et al. 2019). Moreover, accessibility, affordability, taste/flavour, texture, temperature, quality, viscosity, and appearance of food/fluid and interaction with the caregiver also affect the feeding practices and nutritional status of children (Goday et al. 2019) (Fig. 1)
Risk factors
Potential risk factors which may influence the relationship between CF and CFM in infants and young children that were accounted for in this research included:
-
Biological factors may include child biological age, child gestational age, birthweight, birth size, gender, immunisation status, health status, and presence/absence of congenital anomality. The datasets used in this study were devoid of many biological factors, thus we were only able to account for child current age (6-11.9 months, 12 to 17.9 months, and 18-23.9 months), gender (male, and female), and history of illness in past 14 days (Yes and No) for further analysis. We excluded certain variables, such as Birthweight and birth size, because of inadequate information about birthweight in each dataset and the subjective assessment of birth size. Moreover, the reasons related to low birthweight (LBW), and of small birth size were not available in any datasets (Ramachandran 2015).
-
Caregiver influence was assessed as maternal education (no education, primary, secondary/higher)
-
Food accessibility and affordability factors included socioeconomic status (poorest, poorer, middle, richer, and richest), and type of place of residence (urban, and rural) as food accessibility and affordability factors. Factors related to family size, food insecurity, food accessibility, and food affordability were not available in the datasets.
Measurement of complementary feeding indicators
Research assistants collected data pertaining to CF indicators from the mother of the child aged below two years using dietary recall over the past 24 hours. The datasets used in this study collected information about the use of different food items (Supplementary file 2). Using this data (outlined in Table 1), CF indicators were created based on the IYCF guidelines (World Health Organization 1991, 2010, 2021) (Fig. 2). Indicators were developed for the consumption of solid/semi-solid food with breast milk, Minimum Dietary Diversity (MDD), Minimum Meal Frequency (MMF), Minimum Acceptable Diet (MAD), Iron & folate rich food, Egg, and flesh food consumption (EFF) and Zero vegetable and fruits consumption (ZVF) as individual CF indicators (outlined below), while the cumulative effects of CF indicators were also assessed. The details about the definition and measurement parameter of each feeding indicator can be accessed from Supplementary file 3.
Statistical analysis
We used Jamovi for the analysis of data. In this study, all the PDHS and MICS datasets were merged after excluding the data of all the ineligible participants. Following descriptive analysis, the crude odds of each predictor (i.e., CF indicators) and covariate (i.e., child age, child sex, child health, maternal education, wealth index, and type of place of residence) were calculated for assessing the association with CFM. Then, we calculated adjusted odds using multinomial logistic regression for assessing the association of each CF indicator with various forms of CFM. In this study, a total of nine regression models were used to separately assess the associations between each feeding indicator and various forms of CFM. During multinomial logistic regression, a normal healthy child having z-score ranged between -1.99 to +1.99 S.D. was used as the referent category. In all the multivariate models, we removed all the non-significant covariates sequentially (i.e., p value >0.05), with the exception of study predictor variables, until the final model contained only significant covariates (i.e., p-value ≤0.05). Multicollinearity was also examined, and we excluded all the covariates with variance inflation factor (VIF) of 2.5 or more. Moreover, sub-group analysis was performed for assessing the difference between standalone forms of malnutrition and CFM. For sub-group analysis, we performed binomial regression, with stunting as the referent category for coexistence of stunting with overweight/obesity and underweight as the referent for remaining three types of CFM: underweight with wasting, underweight with stunting, and underweight with both wasting & stunting. Additionally, the interaction of different covariates, such as child age, gender, health status, maternal education, wealth index, and place of residence was also assessed for each form of malnutrition, including CFM. Rather than assessing the adjusted interaction of each model, the interaction of each study covariate with different CF indicators was assessed individually because the adjusted model showed evidence of model overfitting (Supplementary file 5).
Results
Description of study population
Data from 30,097 children aged between 6 months to 23.9 month were analysed using MICS and PDHS datasets. Table 1 presents the demographic and dietary profile of the sample.
Among seven food groups, cereals and grains had the highest dietary consumption of over 80%, followed by dairy products consumption (i.e., around 70%). However, the dietary consumption from other food groups: eggs, meat & fish, vitamin A containing fruits & vegetables, other fruits & vegetables, and legumes & nuts was less than 30%.
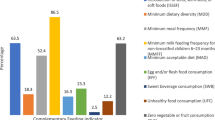
Among different CF indicators, adherence to BF and coadministration of SSF with BF was 68.7% and 65.1%, respectively. Adherence to MDD and MMF was 21.8% and 54.3%, while adherence to MAD was 18.9%. Other CF indicators, such as iron & folate supplementation, ZVF, and EFF also had an adherence of less than 30%. Overall adherence to CF practices was evident in 8% of children. (Table 1).
Prevalence of malnutrition in children under two-years of age
Malnutrition was evident in 42.3% children aged between 6 to 23.9 months, of which 18.2% had standalone forms of malnutrition, and the remaining 28.1% had CFM. Among various types of malnutrition, coexistence of underweight with stunting was one of the leading types of CFM, prevalent in more than 10% of children. The prevalence of stunting with overweight/obesity was lowest, i.e. (1.3%) (Table 1 and Fig. 3)
Determinants of Coexisting forms of Malnutrition (CFM)
Determinants of Coexistence of underweight with wasting
We found a significantly lower odds of coexistence of underweight with wasting in children who consumed iron & folate rich food, and egg & flesh food in last 24 hours. Zero vegetables & fruits (ZVF) significantly increased the odds of coexistence of underweight with wasting by 15% (Table 2). Sub-group analysis showed a significantly higher odds of coexistence of underweight with wasting in MAD adherent children, compared with underweight children (Table 3).
Determinants of Coexistence of underweight with stunting
Compared to a normal child, adherence to breastfeeding either alone or in conjunction with solid/semi-solid food, and ZVF significantly increased the odds of coexistence of underweight with stunting (Table 2). Adherence to MDD, MMF, Iron & Folate food consumption, EEF, and overall CF adherence significantly reduced the odds of coexistence of underweight with stunting. The coexistence of underweight with stunting when compared with underweight children was associated with the continuation of breastfeeding and with the coadministration of breastfeeding with solid/semi-solid food administration. Compared with underweight children, the odds of coexistence of underweight with stunting increased to 1.31 (1.09 to 1.57) in children who continued to take breastmilk at age between 6 to 23.9 months. Coadministration of breastfeeding with solid/semi-solid food significantly decreased the odds of coexistence of underweight with stunting by 16% (1 to 29%) compared to underweight children (Table 3).
Determinants of Coexistence of underweight with both wasting and stunting
On multivariate analysis, we found a significantly lower odds of coexistence of underweight with both wasting and stunting in children adherent to MDD, MFF, iron and folate rich diet, EFF, and with overall CF adherence, compared with a normal child (Table 2). However, no relationship of coexistence of underweight with both wasting and stunting with all CF indicators was reported, when compared with underweight child (Table 3).
Determinants of Coexistence of stunting with overweight/obesity
Compared to a normal child, continuation of breastfeeding, and coadministration of breastfeeding with solid/semi-solid food significantly increased the odds of coexistence of stunting with overweight/obesity (Table 2). Similarly, continuation of breastfeeding was significantly associated with coexistence of stunting with overweight/obesity, compared with stunted children (Table 3).
Interaction of various covariates with complementary feeding indicators among malnourished children
Interaction of child age with complementary feeding indicators
Consumption of breastmilk with solid/semi-solid/soft food in children aged between 18-23.9 months increased the odds of coexistence of stunting with overweight/obesity (OR = 2.21 (1.22 to 4.00), compared to children aged between 6-11.9 months. However, with other forms of CFM, the consumption of breastmilk with solid/semi-solid/soft foods did not show an association with child age.
An adherence to minimum dietary diversity (MDD) decreased the odds of coexistence of underweight with wasting and coexistence of underweight with stunting by 0.38 (0.16 to 0.91) and 0.36 (0.16 to 0.83), respectively in children aged between 12-17.9 months, compared to children aged between 6-11.9 months. Similarly, adherence to MDD lowered the odds of coexistence of underweight with stunting in older children aged between 18-23.9 months by 0.34 (0.15 to 0.77)
Compared to young children aged between 6-11.9 months, use of iron & folate supplementation in children aged over 12 months reduced the odds of coexistence of underweight with wasting to 0.47 (0.25 to 0.86), while the use of vegetables & fruits reduced the odds of coexistence of underweight with wasting to 0.57 (0.35 to 0.93) in children aged between 12-17.9 months. Additionally, the use of vegetables & fruits in children aged between 12-17.9 months reduced the odds of coexistence of underweight with stunting by 0.60 (0.38 to 0.95), compared with children below 12 months. However, in older children aged over 18 months, the practice of vegetables & fruits uses in children increased the odds of coexistence of stunting with overweight/obesity by two-folds (1.98, 95% CI: 1.09 to 3.59) (Supplementary file 6, Table-S-6-A).
Interaction of child sex with complementary feeding indicators
Coadministration of breastmilk with solid/semi-solid/soft food in children lowered the odds of coexistence of underweight with wasting by 0.68 (0.47 to 0.97) in female children, compared with male children. However, with other types of CFM, the coadministration of breastmilk with solid/semi-solid/soft foods showed no association with child sex.
Similarly, the association of CFM with other CF indicators, such as continuation of breastmilk, MDD, MMF, MAD, use of iron & folate supplementation, egg & flesh consumption, and vegetable & fruit diet did not differ by child sex (Supplementary file 6, Table-S-6-B).
Interaction of child health status with complementary feeding indicators
Paediatric CFM was not associated with different CF indicators irrespective of their health status (Supplementary file 6, Table-S-6-C).
Interaction of maternal education with complementary feeding indicators
The association between the coexistence of underweight with wasting and all CF indicators was not affected by maternal education. Similarly, maternal education showed no association between the coexistence of underweight with stunting and different CF indicators. Adherence to MAD was associated with reduced odds of coexistence of underweight with both wasting & stunting in children of mothers with secondary/higher education by 0.58 (0.35 to 0.95), compared to the children of uneducated (none) mothers. Similarly, certain CF practices, such as continuation of breastmilk, coadministration of breastmilk with solid/semi-solid/soft foods, and adherence to MMF significantly reduced the odds of coexistence of stunting with overweight/obesity among children of educated mothers, compared to the children of uneducated mothers (Supplementary file 6, Table-S-6-D).
Interaction of socioeconomic status with complementary feeding indicators
In general, an adherence to the complementary feeding practices showed no association with any form of paediatric CFM and socioeconomic status.
Among different feeding indicators, coadministration of breastmilk with solid/semi-solid/soft foods was associated to reduce the odds of coexistence of underweight with stunting and coexistence of stunting with overweight/obesity by 0.52 (0.31 to 0.90) and 0.39 (0.18 to 0.83) in poorer and richest children, respectively, compared with children of the poorest socioeconomic class. On the other hand, it was associated to increase the odds of coexistence of underweight with wasting and underweight with both wasting & stunting by tw0-folds. Besides coadministration of breastmilk with solid/semi-solid/soft foods, adherence to MMF was associated to increase the odds of coexistence of underweight with wasting and underweight with both wasting & stunting among poorer children compared to poorest children. However, relationship of other feeding indicators with any forms of CFM in children of different socioeconomic strata was not observed (Supplementary file 9.6, Table-S-9.6-E).
Interaction of type of place of residence with complementary feeding indicators
The place of residence had no significant effect on the association between CF indicators and various forms of CFM (Supplementary file 6, Table-S-6-F).
Discussion
To the best of our knowledge, this is the first study which has extensively explored the association of different CF indicators and CFM in children aged between 6 to 23.9 months. We found a protective role of CF adherence for the prevention and control of various forms of paediatric undernutrition, such as coexistence of underweight with wasting, coexistence of underweight with stunting, and coexistence of underweight with both wasting and stunting. In general, less than half of the children were adherent to most of the CF indicators, except continuation of BF, coadministration of solid, semi-solid, soft, & liquid foods with breastmilk, and MMF. Non-adherence to most of the CF indicators was associated with the higher odds of CFM in children aged between 6 to 23.9 months.
The introduction of solid, semi-solid, soft, & liquid foods with breastmilk is one of the core CF indicators prescribed by the WHO for all children aged between 6 to 23.9 months (United Nations Children Funds 2018) . However, our study did not show a protective effect of breastfeeding with various forms of CFM. Rather, we found a high risk of stunting with the continuation of BF either with or without SSF. The high risk of stunting with continuation of BF with or without SSF was reported irrespective of body weight (normal weight, underweight, and overweight/obese). Other studies have also found two-to-three-fold higher odds of paediatric stunting in children receiving breastmilk during CF period, compared to non-breastfed children (Cetthakrikul et al. 2018; Marquis et al. 1997; Syeda et al. 2021). Continuation of breastfeeding during the second year of life results in stunting despite age-appropriate CF initiation (Klag et al. 2015; Syeda et al. 2021). The high risk of stunting in children aged over six-months might be attributable to delayed initiation of solid & semi-solid food or due to the non-adherence of complementary feeding practices (Syeda et al. 2021). However, our previous study demonstrated that early initiation of solid, semi-solid, soft & liquid food before the prescribed age of 6 to 8 months is associated with an increase in the odds of various forms of coexisting forms of undernutrition, such as coexistence of underweight with wasting, coexistence of underweight with stunting, and coexistence of underweight with both wasting & stunting (Khaliq et al. 2021). Previous studies have demonstrated a protective role of protein containing food against paediatric stunting (Khamis et al. 2019; Reinbott and Jordan 2016). A study by Khamis et al. reported that stunting in children can be averted by increasing the consumption of animal proteins, such as egg, meat, fish, and organ meats (Khamis et al. 2019). Similarly, a randomized controlled trial conducted in Ethiopia also proposed use of animal proteins for the prevention of various forms of nutritional disorders (Reinbott and Jordan 2016).WHO in the recent IYCF guidelines of 2021 introduced a new indicator EFF for assessing the consumption of protein obtained from animal sources (World Health Organization 2021). Our study showed 29.5% adherence of EFF, and its adherence is associated to reduce the odds of various forms of paediatrics undernutrition, including coexisting forms of undernutrition (underweight with wasting, underweight with stunting, and underweight with both wasting & stunting). Thus, incorporation of animal containing food can avert the onset of various forms of paediatric undernutrition.
Our findings suggest that cereals & grains and dairy products were chiefly used for CF, whereas the consumption of food from other food groups (nuts & legumes, eggs, fish & meat, vitamin A containing fruits & vegetables, and other fruits & vegetables) was less than 30%. Similarly, a joint report of Government of Pakistan, UNICEF and UK-aid reported that cereals and dairy products were used as a main source of CF in Pakistan, with deprivation of feeding from other food groups (National Institute of Population Sciences 2018). Our study explored the root cause of high prevalence of paediatric malnutrition through two different but interconnected pathways. Firstly, the excessive use of cereals & grains, and dairy products, and restricted use of food from fruits, vegetables, meats, eggs, and legumes & nuts predispose a child towards various forms of nutritional disorders. Secondly, the use of food chiefly from two food groups (cereals & grains, and dairy products) leads to sequential non-adherence of MDD and MAD, which in turn results in paediatric malnutrition, including CFM. Many previous studies have discussed the roles of different food groups and feeding practices for the alleviation of paediatric malnutrition (Kinyoki et al. 2016; Rachmi et al. 2016). Food containing eggs, flesh, and nuts & legumes are rich in protein and different studies suggested the use of proteins for the alleviation of paediatric undernutrition, such as wasting, and stunting (Rachmi et al. 2016; Reinbott and Jordan 2016). Similarly, an adequate consumption of fruits and vegetables is effective in preventing various forms of malnutrition, including micronutrient deficiencies (Kinyoki et al. 2016). Therefore, the recent IYCF guidelines proposed a new CF indicator “ZVF” for assessing the population of children non-adherent to vegetable and fruits consumption (World Health Organization 2021). Our study reported that more than 40% of children did not consume either fruit or vegetables in the last 24 hours. The findings of our study were comparable to other studies, which reported the fruits and vegetable consumption for only a third of children (Cooke et al. 2004). The low consumption of fruits and vegetables is a global concern, and it occurs due to poor quality and high pricing of fruits and vegetables (Cooke et al. 2004; Saxe-Custack et al. 2019). Compared to global inflation estimates, Pakistan has historically reported an average of 8.2% higher inflation rate for the last fifty to sixty years (WorldDate.info 2022). The high inflation rate in Pakistan has tremendously diminished the purchasing power to food, and due to this reason, the inflation drastically affects food affordability (Qayyum et al. 2018). In this regard, there is a need to alleviate malnutrition at both a macro as well as a microlevel. At a macro level, malnutrition can be averted by providing food fortification, and food subsidiary to underprivileged households. However, at a microlevel, the nutritional disorders in children can be averted by increasing adherence to CF practices, nutritional counseling of caregivers, and multicomponent interventions, such as experimental, behavioral, psychological, and educational (Buyuktuncer et al. 2014; Hodder et al. 2020).
Our study reported lower odds of various types of undernutrition, such as wasting, underweight, stunting, underweight with stunting and underweight with both wasting & stunting among MDD and MMF adherent children. Similarly, studies conducted in Cambodia, China, Ethiopia, Haiti, India, Malawi, Mali, Nepal, Peru, Rwanda, Tanzania, Thailand and Zimbabwe also supported that an adherence to MDD and MMF significantly improved nutritional outcomes, and protected infants and young children from various types of undernutrition, including coexisting forms of undernutrition (Aemro et al. 2013; Arimond et al. 2004; Benedict et al. 2021; Feng et al. 2022; Khamis et al. 2019; Reinbott and Jordan 2016; Solanki et al. 2022). Conversely, our study reported a higher odds of overweight/obesity in MMF adherent children. However, a study conducted in Thailand showed no association of MMF with overweight/obesity, and low probability of overweight/obesity among MDD adherent children (Benedict et al. 2021). Hence, an improvement in dietary diversity can curtail both undernutrition and overnutrition in children. The dietary diversity and meal frequency in the paediatric diet can be augmented by improving maternal education and awareness regarding the timing and importance of infants and young child feeding indicators (Wuneh et al. 2019). This was evidenced by a RCT conducted by Reinbott & Jordan that nutrition education is directly associated to improve infant feeding practices (Reinbott and Jordan 2016).
IYCF guidelines suggested an acceptable diet is essential for the growth and nourishment of all children (United Nations Children Funds 2018). The acceptable diet of a child is a measure of MDD and MMF. Children who are adherent to both MDD and MMF are referred to as MAD adherent. Our study reported a lower odds of underweight among children adherent to MAD. An underweight child poses a serious threat for various forms of CFM (World Health Organization 2020a). Similarly, a study by Walters, et al., demonstrated that an adherence to MAD serves to protect children from being underweight (Walters et al. 2019). We found 18.9% MAD adherence, while other studies conducted in various parts of Asia and Africa have reported MAD adherence of 33% in Democratic Republic of Congo (Kambale et al. 2021), 4.1% to 32% in Ethiopia (Molla et al. 2021; Mulat et al. 2019), 8.4% in India (Acharya et al. 2021), 4.4% to 8.4% in Philippines (Guirindola et al. 2018), and 12% in Malawi (Walters et al. 2019). Different studies support that an increase in maternal education, maternal empowerment, and knowledge regarding infant feeding indicators can augment MAD adherence (Mulat et al. 2019; Walters et al. 2019). In a study by Guirindola, et al., breastfed children showed comparatively higher MAD adherence than non-breastfed children (Guirindola et al. 2018). Thus, continuation of breastfeeding during the first two-years of life may also help to improve the adherence to MAD. Furthermore, the adherence to MAD can be improved by augmenting adherence to MDD and MFF.
Our study reported a protective role of iron & folate (IFA) adherence against various types of undernutrition, including coexisting forms of undernutrition. Use of diet enriched with IFA is essential for the growth and development of every child, even during prenatal period (Allali et al. 2017; Stephenson et al. 2018). Despite having myriads of health and nutritional benefits of IFA food, our study reported that the diet of less than 30% children contains IFA containing food. Deficiency of IFA in an individual results in anemia (Oh et al. 2020), and anemia during early infancy and childhood results in impaired growth and development, including developmental delay (Allali et al. 2017). Moreover, anemia in children also leads to decreased intellectual capability, altered cardiac function, and various diseases, such as stroke (Allali et al. 2017; Zavaleta and Astete-Robilliard 2017). Some of the problems relating to health and nutrition can be averted by use of those foods enriched with IFA, such as meat, fish, dark green vegetables, and legumes & nuts (IndiKit 2022). Unfortunately, around 22% of Pakistani people live below the poverty line and are less able to buy food rich in IFA. In this regard, food fortification is very useful, cost-effective, and widely acceptable intervention for the prevention and control of various types of micronutrients disorders (Tong and Walker 2021).
Study strengths, weaknesses, and future direction
Our study examined the relationship of each CF indicator with CFM and is the first to measure the association of CFM with CF indicators including the newly introduced CF indicators published in 2021 IYCF guidelines. Moreover, the use of eight nationally and regionally representative datasets, and large sample size further strengthen the internal validity of our study. Despite various strengths of this study, our study revealed some counterintuitive findings related to the association of coadministration of breastmilk with SSF and adherence to MMF among children of different socioeconomic strata. Similarly, our study also showed higher odds of stunting among breastfeed children and in children taking breastmilk with SSF. However, all the health regulatory bodies promoted the use of breastmilk for children aged between 0 to 23.9 months for their optimal growth and nutrition (World Health Organization 1991, 2010, 2021). In this regard, it is essential to explore the underlying reasons for the counterintuitive findings. The reason for counterintuitive findings can be investigated by strengthening the study design and data collection methods.
In our study, the information related to the feeding indicators were collected qualitatively via a set of questionnaires, which asked about the intake of different food groups including milk and dairy products from the mothers of children aged below two years. The information related to food intake collected was entirely based on maternal verbal response. However, the relationship of CFM with food portion size, and of calories intake was not assessed, because the datasets used in this study were devoid of these variables. Moreover, this study did not examine the influence of seasonal diet variation, food insecurity, and various other socioeconomic and climatic adversities, such as poverty, unemployment, inflation, food pricing, food subsidiary, food acceptability, food taste, famine, drought, and cultural practices of infant feeding. Longitudinal or interventional study may further explore the relationship of different food types, food quantity and calories intake with various types of CFM, to ultimately devise a national nutrition guideline for the prevention and control of various forms of CFM. This study examined CFM only via anthropometric measurement. There is a persistent need to investigate the relationship of each type of CFM with various forms of micronutrient deficiencies by observing clinical signs and symptoms. A holistic approach for the diagnosis of various types of CFM can help to identify the underlying causes of malnutrition in children.
Recommendation and policy implications
The findings of our study supported that adherence to MDD, MMF, use of protein, and IFA can effectively protect a child from various forms of paediatric undernutrition, including CFM. On the other hand, use of breastmilk either alone or in conjunction with SSF was associated with increased odds of stunting in all children irrespective of their weight status, i.e., normal, underweight, and overweight/obese, thereby increasing the odds of both standalone forms of malnutrition and CFM. However, IYCF guidelines, American Association of Paediatrics (AAP), and various other local guidelines also suggested use of breastmilk for better growth and development of children aged below two years (Eidelman et al. 2012; World Health Organization 2021). Further research is needed to substantiate the associations between each CF indicator and CFM.
Based on the findings of this study, it is essential to promote the accessibility of national dietary & nutrition guidelines among the general population, to in turn improve the knowledge and practices about the utilization of different food groups according to caloric requirements. An improvement in the knowledge and practices about different food groups, portion size, and caloric intake will ultimately aid in the prevention & control of various forms of CFM in children aged between 6 to 23.9 months.
Conclusions
Children aged between 6 to 23.9 months have the highest risk of various forms of nutritional disorders, including CFM. In Pakistan, cereals and dairy are two major group of food used in children for CF, while the consumption of meat, egg, vegetables, fruits, and legumes & nut was evident in less than 30 percent. Most of the CF indicators, when practiced according to the infant feeding guidelines have the potential to avert both standalone forms of undernutrition as well as coexisting forms of undernutrition. However, use of breastmilk either alone or in conjunction with SSF showed no association with CFM, and an increased odds of stunting irrespective of child weight, i.e., normal, underweight, and overweight/obese. For tackling paediatric undernutrition, it is essential to employ dual methods of parental education about CF adherence and its importance alongside environmental change. An improvement in MDD, MMF, MAD, use of protein, and IFA can alleviate various forms of paediatric undernutrition, including coexisting forms of paediatric undernutrition. However, at a population level, food fortification can aid in reducing the burden of various forms of nutritional disorders, including micronutrient deficiencies.
References
Acharya A, Pradhan MR, Das AK (2021) Daterminants of minimum acceptable diet feeding among children aged 6-23 months in Odisha. Public Health Nutr, India. https://doi.org/10.1017/S1368980021002172
Aemro M, Mesele M, Birhanu Z, Atenafu A (2013) Dietary diversity and meal frequency practices among infant and young children aged 6–23 months in Ethiopia: a secondary analysis of Ethiopian demographic and health survey 2011. J Nutr Metabol 2013:1–8. https://doi.org/10.1155/2013/782931
Allali S, Brousse V, Sacri AS, Chalumeau M, de Montalembert M (2017) Anaemia in children: prevalence, causes, diagnostic work-up, and long-term consequences. Expert Rev Hematol. https://doi.org/10.1080/17474986.2017.1354696
Arimond M, Ruel MT (2004) Dietary diversity is associated with child nutritional status: evidence from 11 demographic and health surveys. J Nutr 134(10):2579–2585
Benedict L, Hong SA, Winichagoon P, Tejativaddhana P, Kasemsup V (2021) Double burden of malnutrition and its association with infant and young child feeding practices among children under-five in Thailand. Public Health Nutr 24(10):3058–3065
Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, Webb P, Lartey A, Black RE (2013) Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. https://doi.org/10.1016/S0140-6736(13)60996-4
Buyuktuncer Z, Kearney M, Ryan CL, Thurston M, Ellahi B (2014) Fruit and vegetables on prescription: a brief intervention in primary care. J Hum Nutr Diet 27:186–193
Cetthakrikul N, Topothai C, Suphanchaimat R, Tisayaticom K, Limwattananon S, Tangcharoensathien V (2018) Childhood stunting in Thailand: when prolonged breastfeeding interacts with household poverty. BMC Pediatr. https://doi.org/10.1186/s12887-018-1375-5
Cooke L, Wardle J, Gibson E, Sapochnik M, Sheiham A, Lawson M (2004) Demographic, familial and trait predictors of fruit and vegetable consumption by pre-school children. Public Health Nutr 7(2):295–302
Dagne AH, Anteneh KT, Badi MB, Adhanu HH, Ahunie MA, Tebeje H, Demewozu M, Aynalem GL (2019) Appropriate complementary feeding practice and associated factors among mothers having children aged 6-24 months in Debre Tabor Hospital, North West Ethiopia, 2016. BMC Res Notes. https://doi.org/10.1186/s13104-019-4259-3
De-Vries I, Breugem C, Van-der HA, Eijkemans M, Kon M, van-der MA (2014) Prevalence of feeding disorders in children with cleft palate only: a retrospective study. Clin Oral Invest. https://doi.org/10.1007/s00784-013-1117-x
Dhami MV, Ogbo FA, Osuagwu UL, Agho KE (2019) Prevalenceand factors associated with complementary feeding practices among children aged 6–23 months in India: a regional analysis. BMC Public Health 19(1):1–16
Eidelman AI, Schanler RJ, Johnston M, Landers S, Noble L, Szucs K, Viehmann L (2012) Breastfeeding and the use of Human Milk. Pediatr. https://doi.org/10.1542/peds.2011-3552
Feng J, Gong Z, Wang Y, Huo J, Zhuo Q (2022) Complementary feeding and malnutrition among infants and young children aged 6–23 months in rural areas of China. Nutrients 14(9):1807
Global Nutrition Report (2018) The Burden of Malnutrition. https://globalnutritionreport.org/reports/global-nutrition-report-2018/burden-malnutrition/. Accessed 18 August 2020
Global Nutrition Report (2019) Global overview: Malnutrition buden. Global Nutrition Report. https://globalnutritionreport.org/resources/nutrition-profiles/. Accessed 18 August 2020
Global Nutrition Report (2021) Country Nutrition Profiles. https://globalnutritionreport.org/resources/nutrition-profiles/. Accessed 21 May 2021
Goday PS, Huh SY, Silverman A, Lukens CT, Dodrill P, Cohen SS, Delaney AL, Fueling MB, Noel RJ, Gisel E (2019) Pediatric feeding disorder: consensus definition and conceptual framework. J Pediatr Gastroentrol Nutr. https://doi.org/10.1097/MPG.0000000000002188
Guirindola MO, Maniego MLV, Silvestre CJ, Acuin CCS (2018) Determinants of meeting the minimum acceptable diet among Filipino children aged 6-23 months. Philipp J Sci 147(1):75–89
Hodder RK, O'Brien KM, Tzelepis F, Wyse RJ, Wolfenden L (2020) Interventions for increasing fruit and vegetable consumption in children aged five years and under. Cochrane Database of Systematic Reviews (5)
IndiKit (2022) Consumption of Iron-Rich Foods Among Children. https://www.indikit.net/indicator/1-nutrition/274-consumption-of-iron-rich-foods-among-children. Accessed 08 October 2022
Jones G, Steketee RW, Black RE, Bhutta Z, Morris SS (2003) How many child deaths can we prevent this year? Lancet. https://doi.org/10.1016/S0140-6736(03)13811-1
Kambale RM, Ngaboyeka GA, Kasengi JB, Niyitegeka S, Cinkenye BR, Baruti A, Mutuga KC, Vander Linden D (2021) Minimum acceptable diet among children aged 6–23 months in south Kivu, Democratic Republic of Congo: a community-based cross-sectional study. BMC Pediatr. https://doi.org/10.1186/s12887-021-02713-0
Khaliq A, Wraith D, Miller Y, Nambiar-Mann S (2021) Prevalence, Trends, and Socioeconomic Determinants of Coexisting Forms of Malnutrition Amongst Children under Five Years of Age in Pakistan. Nutrients. https://doi.org/10.3390/nu13124566
Khaliq A, Wraith D, Miller Y, Nambiar S (2022a) Association of Infant Feeding Indicators and Infant Feeding Practices with Coexisting Forms of Malnutrition in Children under Six Months of Age. Nutrients. https://doi.org/10.3390/nu14204242
Khaliq A, Wraith D, Nambiar S, Miller Y (2022b) A review of the prevalence, trends, and determinants of coexisting forms of malnutrition in neonates, infants, and children. BMC Public Health. https://doi.org/10.1186/s12889-022-13098-9
Khamis AG, Mwanri AW, Ntwenya JE, Kreppel K (2019) The influence of dietary diversity on the nutritional status of children between 6 and 23 months of age in Tanzania. BMC Pediatr. https://doi.org/10.1186/s12887-019-1897-5
Kinyoki DK, Kandala NB, Manda SO, Krainski ET, Fuglstad GA, Moloney GM, Berkley JA, Noor AM (2016) Assessing comorbidity and correlates of wasting and stunting among children in Somalia using cross-sectional household surveys: 2007 to 2010. BMJ Open. https://doi.org/10.1136/bmjopen-2015-009854
Klag EA, McNamara K, Geraghty SR, Keim SA (2015) Associations between breast milk feeding, introduction of solid foods, and weight gain in the first 12 months of life. Clin Pediatr. https://doi.org/10.1177/0009922815569202
Korir JK (2013) Determinants of complementary feeding practices and nutritional status of children 6-23 months old in Korogocho slum, Nairobi County, Kenya. Dissertation. Kenyatta University
Marquis GS, Habicht JP, Lanata CF, Black RE, Rasmussen KM (1997) Association of breastfeeding and stunting in Peruvian toddlers: an example of reverse causality. Inter J epidemio. https://doi.org/10.1093/ije/26.2.349
Martorell R (2017) Improved nutrition in the first 1000 days and adult human capital and health. American J Human Bio 29(2):e22952. https://doi.org/10.1002/ajhb.22952
Molla A, Egata G, Getacher L, Kebede B, Sayih A, Arega M, Bante A (2021) Minimum acceptable diet and associated factors among infants and young children aged 6–23 months in Amhara region, Central Ethiopia: community-based cross-sectional study. BMJ Open. https://doi.org/10.1136/bmjopen-2020-044284
Mulat E, Alem G, Woyraw W, Temesgen H (2019) Uptake of minimum acceptable diet among children aged 6–23 months in orthodox religion followers during fasting season in rural area, DEMBECHA, north West Ethiopia. BMC Nutri. https://doi.org/10.1186/s40795-019-0274-y
National Institute of Population Sciences (2018) UNICEF. Complementary feeding practices in Pakistan an in-depth analysis of PDHS 2012-13. https://www.unicef.org/pakistan/media/1496/file/Complementary%20feeding%20practices%20in%20Pakistan.pdf. Accessed on 7 August 2019
National Institute of Population Studies (2019) Pakistan Demographic and Health Survey 2017-18. http://dhsprogram.com/pubs/pdf/FR354/FR354.pdf. Accessed 04 July 2019
Neu J (2007) Gastrointestinal development and meeting the nutritional needs of premature infants. The American J Clin Nutri. https://doi.org/10.1093/ajcn/85.2.629S
Oh C, Keats EC, Bhutta ZA (2020) Vitamin and mineral supplementation during pregnancy on maternal, birth, child health and development outcomes in low-and middle-income countries: a systematic review and meta-analysis. Nutrients. https://doi.org/10.3390/nu12020491
Qayyum A, Sultana B (2018) Factors of food inflation: Evidence from time series of Pakistan. J Bank Financ Manag 1(2):23–30
Rachmi CN, Agho KE, Li M, Baur LA (2016) Stunting coexisting with overweight in 2· 0–4· 9-year-old Indonesian children: prevalence, trends and associated risk factors from repeated cross-sectional surveys. Public Health Nutr. https://doi.org/10.1017/S1368980016000926
Ramachandran P (2015) Maternal and child nutrition: The first 1,000 days. Indian J Med Res 142(2):231
Reinbott A, Jordan I (2016) Determinants of child malnutrition and infant and young child feeding approaches in Cambodia. World Rev Nutr Diet. https://doi.org/10.1159/000444609
Sadhu G, Hemangini G (2020) COVID-19’s Shadow on Undernourished Children (6–23 months): An Evidence-Based Study on Magnitude and its Determinants in Rajasthan. J Hlth Mgmt. https://doi.org/10.1177/0972063420983094
Saxe-Custack A, LaChance J, Hanna-Attisha M (2019) Child consumption of whole fruit and fruit juice following six months of exposure to a pediatric fruit and vegetable prescription program. Nutrients 12(1):25
Scott JA (2020) The first 1000 days: A critical period of nutritional opportunity and vulnerability. Nutri Dietetics. https://doi.org/10.1111/1747-0080.12617
Solanki KH, Parande MA, Salunke NM, Sangwan K, Tambe MP (2022) Association of minimum dietary diversity and minimum meal frequency with anthropometric parameters among children of 6 to 23 months of age attending immunization clinic of a tertiary care hospitals. Int J Commun Med Pub Health 9(1):166
Stephenson J, Heslehurst N, Hall J, Schoenaker DA, Hutchinson J, Cade JE, Poston L, Barrett G, Crozier SR, Barker M (2018) Before the beginning: nutrition and lifestyle in the preconception period and its importance for future health. Lancet. https://doi.org/10.1016/S0140-6736(18)30311-8
Syeda B, Agho K, Wilson L, Maheshwari GK, Raza MQ (2021) Relationship between breastfeeding duration and undernutrition conditions among children aged 0–3 Years in Pakistan. Inter J Pediatr Adoles Medi. https://doi.org/10.1016/j.ijpam.2020.01.006
Tong H, Walker N (2021) Current levels of coverage of iron and folic acid fortification are insufficient to meet the recommended intake for women of reproductive age in low-and middle-income countries. J of Glob Health. https://doi.org/10.7189/jogh.11.18002
United Nations Children Funds (2018) Infant and young child feeding. https://data.unicef.org/topic/nutrition/infant-and-young-child-feeding/. Accessed 10 November 2021
United Nations Children Funds (2019) National Nutrition Survey 2018: Key Finding Report. https://www.unicef.org/pakistan/national-nutrition-survey-2018. Accessed 04 August 2019
United Nations Development Programme (2020) Millennium Development Goals. https://www.undp.org/content/undp/en/home/sdgoverview/mdg_goals.html. Accessed 28 August 2022
Walters CN, Rakotomanana H, Komakech JJ, Stoecker BJ (2019) Maternal determinants of optimal breastfeeding and complementary feeding and their association with child undernutrition in Malawi (2015-2016). BMC Public Health. https://doi.org/10.1186/s12889-019-7877-8
White JM, Begin F, Kumapley R, Murray C, Krasevec J (2017) Complementary feeding practices: Current glonal and regional estimates. Matern Child Nutr. https://doi.org/10.1111/mcn.12505
World Health Organization (1991) Indicators for assessing breast-feeding practices: report of an informal meeting, 11-12 June 1991, Geneva, Switzerland. https://www.who.int/iris/bitstream/handle/10665/62134/WHO_CDD_SER_91.14.pdf;jse. Accessed 14 December 2019
World Health Organization (2010) Indicators for assessing infant and young child feeding practices part 3: country profiles. World Health Organization. https://www.who.int/iris/bitstream/handle/10665/44368/9789241599757_eng.pdf. Accessed 17 December 2019
World Health Organization (2020a) Malnutrition: Key facts. https://www.who.int/news-room/fact-sheets/detail/malnutrition. Accessed 14 June 2021.
World Health Organization (2020b) Nutrition: Global Targets 2025. https://www.who.int/nutrition/global-target-2025/en/ Accessed 07 September 2022
World Health Organization (2021) Indicators for assessing infant and young child feeding practices: definitions and measurement methods. https://www.who.int/iris/bitstream/handle/10665/340706/9789240018389-eng.pdf?sequence=1 Accessed 07 September 2022
Wuneh AG, Ahmed W, Bezabih AM, Reddy PS (2019) Dietary diversity and meal frequency practices among children aged 6–23 months in agro pastoral communities in Afar region, Ethiopia: a cross-sectional study. Ecol Food Nutr 58(6):575–596
Zavaleta N, Astete-Robilliard L (2017) Effect of anemia on child development: Long-term consequences. Revis Perua de Medici Experi Salu Public. https://doi.org/10.17843/rpmesp.2017.344.3251
Zhang Y, Huang X, Yang Y, Liu X, Wang A, Wang Y, Zhou H (2018) Double buden of malnutrition among chidlren under 5 in poor areas of China. PLOS One. https://doi.org/10.1371/journal.pone.0204142
Zhou H, Wang WL, Ye F, Zeng XL, Wang Y (2012) Relationship between child feeding practices and malnutrition in 7 remote and poor countries. Asia Pacif J Clin Nutr, PR China. https://doi.org/10.3316/ielapa.301154323680038
Acknowledgments
We would like to acknowledge the data archivist of the Demographic and Health Surveys (DHS) Program and UNICEF, who provided access to the datasets of all the Demographic and Health Surveys (DHS) and Multiple Indicator Cluster Surveys (MICS) implemented in Pakistan for analysis.
Data availability statement
The data from this study can be retrieved from the DHS program (www.dhsprogram.com) and UNICEF (www.mics.unicef.org/surveys).
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions This manuscript is a product of the Ph.D. Thesis of A.K., who received a High Degree Research (HDR) scholarship and Queensland University of Technology Postgraduate Research Award (QUTPRA) scholarship for his Ph.D. A.K. and the team have applied for covering the publication costs for this paper. The APC (Article Processing Charge) was funded by the Queensland University of Technology.
Author information
Authors and Affiliations
Contributions
This research paper is part of the Ph.D. Thesis of A.K. The idea of this project was conceptualized by A.K. The data management, data analysis, and original draft writing were performed by A.K.; D.W. assisted and supervised A.K. with data analysis. Y.M. and S.N. provided technical support based on their expertise. The paper has been reviewed and edited by D.W., Y.M. and S.N. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Institutional review board statement
The project of this study was approved by the Queensland University of Technology Human Research Ethics Committee (UHREC). The approval number of this project was 2000000177.
Informed consent statement
In this study, the research team received data from DHS and UNICEF repository which was de-identified, i.e., it does not contain information in which a participant can either be identified or traced by any means. Due to this reason, this study does not involve a statement for informed consent.
Conflicts of interest
The authors declare no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
WHAT IS ALREADY KNOWN ON THIS TOPIC:
The first thousand days of life, from conception to two years of age, are crucial for the growth and nourishment of a child. For optimizing the health & nutrition outcome of children aged between 0 to 23.9 months, both the World Health Organization (WHO) and UNICEF proposed a joint guideline, entitled: ‘Infant & Young Child Feeding (IYCF)’. An adherence to IYCF indicator showed promising health & nutrition outcome and protect children from various types of nutritional disorders. However, the relationship of complementary feeding indicators with the various types coexisting forms of malnutrition (CFM) has not been examined anywhere so far.
WHAT THIS STUDY ADDS:
The prevalence of CFM in children aged between 6 to 23.9 months is 1.5 folds higher than the prevalence of standalone forms of malnutrition (CFM = 28.1% ~ SFM =18.2%). Adherence to minimum dietary diversity (MDD) and minimum meal frequency (MMF) reduce the odds of various forms of CFM. Similarly, an exposure to egg & flesh food and iron & folate supplementation also aids to reduce the odds of various forms of CFM in children aged between 6 to 23.9 months. The odds of CFM increased to around 1.5 folds after first birthday. However, an improvement in maternal education and socioeconomic status serve to reduce the odds of various forms of CFM.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY:
The accelerated burden of CFM in children can be averted by promoting the use of various types of foods, such as egg, flesh foods, and iron & folate. Moreover, there is need to educate mother/caregiver about the basics of MDD and MMF.
Supplementary Information
ESM 1
(DOCX 82 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khaliq, A., Nambiar, S., Miller, Y. et al. Adherence to complementary feeding indicators and their associations with coexisting forms of malnutrition in children aged between 6 to 23.9 months of age. J Public Health (Berl.) (2023). https://doi.org/10.1007/s10389-023-02054-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-023-02054-5