Abstract
Background
We aimed to estimate the global burden of colorectal cancer (CRC) between 1990 and 2019.
Methods
Data were extracted from the Global Burden of Disease study 2019. Estimated annual percentage changes (EAPCs) were calculated to quantify temporal trends in the age-standardized rates of CRC incidence, deaths, and disability-adjusted life-years (DALYs) by age, sex, region, and country. The correlations of EAPCs in the age-standardized rates with sociodemographic index (SDI) were also analyzed.
Results
From 1990 to 2019, the CRC incidence, deaths, and DALYs increased worldwide by 157%, 110%, and 96%, respectively. The global age-standardized incidence rate increased (EAPC, 0.58; 95% confidence interval [CI], 0.51–0.66), whereas both the age-standardized death rate (EAPC, −0.21; 95% CI, −0.28 to −0.14) and age-standardized DALY rate (EAPC, −0.21; 95% CI, −0.26 to −0.15) presented downward trends. As for regions, the largest increases in the age-standardized incidence rate, age-standardized death rate, and age-standardized DALY rate were observed in East Asia. In terms of countries, the largest increase in CRC incidence was found in Equatorial Guinea (3.98), followed by Vietnam (3.79) and China (3.66). The age-standardized incidence rate was higher in men than in women. Negative correlations were found between the EAPC in the age-standardized incidence rate of CRC and the SDI.
Conclusions
Future CRC preventive strategies should focus on the male population and older adults, especially in East Asia, Qatar, United Arab Emirates, Saudi Arabia, and other high-risk regions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Colorectal cancer (CRC) is the third most common cancer and the second most deadly cancer globally (Bray et al. 2018). In 2019, there were 1.8 million new CRC cases and more than 880,000 CRC-related deaths worldwide (Bray et al. 2018). Given the rapid aging of the global population and the increasing prevalence of risk factors, such as smoking, obesity, sedentary lifestyle, and unhealthy dietary habits, the epidemiological trends in CRC might have changed (Botteri et al. 2020; Fitzmaurice et al. 2017; Kerr et al. 2017).
The Global Burden of Disease (GBD) study estimates a variety of metrics for several diseases annually, starting from 1990 (GBD 2019 Demographics Collaborators 2020; Yu and Hemminki 2020). The GBD estimates are also updated annually with improved modeling strategies and complemented by data sources (2020). The GBD data thus provide a unique opportunity for comparative assessments of long-term trends in CRC incidence, deaths, and disability-adjusted life-years (DALYs) between different countries and regions. A study reported that the global CRC incidence and mortality rates are rapidly rising in many low-income and middle-income countries (Arnold et al. 2017). However, to date, few studies have systematically investigated and compared changes in the long-term trends in CRC burden between different regions and sexes.
In this study, we performed an updated systematic analysis of the global, regional, and sex-specific CRC incidence, deaths, and DALYs from 1990 to 2019. The improved understanding of the epidemiological and geographic trends in these CRC estimates due to our findings may provide insights into the guidance for the design and development of national CRC control and prevention programs.
Methods
Data source
The annual data on CRC incidence, mortality, and DALYs were collected from the Global Burden of Disease (GBD) study 2019 (http://ghdx.healthdata.org/gbd-results-tool). The data from 204 countries and territories stratified by age and sex from 1990 to 2019 and can be visualized in the form of charts and graphs (2020). The 204 countries and territories were classified into five regions according to their sociodemographic index (SDI)—namely, low, low-middle, middle, high-middle, and high SDI—and also into 21 geographic areas. Meanwhile, we also assessed the trends in CRC estimates according to the following age stratification: 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, 85–89, 90–94, and > 95 years. We followed the Guidelines for Accurate and Transparent Health Estimates Reporting recommendations (Stevens et al. 2016). This study was performed in line with the principles of the Declaration of Helsinki. This study was approved by the Institutional Review Board of Ningbo No.2 Hospital and Informed consent of this study was waived because no identifiable information was included in the analyses. The data included in the GBD study were obtained primarily from censuses, household surveys, disease registries, health service utilization data, and vital statistics records.
Estimation framework
CRC incidence was estimated using DisMod-MR, a Bayesian meta-regression disease modeling tool (2020). The non-specific codes of all available data on mortality were corrected and used to estimate mortality rates for the causes of death listed in the GBD, including CRC (2020). The Cause of Death Ensemble model was used to estimate death rates by age, sex, year, and country (Liu et al. 2019). Years lived with disability (YLDs) were calculated as the product of disability weight and the prevalence of CRC. DALYs due to CRC were calculated as the sum of YLDs and the years of life lost due to premature death (2015). Final estimates were computed using the mean estimates across 1000 draws, and 95% uncertainty intervals (UIs) were specified on the basis of the 25th and 975th values across all 1000 draws.
Statistical analysis
Estimated annual percentage changes (EAPCs) were calculated to quantify trends in CRC incidence, deaths, and DALYs (Liu et al. 2019). EAPC is a summary and widely used measure of age-standardized rate trends over a specified time period. The natural logarithm of the regression line fitted to the age-standardized rate is y = a + bx + c, where x is the calendar year. EAPC is calculated as 100 × (exp(b) − 1), and its 95% confidence interval (CI) can also be obtained from a linear regression model. If the estimated EAPC and the lower bound of its 95% CI are both > 0, the age-standardized rate is considered to exhibit an increasing trend; in contrast, when both the estimated EAPC and the upper bound of its 95% CI are < 0, the age-standardized rate is considered to exhibit a decreasing trend. Otherwise, the age-standardized rate is considered stable. We further evaluated the associations of EAPCs in the age-standardized rates with SDI using Pearson correlation analysis. All of the analyses were conducted using R program (version 3.5.1).
Results
CRC worldwide
Globally, CRC incidence increased from 842,098 (95% uncertainty interval [UI], 810,407–868,574) in 1990 to 2,166,168 (95% UI, 1,996,297–2,342,842) in 2019, while related deaths increased from 518,126 (95% UI, 493,682–537,876) in 1990 to 1,085,797 (95% UI, 1,002,795–1,149,678) in 2019 (Tables 1 and 2). CRC was responsible for 24,284,087 DALYs (95% UI, 22,614,919–25,723,220) in 2019 (Table 3). According to these values, CRC incidence, deaths, and DALYs increased by 157%, 110%, and 96%, respectively, from 1990 to 2019 (Tables 1, 2, and 3).
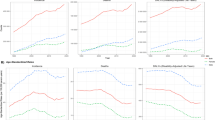
From 1990 to 2019, the age-standardized incidence rate of CRC showed an upward trend worldwide (EAPC, 0.58; 95% CI, 0.51–0.66), whereas the age-standardized death rate (EAPC, −0.21; 95% CI, −0.28 to −0.14) and age-standardized DALY rate (EAPC, −0.21; 95% CI, −0.26 to −0.15) presented a downward trend (Tables 1, 2, and 3, Fig. 1A–C, online supplemental Fig. 1). In addition, the age-standardized incidence rate for women (EAPC, 0.11; 95% CI, 0.03–0.19) and the age-standardized death rate (EAPC, 0.10; 95% CI, 0.03–0.17) and age-standardized DALY rate (EAPC, 0.13; 95% CI, 0.06–0.20) for men continued to increase, whereas the age-standardized death rate (EAPC, −0.59; 95% CI, −0.67 to −0.52) and age-standardized DALY rate (EAPC, −0.65; 95% CI, −0.71 to −0.60) for women showed a decreasing trend (Tables 1, 2, and 3, Fig. 1A–C, online supplemental Fig. 1).
The EAPC of colon and rectum cancer ASRs from 1990 to 2019, by sex and region. (A) The EAPC of ASIR. (B) The EAPC of ASDR. (C) The EAPC of age-standardized DALY rate. EAPC = estimated annual percentage change. ASRs = age-standardized rates. ASIR = age standardized incidence rate. ASDR = age standardized death rate. DALY = disability adjusted life-year
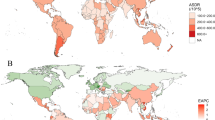
Furthermore, the age-standardized rates and their trends varied among different countries (Fig. 2A–F). The three countries with the largest increases in CRC incidence during 1990–2019 were Equatorial Guinea (3.98), Vietnam (3.79), and China (3.66) (online supplemental Table 3). Equatorial Guinea also showed the largest increase in CRC-related deaths (3.51) (online supplemental Table 4) as well as the largest increase in CRC-related DALYs (3.06) (online supplemental Table 5) from 1990 to 2019.
The global ASRs of colon and rectum cancer for both genders in 204 countries, and the global EAPC of colon and rectum cancer ASRs from 1990 to 2019, by countries. (A) The age standardized incidence rate. (B) The age standardized death rate. (C) The age-standardized DALY rate. (D) The EAPC of ASIR. (E) The EAPC of ASDR. (F) The EAPC of DALY rate. EAPC = estimated annual percentage change. ASRs = age-standardized rates. ASIR = age standardized incidence rate. ASDR = age standardized death rate. DALY = disability adjusted life-year
CRC incidence
At a global level, from 1990 to 2019, the age-standardized incidence rate of CRC in most countries presented an upward trend (online supplemental Table 3). It was higher in men than in women (male-to-female ratio, 1.26 in 1990 and 1.56 in 2019) (Table 1). As reported in online supplemental Table 1, the largest decrease in the age-standardized incidence rate was in Austria (total EAPC, −1.95; females EAPC, −2.04; males EAPC, −2.02), while the largest increase was in Equatorial Guinea (total EAPC, 3.98; females EAPC, 4.39; male EAPC, 3.62). The largest increase in the age-standardized incidence rate among men was in China (EAPC, 4.46). The region with the largest number change in CRC incidence during 1990–2019 was East Asia (5.67), whereas that with the smallest number change was Eastern Europe (1.51) (online supplemental Table 2).
As for various SDI quintiles, the fastest growth in the age-standardized incidence rate of CRC during 1990–2019 was observed in the middle SDI quintile (EAPC, 2.61; 95% CI, 2.44–2.78) (Table 1). High SDI countries had the highest age-standardized incidence rate (42.45 in 1990 and 42.78 in 2019), whereas low SDI countries had the lowest age-standardized incidence rate (6.20 in 1990 and 7.33 in 2019) (Table 1). The age-standardized incidence rates in the following SDI quintiles (high-middle, middle, low-middle, and low) continued to increase over time (Table 1).
However, the age-standardized incidence rate of CRC from 1990 to 2019 was higher in men than in women, as demonstrated by the male-to-female ratios of 1.26 and 1.56 in the respective years (Table 1). The male-to-female ratio of CRC incidence in different age groups showed a bimodal distribution, with a peak in the 65–69-year age group globally (online supplemental Fig. 2A).
The EAPC in the age-standardized incidence rate of CRC was found to be negatively correlated with the age-standardized incidence rate of CRC (ρ = −0.02, P = 0.59, online supplemental Fig. 3A) and the SDI of regions (ρ = −0.17, P < 0.001, online supplemental Fig. 3D). We also found that the higher the SDI of a region, the lower the proportion of incident cases of CRC in young people, and that regions in which SDI increased from 1990 and 2019 had a higher proportion of incident cases of CRC in older adults (online supplemental Fig. 4A and B). The annual proportions of CRC incidence in young people and older adults were relatively stable from year to year (online supplemental Fig. 5A). Age distribution of incidence (per 100,000) for colon and rectum cancer in different countries in 2019 are shown in online supplemental Table 6.
CRC-related deaths
As presented in Table S1, the top three countries with the highest age-standardized death rate in 2019 were Greenland (31.38), Brunei Darussalam (30.26), and Hungary (28.56), while those with the lowest age-standardized death rate were Bangladesh (4.94), Somalia (5.01), and Nepal (5.40). The largest decrease in the age-standardized death rate was in Austria (total EAPC, −2.81; females EAPC, −2.98; males EAPC, −2.86), while the largest increase was in Equatorial Guinea (total EAPC, 3.51; females EAPC, 3.91; males EAPC, 3.17) (online supplemental Table 1).
Among regions, Central Europe (23.57) and South Asia (7.29) had the highest and lowest age-standardized death rate, respectively (online supplemental Table 2). As presented in online supplemental Table 2, the largest increase in the age-standardized death rate was in East Asia (total EAPC, 1.40; males EAPC, 2.21), while the largest decrease was in Australasia (total EAPC, −1.73; females: EAPC, −1.72; males EAPC, −1.82). The largest increase in the age-standardized death rate among women was in South Asia (EAPC, 1.15).
As reported in Table 2, the age-standardized death rates increased only in the middle (EAPC, 1.24; 95% CI, 1.10–1.38), low-middle (EAPC, 1.15; 95% CI, 1.11–1.19), and low (EAPC, 0.58; 95% CI, 0.52–0.65) SDI quintiles. From 1990 to 2019, high SDI regions had the highest age-standardized death rates (21.18 in 1990 and 16.29 in 2019), while low SDI regions had the lowest age-standardized death rates (6.22 in 1990 and 7.33 in 2019). The largest decrease in the age-standardized death rate was in the high SDI quintile (EAPC, −1.09; 95% CI, −1.18 to −1.00).
The male-to-female ratio of CRC-related deaths in different age groups showed a bimodal distribution, with a peak in the 65–69-year age group globally (online supplemental Fig. 6). In addition, the EAPC in the age-standardized death rate was positively correlated with the SDI (ρ = 0.56, P < 0.001, online supplemental Fig. 3E). We also found that the higher the SDI of a region, the lower the proportion of CRC-related deaths in young people, and that regions in which SDI increased from 1990 and 2019 had a higher proportion of CRC-related deaths in older adults (online supplemental Fig. 4C and D). From 1990 to 2019, the annual proportion of death due to CRC in young people decreased, while that in older adults increased (online supplemental Fig. 5B). Age distribution of death rate (per 100,000) for colon and rectum cancer in different countries in 2019 are shown in online supplemental Table 7.
CRC-related DALYs
As shown in online supplemental Table 1, women in Greenland (639.09 in 2019) and men in Hungary (884.52 in 2019) had the highest DALYs in 2019. The largest decrease in the age-standardized DALY rate was in Austria (total EAPC, −3.09; females EAPC, −3.12; males EAPC, −3.19), while the largest increase was in Equatorial Guinea (total EAPC, 3.06; females EAPC, 3.52). Among men, the largest increase in the age-standardized DALY rate was in Vietnam (EAPC, 3.03).
The top three regions with the highest age-standardized DALY rate of CRC in 2019 were Central Europe (512.56), Southern Latin America (447.56), and Eastern Europe (423.70) (online supplemental Table 2), whereas those with the lowest age-standardized DALY rate were South Asia (165.06), Central sub-Saharan Africa (169.27), and Western sub-Saharan Africa (176.11) (online supplemental Table 2). The largest increase in the age-standardized DALY rate was in East Asia (total EAPC, 1.24; males EAPC, 2.09), while the largest decrease was in Australasia (total EAPC, −1.89; females EAPC, −1.90; males EAPC, −1.92). Among women, the EAPC was largest in Western sub-Saharan Africa (EAPC, 0.95) (online supplemental Table 2).
The highest age-standardized DALY rates of CRC were observed in high SDI regions in 1990 (454.74) but in high-middle SDI regions in 2019 (356.65). The lowest age-standardized DALY rates remained in the low SDI quintile in this period (146.24 in 1990 and 166.10 in 2019) (Table 3).
The male-to-female ratio of the age-standardized DALY rate of CRC across different age groups showed a bimodal distribution, with a peak in the 65–69-year age group globally (online supplemental Fig. 7). Positive correlations were found between the EAPC in the age-standardized DALY rate of CRC and the SDI (ρ = 0.56, P < 0.001, Fig. S3F). In 2019, low SDI regions had the highest proportion of CRC-related DALYs in young people (15–49 years), and regions in which SDI increased from 1990 to 2019 had a higher proportion of DALYs in older adults (online supplemental Fig. 4E and F). The annual proportions of CRC-related DALYs decreased in young people but increased from year to year in older adults (online supplemental Fig. 5C). Age distribution of DALYs (per 100,000) for colon and rectum cancer in different countries in 2019 are shown in online supplemental Table 8.
Discussion
In this study, we comprehensively analyzed the changing trends in CRC incidence, deaths, and DALYs at global, regional, and national levels by age, sex, and SDI from 1990 to 2019 based on data from the GBD study 2019. To that end, EAPCs in the age-standardized rates and the risk factors associated with CRC-associated DALYs and deaths were evaluated using the comparative risk assessment framework. From 1990 to 2019, CRC incidence, deaths, and DALYs increased worldwide by 157%, 110%, and 96%, respectively. Despite increases in the age-standardized incidence rate of CRC globally, the age-standardized death rate and age-standardized DALY rates among men and women decreased from 1990 to 2019. The increase in the absolute numbers of CRC cases and related categories is largely attributable to population growth and aging.
Globally, a rising trend was observed in the age-standardized incidence rate of CRC in most countries. Notably, the age-standardized incidence rate was higher in men than in women, which is consistent with the findings of a previous study (Lu et al. 2020). Compared with women, men are more strongly affected by CRC risk factors, such as smoking and drinking (Graff et al. 2017; Kerr et al. 2017; Wilsnack et al. 2009). Interestingly, the male-to-female ratio of CRC incidence, deaths, and DALYs showed a bimodal distribution with a peak in the 65–69-year age group, probably because most of the CRC cases were diagnosed between the ages of 65 and 68 years (Motsuku et al. 2021). CRC incidence in East Asia increased rapidly and significantly during 1990–2019 as countries in this region underwent rapid economic and societal changes during these decades. This is consistent with previous reports that CRC is more frequently diagnosed in more developed countries than in less developed countries (Ladabaum et al. 2020; Siegel et al. 2020).
Furthermore, the burden of CRC was found to differ greatly among different SDI quintiles. From 1990 to 2019, the age-standardized incidence rate in all SDI quintiles continued to increase, which could be attributable to the wide use of screening colonoscopy (Brenner et al. 2014). However, we found a significant positive correlation between the age-standardized incidence rate and SDI, which could be attributed to better diagnosis, the registry system, and population aging in developed countries (Arnold et al. 2017). Nevertheless, the fastest growth in the age-standardized incidence rate was observed in the middle SDI quintile, owing to rapid developments in society and medical technologies. Furthermore, negative correlations were observed between the EAPC in the age-standardized incidence rate and SDI, in addition to a higher proportion of incident cases among older adults in lower SDI regions. This suggests that more effective CRC prevention and treatment measures are warranted for older adults in low SDI regions.
The trends in CRC-related deaths and DALYs were also analyzed. Both deaths and DALYs showed increasing trends from 1990 to 2019. As for deaths, Greenland, Brunei Darussalam, and Hungary showed the highest age-standardized death rates, whereas Bangladesh, Somalia, and Nepal showed the lowest age-standardized death rates. Notably, the most pronounced decrease in the age-standardized death rate was found in Austria, this decline could be explained by Austria being a high SDI country with an advanced economy and medical infrastructure (Arnold et al. 2017; Lu et al. 2020).
Regionally, the largest increases in both the age-standardized incidence rate and age-standardized death rate were found in East Asia, which was consistent with one of the three trends in global CRC incidence and mortality reported is linked to the ongoing societal and economic development in this region (Arnold et al. 2017). Central Europe showed the highest age-standardized death rate, whereas South Asia showed the lowest age-standardized death rate. In addition, although the age-standardized death rate in South Asia was lowest, the age-standardized death rate among women in this region showed the largest increase, the reason for which remains unexplored. The largest decrease in the age-standardized death rate was in Australasia, which could partly be related to the adoption of best practices in CRC treatment and management to improve survival in this region (Arnold et al. 2017; Cammà et al. 2000; Center et al. 2009).
Globally, CRC-related deaths increased in all SDI quintiles; however, an increasing trend in the age-standardized death rates was only observed in the middle, low-middle, and low SDI quintiles, likely owing to inadequate medical resources and poor access to early detection and treatment in these regions (Goss et al. 2013). In contrast, a decreasing trend was observed in the age-standardized death rate in the high SDI quintile, which could be largely attributed to improvements in CRC screening technology. For example, since the 1990s, the USA, Israel, and Japan have implemented screening and early detection programs, which likely explains the decreasing trends in the age-standardized death rates observed in these countries (Schreuders et al. 2015). Further, from 1990 to 2019, a positive correlation was observed between the proportion of deaths due to CRC among older adults and the SDI, which could be attributed to population aging (Yang et al. 2013).
To the best of our knowledge, this study describes the latest epidemiologic patterns of CRC burdens at global, regional, and national levels by sex, age, and SDI. The strength of this study is its systematic use of data (from the GBD 2019 study) and methods to estimate the CRC burden in various regions throughout the world from 1990 to 2019. The results could be significant in guiding the design and development of national CRC control and prevention programs.
Nevertheless, the estimates obtained in the current study from the GBD data should be viewed with caution due to the following limitations. First, countries in the low SDI quintile might not have robust mortality reporting systems and population-based cancer registries, and one of the key limitations of the GBD study is that it is greatly affected by the lack of data on cancer registration. All of the data used in the current study were extracted from the GBD study, which were calculated from mathematical models rather than from the surveillance data itself. This might partly explain the differences in our findings with respect to some global studies (Araghi et al. 2019).
Finally, CRC is greatly affected by regional differences in diagnostic techniques and disease awareness, prevention, and multidisciplinary treatment strategies, such as surgery and chemotherapy. Thus, the results of our study should be interpreted cautiously.
Conclusions
Despite worldwide decreases in the age-standardized death rate and age-standardized DALY rate of CRC from 1990 to 2019, the values of these measures remained high during the study period in high-middle and middle SDI regions. In particular, East Asia, Equatorial Guinea, and Southern Latin America had the largest burden of CRC, and globally, CRC was more frequently reported in men than in women. Future CRC preventive strategies should therefore focus on the male population and older adults, especially in East Asia, Qatar, United Arab Emirates, Saudi Arabia, and other high-risk regions.
Data availability
Data can be obtained from the corresponding authors upon reasonable request.
Code availability
Not applicable.
Change history
03 March 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10389-023-01861-0
References
Araghi M, Soerjomataram I, Jenkins M, Brierley J, Morris E, Bray F, Arnold M (2019) Global trends in colorectal cancer mortality: projections to the year 2035. Int J Cancer 144:2992–3000. https://doi.org/10.1002/ijc.32055
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F (2017) Global patterns and trends in colorectal cancer incidence and mortality. Gut 66:683–691. https://doi.org/10.1136/gutjnl-2015-310912
Botteri E, Borroni E, Sloan EK, Bagnardi V, Bosetti C, Peveri G, Santucci C et al (2020) Smoking and colorectal cancer risk, overall and by molecular subtypes: a meta-analysis. Am J Gastroenterol 115:1940–9. https://doi.org/10.14309/ajg.0000000000000803
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Brenner H, Stock C, Hoffmeister M (2014) Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: systematic review and meta-analysis of randomised controlled trials and observational studies. BMJ 348:g2467. https://doi.org/10.1136/bmj.g2467
Cammà C, Giunta M, Fiorica F, Pagliaro L, Craxì A, Cottone M (2000) Preoperative radiotherapy for resectable rectal cancer: a meta-analysis. JAMA 284:1008–1015. https://doi.org/10.1001/jama.284.8.1008
Center MM, Jemal A, Ward E (2009) International trends in colorectal cancer incidence rates. Cancer Epidemiol Biomarkers Prev 18:1688–1694. https://doi.org/10.1158/1055-9965.Epi-09-0090
Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ et al (2017) Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol 3:524–548. https://doi.org/10.1001/jamaoncol.2016.5688
GBD 2019 Demographics Collaborators (2020) Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet (London, England) 396:1160–203. https://doi.org/10.1016/s0140-6736(20)30977-6
GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England) 396:1204–22. https://doi.org/10.1016/s0140-6736(20)30925-9
GBD 2013 Mortality and Causes of Death Collaborators (2015) Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 385:117–71. https://doi.org/10.1016/s0140-6736(14)61682-2
Goss PE, Lee BL, Badovinac-Crnjevic T, Strasser-Weippl K, Chavarri-Guerra Y, St Louis J, Villarreal-Garza C et al (2013) Planning cancer control in Latin America and the Caribbean. Lancet Oncol 14:391–436. https://doi.org/10.1016/s1470-2045(13)70048-2
Graff RE, Möller S, Passarelli MN, Witte JS, Skytthe A, Christensen K, Tan Q et al (2017) Familial risk and heritability of colorectal cancer in the Nordic Twin Study of Cancer. Clin Gastroenterol Hepatol 15:1256–1264. https://doi.org/10.1016/j.cgh.2016.12.041
Kerr J, Anderson C, Lippman SM (2017) Physical activity, sedentary behaviour, diet, and cancer: an update and emerging new evidence. Lancet Oncol 18:e457–e471. https://doi.org/10.1016/s1470-2045(17)30411-4
Ladabaum U, Dominitz JA, Kahi C, Schoen RE (2020) Strategies for colorectal cancer screening. Gastroenterology 158:418–432. https://doi.org/10.1053/j.gastro.2019.06.043
Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C, Jin L et al (2019) The trends in incidence of primary liver cancer caused by specific etiologies: results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol 70:674–683. https://doi.org/10.1016/j.jhep.2018.12.001
Lu XQ, Li Y, Wang W, Feng WT, Shi OM, Wang Q (2020) International incidence trends in early- and late-onset colorectal cancer: a population-based study. Int J Colorectal Dis 35:1077–1086. https://doi.org/10.1007/s00384-020-03558-2
Motsuku L, Chen WC, Muchengeti MM, Naidoo M, Quene TM, Kellett P, Mohlala MI et al (2021) Colorectal cancer incidence and mortality trends by sex and population group in South Africa: 2002–2014. BMC Cancer 21:129. https://doi.org/10.1186/s12885-021-07853-1
Schreuders EH, Ruco A, Rabeneck L, Schoen RE, Sung JJ, Young GP, Kuipers EJ (2015) Colorectal cancer screening: a global overview of existing programmes. Gut 64:1637–1649. https://doi.org/10.1136/gutjnl-2014-309086
Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, Cercek A et al (2020) Colorectal cancer statistics, 2020. CA Cancer J Clin 70:145–164. https://doi.org/10.3322/caac.21601
Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, Grove JT et al (2016) Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet 388:e19–e23. https://doi.org/10.1016/s0140-6736(16)30388-9
Wilsnack RW, Wilsnack SC, Kristjanson AF, Vogeltanz-Holm ND, Gmel G (2009) Gender and alcohol consumption: patterns from the multinational GENACIS project. Addiction 104:1487–1500. https://doi.org/10.1111/j.1360-0443.2009.02696.x
Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, Wan X et al (2013) Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet (london, England) 381:1987–2015. https://doi.org/10.1016/s0140-6736(13)61097-1
Yu H, Hemminki K (2020) Genetic epidemiology of colorectal cancer and associated cancers. Mutagenesis 35:207–219. https://doi.org/10.1093/mutage/gez022
Funding
This work was supported by the Key Laboratory of Diagnosis, Treatment and Research of Digestive System Tumor of Zhejiang Province (2019E10020), the Natural Public Welfare Fund of Zhejiang Province (LGC20H160002), the Medical and Health Science and Technology Foundation of Zhejiang Province (2019KY595, 2018KY690, 2018KY699, 2017KY593, 2017KY594), the Natural Science Foundation of Ningbo (2018A610368, 2017A610145, 2017A610158, 2016A610135), Key projects of Ningbo public welfare fund (20211JCGY020386), Ningbo Clinical Research Center for Digestive System Tumors (2019A21003), Natural Science Foundation of Ningbo (202003N4206), Ningbo Medical Key Discipline (No. 2022-B11), the Research Foundation of Hwa Mei Hospital, University of Chinese Academy of Sciences (2022HMKY3), the Public Welfare Foundation of Ningbo (2021S108).
Author information
Authors and Affiliations
Contributions
Jianjiong Li and Xiaoyu Dai conceived the ideas for this research and provided overall guidance; Ke Chen accessed and analyzed the data; Zhou Wu prepared the first draft and finished the manuscript based on revisions from all other authors. All authors had full access to all the data and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Ningbo No.2 Hospital and Informed consent of this study was waived because no identifiable information was included in the analyses. The data included in the GBD study were obtained primarily from censuses, household surveys, disease registries, health service utilization data, and vital statistics records.
The methods were conducted in accordance with regional, national and international guidelines and regulations and in accordance with the declaration of Helsinki. Ethical approval of the study was obtained from the Ethics Review Committee of Hwa Mei Hospital (YJ-KYSB-NBEY-2021–140-01). Informed consent was waived because no identifiable information was included in the analyses, and Hwa Mei Hospital waived the need of informed consent for this study.
Conflict of interest
The authors declare that they have no conflicts of interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to addition of a new foundation to the Funding section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, Z., Chen, K., Li, J. et al. The global, regional, and national burden of colorectal cancer in 204 countries and territories from 1990 to 2019. J Public Health (Berl.) 32, 609–618 (2024). https://doi.org/10.1007/s10389-023-01831-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-023-01831-6