Abstract
Aim
This research aims to examine the effects of variables that can affect COVID-19 deaths and cases in Organisation for Economic Co-operation and Development (OECD) countries during the years 2020 (first wave), 2021 (vaccine available), and 2022 (vaccine available and Omicron variant appeared).
Material and method
The factors that are thought to affect the case and death rates in 37 OECD countries were examined by multiple linear regression analysis using SPSS 22. The dependent variables were the COVID-19 deaths and cases per 10,000 (in 2020, 2021, and 2022); the independent variables were universal health coverage, physicians, nurses, intensive care beds, hospital beds, non-communicable diseases mortality per 100,000 people, population over 65 years of age, out-of-pocket expenditure, private expenditure, and health expenditure per capita and percent of % GDP.
Results
It was determined that the non-communicable diseases mortality is the relatively important variable COVID-19 cases and deaths in 2020 and 2021. After controlling for the scores of other variables, according to the ß coefficients, a one-unit increase in the number of physicians variable increases COVID-19 cases by 1.14 units in 2022; a one-unit increase in the universal coverage variable decreases COVID-19 deaths by 0.33 units in 2022.
Conclusion
The results of this research provide evidence that the effects of the COVID-19 outbreak have changed between 2020, the first wave of the epidemic, 2021, when the vaccine is available, and 2022, when both the vaccine is available and the Omicron variant is seen. With the increase in vaccination in 2022, the impact of non-communicable diseases mortality on the number of COVID-19 cases has decreased.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
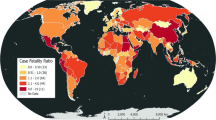
In late 2019, several cases reported in the Hubei (China) region presented to the hospital with complaints of pneumonia and respiratory failure caused by a novel coronavirus (SARS-CoV-2). On February 11, 2020, the World Health Organization defined this disease as COVID-19. COVID-19, named a public health emergency by the World Health Organization (WHO) on 30 January, was declared a pandemic by WHO on March 11, 2020 (Balkhair 2020; Ferrer 2020). COVID-19 is defined as a respiratory disease with a clinical spectrum of mild-to-moderate disease (80%), severe disease (15%) and critical illness (5%), with an overall case fatality rate of 0.5%–2.8% (European Centre for Disease Prevention and Control 2020).
The COVID-19 pandemic has caused great difficulties for health systems in addition to economic and political systems all worldwide (Balkhair 2020; Alshogran et al. 2021). The effects are still continuing, with more than 570 million confirmed cases and 6.3 million deaths worldwide at the end of July 2022 (Johns Hopkins CSSE 2022). With the disease becoming a global problem, interest in understanding the factors associated with deaths and cases from COVID-19 has increased. Understanding the socioeconomic, demographic, and health determinants that affect COVID-19 cases and deaths has become essential (Alshogran et al. 2021; García 2021).
It is thought that many factors had a critical place during the COVID-19 pandemic. Countries are expected to be more affected by COVID-19 with lower gross domestic product (GDP) or health resources such as fewer physicians and hospital beds (Li 2020). It has been demonstrated by international studies that socioeconomic inequalities have an important effect on death rates in the 1918 Spanish flu epidemic, the 2009 H1N1 epidemic, and the COVID-19 epidemic (Bambra et al. 2020). Additionally, there is evidence that the course of the epidemic differed significantly in countries where universality cannot be achieved in the provision of health services and where the distinction between rich and poor in access to services was felt (Oliver 2020; Unruh et al. 2021). Old age and comorbidities are considered the important risk factors for COVID-19 disease severity (Chen et al. 2020; Rod et al. 2020; Velevan and Meyer 2020). In addition to demographic variables, the pandemic is thought to be affected by many factors, including intensive care bed capacity. During the COVID-19 epidemic, acquiring beds turned into an opportunity for patient treatment (Xie et al. 2021). Intensive care specialists, in collaboration with many other clinical units within the hospital, have transformed other beds in hospitals up to 300% into intensive care services for the care of critical and severe patients (Ferrer 2020; Xie et al. 2021). Countries with higher beds per hospital are expected to experience less pressure and strain (Duhon et al. 2021).
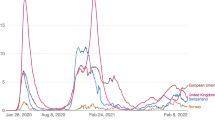
The effects of COVID-19, which emerged in late 2019, were seen in 2020 and reached its peak with increasing death numbers (Jabłońska et al. 2021). Because vaccines began receiving authorization in late 2020, most countries started to implement around 2020 and to spread in 2021 (OECD 2021; Prüβ 2021; Watson et al. 2022). The Omicron variant, on the other hand, was defined in late 2021 and its massive impact was felt in 2022 (Rana et al. 2022). The cumulative number of cases and deaths was insufficient to assess countries with high death and case rates in the early stages, but have been brought under control in the following years. Therefore, examining the effects of these variables during 2020 (first wave in the number of COVID-19 cases and deaths), 2021 (the vaccine is available), and 2022 (the vaccine is available and the Omicron variant) will provide interesting evaluations. Although there are studies in the literature that examine the factors affecting the number of COVID-19 cases or deaths (Bouba et al. 2021; Farseev et al. 2020; Upadhyaya et al. 2020), there have been no studies conducted to determine the factors that periodically affect the number of cases and deaths.
This research aims to determine variables and examine the effects of variables that can affect COVID-19 deaths and cases in Organisation for Economic Co-operation and Development (OECD) countries during the years 2020, 2021, and 2022. The OECD is an intergovernmental economic research institution committed to democratic government and market economy, headquartered in Paris, France, which provides the opportunity for comparison among countries by presenting statistically the health indicators of its member countries (Mattke et al. 2006; Kelley and Hurst 2006). It is thought that this will contribute to future healthcare planning by revealing the indicators related to the pandemic in OECD countries with this research.
Methods
The universe of the research consists of 38 OECD member countries. These countries were Australia, Austria, Belgium, Canada, Chile, Colombia, Costa Rica, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Israel, Italy, Japan, South Korea, Lithuania, Latvia, Luxembourg, Mexican, Holland, New Zealand, Norway, Poland, Portugal, Slovak Republic, Slovenia, Spain, Sweden, Switzerland, Turkey, United Kingdom, and the USA. In this study, the sample was not selected and the entire universe was reached. However, since the data on the number of intensive care beds in Costa Rica could not be reached, Costa Rica was excluded from the dataset. OECD countries were chosen because the OECD compile and compare data on member nations using the same standards (Afonso and Aubyn, 2005). Since it is of great importance that the data be complete and reliable in studies conducted with health indicators, care was taken in the selecting of the variables that the data were complete among OECD countries and belong to the same year. The independent variables' non-communicable disease data pertains to the year 2019, whilst the other variables do so for the year 2020.
The study's variables were chosen after researching the literature. The study's dependent variables are COVID-19 deaths per 10,000 people, and the COVID-19 cases per 10,000 people data pertains to the year 2020 (first wave in the number of COVID-19 cases and deaths), 2021 (the vaccine is available), and 2022 (the vaccine is available and the Omicron variant); the study's independent variables are current health expenditure (%) of GDP, out-of-pocket expenditure (%), private expenditure (%), government expenditure (%), health expenditures per capita, physicians per 1000 inhabitants, nurses per 1000 inhabitants, intensive care beds per 1000 people, universal health coverage (%), total non-communicable diseases mortality per 100,000 people, and population over 65 years of age (%) (Table 1). After obtaining the number of COVID-19 cases and deaths, the number of cases and deaths per 10,000 people was calculated using the population data of the countries.
Correlation analysis must be performed first in multiple regression because there are occasions when it is crucial to determine which independent variable is more significant and has a greater impact on the dependent variable (Gültekin 2013). Correlation analysis was used to choose the variables in order to avoid multiple correlation problems for independent variables. Correlation analysis is used to determine the linear relationship between two variables or to analyze the relationship of a variable with two or more variables. If the variables exhibit a normal distribution, they are analyzed with Pearson correlation analysis; if the variables don’t exhibit a normal distribution, they are analyzed with Spearman correlation analysis (Colak 2014). The determination of the normal distribution of the data included in the study was analyzed by looking at the values of the skewness and kurtosis coefficients, and based on this analysis, it was determined that the data showed a normal distribution and had parametric properties. Since the variables exhibited a normal distribution, Pearson correlation analysis was used.
In a theoretical model with continuous variables, a mathematical model is used to show the correlations between a dependent variable and multiple independent variables using the multiple linear regression technique (Özdamar 2011). Additionally, if the values of the explanatory variables are known, it is possible to estimate the value of the dependent variable, use the regression equation to explain the relationship between the predicted variable and the predictor variables, to reveal how much of the predictor variables explain the observed changes in the predicted variable, and to determine the degrees of the effects of a series of predictor variables that effect on the predicted variable. The multiple linear regression technique was used to determine the priorities in explaining the change (Büyüköztürk 2011; Can 2013; Karagöz 2016; Tabachnick and Fidell 1996). The enter technique is preferred because it allows for the simultaneous entry and analysis of all independent variables.
To use the multiple linear regression analysis technique, the independent variables should be accurately measured, the predicted and predictive variables should have a normal distribution, and there shouldn't be any multicollinearity between them (Field 2009; Özdamar 2011; Tabachnick and Fidell 1996). In the study, the Mahalanobis distance was analyzed, and it was found that several countries had extreme values that deviated from the sample. The analyses, however, led to the finding that there are no countries with extremely extreme values. Scatter diagrams were used to examine the multivariate normality assumption, and it was discovered that the resulting diagrams were elliptical, indicating that the data had a multivariate normal distribution. Regression analysis residual plots were used to examine the linearity of the data within the variables of the study. The difference between the actual values of the data included in the study and the estimated value after the model determination is defined as the residual value; it represents the error part in the regression model and in cases where the model does not fit well, the residual values are large, and the large-residual values indicate that the data have extreme values (Şen, 2016). It was found that there was no negative in the model fit and that the linearity assumption was observed because the student type residuals obtained within the scope of this study are in the range of +2 to −2. It was determined that there was no multicollinearity problem in the study's data since VIF values are VIF < 10, tolerance value is > 0.1, Cl values are Cl < 10. The program SPSS 22.0 was used to process the data.
Results
It is determined that there is a significant and very high correlation between current health expenditure (%) of GDP and government expenditure (%), health expenditures per capita, also between nurses per 1000 people and health expenditures per capita (r > 0.80, p = 0.00). The conclusion is that there is a significant and high correlation between intensive care beds per 1000 people and hospital beds per 1000 people (r = 0.60–0.80, p = 0.00). Results of the analysis: health expenditures per capita which is very highly correlated with government expenditure (%), current health expenditure (%) of GDP which is highly correlated with health expenditures per capita, and intensive care beds per 1000 people which is highly correlated with hospital beds per 1000 people are excluded from the variables (Table 2).
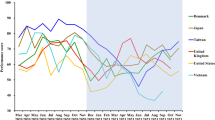
It is determined that the average rate of COVID-19 cases in OECD countries is 314,19 in 2020; the average rate of COVID-19 cases is 892 in 2021, and the average rate of COVID-19 cases is 2933,06 in 2022. It was determined that the average deaths of COVID-19 is 12,07 in 2020; the average deaths of COVID-19 is 9,81 in 2021, and the average deaths of COVID-19 is 6,62 in 2022. The average rate of universal health coverage (%) is 12,07; the average rate of physicians (per 1000 people) are 3,64; the average rate of nurses (per 1000 people) are 9,31; the average rate of intensive care beds are 3.84; the average rate of non-communicable diseases mortality are 349.3; the average rate of the population over 65 is 18.0; the average rate of out-of-pocket expenditures are 1.7 and the average rate of private expenditures are 0,55 (Table 3).
Thought to impact on the COVID-19 cases per 10,000 people in 2020 (first wave in COVID-19 cases), 2021 (the vaccine is available), and 2022 (the vaccine is available and the Omicron variant) were the model-established variables of universal health coverage (%), physicians (per 1000 people), nurses (per 1000 people), intensive care beds (per 1000 people), non-communicable diseases mortality (per 100.000), population over 65 years of age (%), out-of-pocket expenditure (%), private expenditure (%).
Thus, it can be stated that there is a significant relationship between the predicted variable and the predictor variables. The variables used explained 25% the COVID-19 cases per 10,000 people in 2020 when in the first wave. When the standardized regression coefficients are examined, the predictor variable that is significant is non-communicable disease, which is a relatively significant variable in the COVID-19 cases in 2020 (ß = 2.23).
The variables used explained 30% of the number of COVID-19 cases per 10,000 people in 2021 when the vaccine was available. When the standardized regression coefficients are assessed, the non-communicable disease predictor variable is also considerable and is a relatively significant variable in the number of COVID-19 cases in 2021 (ß = 1.78).
The variables used explained 50% of the number of COVID-19 cases per 10,000 people in 2022 when the vaccine was available and the Omicron variant was active. When the standardized regression coefficients are examined, the physicians, which is a relatively significant variable because the vaccine is available, (ß = 1.14) are significant predictor variable in the number of COVID-19 cases in 2022 (Table 4).
It was determined that non-communicable diseases mortality is the relatively important variable in the first wave in the number of COVID-19 cases in 2020, and the vaccine being available in the number of COVID-19 cases in 2021. Therefore, a new model was established to determine the impact of non-communicable diseases mortality (per 100,000) during 2020 (first wave in number of COVID-19 cases) and 2021 (the vaccine is available).
It was determined that the non-communicable disease variables explained 11% of COVID-19 cases in 2020 (first wave) and, 13% of Covid 19 cases in 2021 (presence of vaccine). It was determined that physicians are the relatively important variable in the number of COVID-19 cases in 2022. A new model was established to determine the impact of physicians on the number of COVID-19 cases in 2022 (the vaccine is available and the Omicron variant). Physicians explained 30% of the number of COVID-19 cases per 10,000 people in 2022 when the vaccine is available and the Omicron variant is spreading (Table 5).
Those variables considered to impact on the deaths of COVID-19 per 10,000 during 2020 (first wave in the number of COVID-19 death), 2021 (the vaccine is available), and 2022 (the vaccine is available and the Omicron variant is present), were determined to be the models-established variables of universal health coverage (%), physicians (per 1000 people), nurses (per 1000 people), intensive care beds (per 1000 people), non-communicable diseases mortality (per 100,000), population over 65 years of age (%), out-of-pocket expenditure (%), and private expenditure (%). As a result, a significant relationship exists between the predicted variable and the predictor variables.
The variables used explained 20% of the number of COVID-19 deaths per 10,000 people in 2020 during the first wave. Non-communicable disease, which is a moderately significant variable on COVID-19 death in 2020 during the first wave, is the predictor variable that is significant when the standardized regression coefficients are assessed (ß = 2.48) (Table 6).
The variables used explained 45% of the COVID-19 deaths per 10,000 people in 2021 (the year the vaccine was available). The non-communicable diseases mortality predictor variable is a relatively significant variable in the number of COVID-19 deaths in 2021 (ß = 3.22), according to the analysis of the standardized regression coefficients (Table 6).
The variables used explained 39% of the COVID-19 deaths per 10,000 people in 2022 (the vaccine was available and the Omicron variant was active). The COVID-19 death rate in 2022 is also influenced by the non-communicable diseases mortality (Table 6).
It is determined that non-communicable diseases mortality is the relatively significant factor in the number of COVID-19 deaths in 2020 during the first wave. To assess the effect of non-communicable disease mortality in 2020, a new model was developed. It is determined that the non-communicable diseases variables explained 11% of COVID-19 deaths in 2020.
Non-communicable diseases mortality and nurses were found to be two moderately significant variables for 2021 when the vaccine was available. According to analysis, nurses and non-communicable diseases mortality account for 30% of COVID-19 deaths in 2021 when the vaccine was available.
It was determined that the number of COVID-19 deaths in 2022 would be influenced by noncommunicable diseases and universal health coverage. Thus, a new model was established to determine the impact of non-communicable diseases mortality and universal health coverage during 2022 when the vaccine was available and the Omicron variant was present. Non-communicable diseases mortality and universal health coverage variables explained 28% of the number of COVID-19 deaths per 10,000 people in 2022 (Table 7).
Discussion
In this study on the COVID-19 deaths and cases in OECD countries during 2020, 2021, and 2022, the effects of countries' healthcare resources, healthcare financing, non-communicable diseases mortality, and population over 65 years of age are emphasized.
According to the research findings, in 2020, during the first wave of COVID-19, and in 2021, when the vaccine was available, non-communicable diseases mortality were found to be the most significant variable on the number of COVID-19 cases and deaths in OECD countries. After controlling for the scores of other variables according to the ß coefficients, a one-unit increase in the non-communicable diseases mortality variable increased COVID-19 cases by 2.23 units in 2020 and by 1.78 units in 2021. Additionally, a one-unit increase in the non-communicable diseases mortality variable increased COVID-19 deaths by 2.48 units in 2020 and by 3.22 units in 2021.
This result can be explained by the fact that COVID-19 affects people with chronic diseases more. The non-communicable disease mortality examined in this study represents the share of deaths in total deaths for all ages due to causes including cancer, diabetes, cardiovascular diseases, digestive diseases, dermatologic diseases, musculoskeletal diseases, and congenital abnormalities (World Bank 2021). Bretschger et al. (2020), in their study on 37 OECD countries, found that the prevalence of obesity has significant effects on the number of COVID-19 deaths. Koç and Saraç (2020) found that the increase in the prevalence of chronic diseases such as obesity and diabetes has an increasing effect on the number of COVID-19 cases and deaths in a study on 36 OECD countries. Hashim et al. (2020), in their study of 93 countries, found that certain risk factors were predictors of the case fatality rate per 100,000 population (R2 = 0.35, p < 0.05). These risk factors included Alzheimer's disease, COPD, depression, and GDP per capita. In a study by Alshogran et al. (2021) in 113 countries, and in another study by Khan et al. (2020) in 86 countries, a statistically significant positive correlation was found between non-communicable disease mortality and COVID-19 case fatality rate. The results of various studies are also similar to the findings obtained from this study.
Some studies in the literature have found that people with non-communicable diseases mortality such as diabetes, cardiovascular disease, chronic kidney disease, chronic respiratory disease, hypertension, and cancer have a higher risk of COVID-19 death than those who do not (Acharya et al. 2020; Caramelo et al. 2020; Erdal et al. 2021; Goh et al. 2020; Macedo et al. 2020). There is evidence to suggest that, in addition to the risk of death, chronic diseases also affect hospitalization and the increasing number of cases (Li et al. 2020; Semenzato et al. 2021). It is thought that measures should be taken for the treatment of chronic patients during the COVID-19 pandemic (Öztürk and Çınar 2021).
It was concluded that both the vaccine and the development of the Omicron variant reduced the impact of non-communicable diseases mortality on COVID-19. This situation can be explained by the widespread use of one dose of vaccination in 2022, and even the fact that two and third doses of vaccination have been made (Chen et al. 2022).
After controlling for the scores of other variables according to the ß coefficients, a one-unit increase in the number of physicians variable increased COVID-19 cases by 1.14 units in 2022. The number of doctors was the most important variable in 2022 when the spread both of vaccination and the Omicron variant was seen. In line with the findings from this study, there is evidence of a positive relationship between COVID-19 deaths and the number of physicians. Wirawan and Januraga (2021) found a positive significant relationship between the incidence of COVID-19 and the ratio of general practitioners. Gayawan et al. (2020) found a significant positive correlation (r= 0.49) between COVID-19 and the number of physicians in their study in 47 African countries. De Figueiredo et al. (2021), on the other hand, found that the number of physicians per capita was associated with a higher incidence rate.
In many studies, a negative relationship between variables such as COVID-19 deaths and case fatality rate with the number of physicians is seen (Alshogran et al. 2021; Blondel and Vranceanu 2020; Lupu et al. 2020; Khan et al. 2020; García 2021). Barnett-Itzhaki and Levi (2021), in their study on 36 OECD countries, found that the number of physicians did not have a significant effect on confirmed cases 60 and 80 days after the first confirmed case. In a study conducted by Bouba et al. (2021) in 54 African countries, it was found that the number of physicians per 1000 people did not significantly affect COVID-19 cases.
In line with the results obtained from different studies in the literature, we can say that there is no agreement on the relationship between the number of physicians and COVID-19 cases and deaths. Overall, an increase in the number of physicians in a country is expected to have a negative impact on the deaths and cases as it means better healthcare for patients who are infected and prone to COVID-19 infection and death (Upadhyaya et al. 2020). This positive relationship between the COVID-19 deaths and the number of physicians in some studies is described as a paradox and can be explained using healthcare capacity as a measure of a country's wealth (De Figueiredo et al. 2021). It is thought that this situation that emerged in the studies may be due to the different characteristics of the sample group and the use of data sets from different years.
After controlling for the scores of other variables according to the ß coefficients, a one-unit increase in the universal coverage variable decreased COVID-19 deaths by 0.33 units in 2022. Increasing universal health coverage, which means access to health services, including preventive, curative, rehabilitation, and health promotion, is associated with the intention to improve the accessibility and affordability of health services (Hussain and Arif 2021). For example, Finland implemented some reforms to expand health coverage during the pandemic (Hiam and Yates 2021).
Conclusion
The COVID-19 outbreak has revealed that the vulnerabilities in the health systems of countries have profound effects on people's health, economy, trust in the government, and social life around the world. To effectively combat COVID-19, it is vital to identify the factors that affect the results of COVID-19. It is estimated that the number of confirmed cases and deaths worldwide is underreported. All the same, it is difficult to make comparisons between countries due to differences in their health systems. Inevitably, the measures taken by countries in fighting the COVID-19 pandemic will also affect the research findings. Therefore, the COVID-19 data need to be interpreted carefully.
The results of this research provide evidence that the effects of the COVID-19 outbreak have changed between 2020, during the first wave of the epidemic, 2021, when the vaccine was available, and 2022, when both the vaccine was available and the Omicron variant was seen. With the increase in vaccination in 2022, the impact of non-communicable diseases on the number of COVID-19 cases has decreased. However, non-communicable diseases mortality has been a significant determinant in the number of COVID-19 cases and deaths in OECD countries in 2020 and 2021. The results show that tackling chronic diseases can help significantly reduce the negative effects of the COVID-19 pandemic. The disease burden and universal health coverage are considered as key factors in controlling losses from the pandemic. It is recommended to publish the number of physicians according to the branches in make better estimates.
Additionally, the negative effect of universal health coverage on the number of COVID-19 deaths in 2022 draws attention to the conclusion that increasing insurance coverage will reduce the effects of the pandemic. Additionally, one of the greatest weapons of fighting against COVID-19 is the correct management of the crisis with timely and appropriate restrictions taken by countries. Countries should adopt the best strategy appropriate to them, depending on the resources they have and the availability of chronic disease burden.
Research limitations
The most important problem in studies on COVID-19 is that there are no data for the same period in each country for the variables used. In this study, COVID-19 cases and deaths, which are the dependent variable, belong to 2020, 2021, and 2022; the independent variables belong to the most recent year available, 2020.
Data from the OECD, World Bank, Trading Economics, and the Worldometer were used as data sources in the research. The most up-to-date data were included in the study because there were no variables for the years compared for each variable examined within the scope of the research in the data sources. While evaluating the number of physicians per 1000 people, which is a variable used in the research, not every physician treats patients with COVID-19.
During the pandemic period, cash aid and especially social security expenditures were made to hospitals in countries. For example, in the USA, the government has provided $100 billion in cash aid to hospitals affected by COVID-19 (Congressional Budget Office 2021; Cutler 2020). Therefore, the countries' health expenditures during the pandemic may have increased due to their emergency budgets. Additionally, the fact that each country has started to take different measures at different times may effect the number of COVID-19 cases and deaths.
References
Acharya D, Lee K, Lee DS, Lee YS, Moon SS (2020) Mortality rate and predictors of mortality in hospitalized COVID-19 patients with diabetes. Healthcare 8:338. https://doi.org/10.3390/healthcare8030338
Afonso A, Aubyn M (2005) Non-parametric approaches to education and health efficiency in OECD countries. J Appl Econ 8(2):227–246. https://doi.org/10.1080/15140326.2005.12040626
Alshogran OY, Altawalbeh SM, Al-Azzam SI, Karasneh R (2021) Predictors of Covid-19 case fatality rate: An ecological study. Ann Med Surg 65:102319. https://doi.org/10.1016/j.amsu.2021.102319
Balkhair AA (2020) COVID-19 pandemic: a new chapter in the history of infectious diseases. Oman Med J 35(2):e123. https://doi.org/10.5001/omj.2020.41
Bambra C, Riordan R, Ford J, Matthews F (2020) The COVID-19 pandemic and health inequalities. J Epidemiol Commun Health 74(11):964–968. https://doi.org/10.1136/jech-2020-214401
Barnett-Itzhaki Z, Levi A (2021) Effects of chronic exposure to ambient air pollutants on COVID-19 morbidity and mortality—a lesson from OECD countries. Environ Res 195:110723. https://doi.org/10.1016/j.envres.2021.110723
Blondel S, Vranceanu R (2020) COVID-19 mortality and health expenditures across European countries: the positive correlation puzzle. SSRN Journal 2020:3679972. https://doi.org/10.2139/ssrn.3679972
Bouba Y, Tsinda EK, Fonkou MDM, Mmbando GS, Bragazzi NL, Kong JD (2021) The determinants of the low COVID-19 transmission and mortality rates in Africa: a cross-country analysis. Front Public Health 9:751197. https://doi.org/10.3389/fpubh.2021.751197
Bretschger L, Grieg E, Welfens PJ, Xiong T (2020) COVID-19 infections and fatalities developments: empirical evidence for OECD countries and newly industrialized economies. IEEP 17(4):801–847. https://doi.org/10.1007/s10368-020-00487-x
Büyüköztürk S (2011) Sosyal bilimler için veri analizi el kitabı. Pegem Akademi Yayıncılık, Ankara
Can A (2013) SPSS ile bilimsel araştırma sürecinde nicel veri analizi. Pegem Akademi Yayıncılık, Ankara
Caramelo F, Ferreira N, Oliveiros B (2020) Estimation of risk factors for COVID-19 mortality—preliminary results. MedRxiv. https://doi.org/10.1101/2020.02.24.20027268
Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K, Xu D, Yu H, Wang H (2020) Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 368:m1091. https://doi.org/10.1136/bmj.m1091
Chen Z, Zheng W, Wu Q et al (2022) Global diversity of policy, coverage, and demand of COVID-19 vaccines: a descriptive study. BMC Med 20:130. https://doi.org/10.1186/s12916-022-02333-0
Colak E (2014) Korelasyon analizi. http://eczacilik.anadolu.edu.tr/bolumSayfalari/belgeler/ecz2014%2012_20140527094539.pdf Accessed 19 July 2022
Congressional Budget Office (2021) The federal budget in fiscal year 2020: An infographic. Congressional Budget Office, Washington DC. https://www.cbo.gov/publication/57170 20 Dec 2022.
Cutler D (2020) How will COVID-19 affect the health care economy? JAMA 323(22):2237–2238. https://doi.org/10.1001/jama.2020.7308
De Figueiredo AM, Daponte A, De Figueiredo DCMM, Gil-García E, Kalache A (2021) Letalidad de la COVID-19: ausencia de patrón epidemiológico. Gac Sanit 35(4):355–357. https://doi.org/10.1016/j.gaceta.2020.04.001
Duhon J, Bragazzi N, Kong JD (2021) The impact of non-pharmaceutical interventions, demographic, social, and climatic factors on the initial growth rate of COVID-19: A cross-country study. Sci Total Environ 760:144325. https://doi.org/10.1016/j.scitotenv.2020.144325
Erdal GS, Polat O, Erdem GU, Korkusuz R, Hindilerden F, Yilmaz M et al (2021) The mortality rate of COVID-19 was high in cancer patients: a retrospective single-center study. Int J Clin Oncol 26(5):826–834. https://doi.org/10.1007/s10147-021-01863-6
European Centre for Disease Prevention and Control (2020) Coronavirus disease 2019 (COVID-19) pandemic: increased transmission in the EU/EEA and the UK –seventh update, Stockholm. https://www.ecdc.europa.eu/sites/default/files/documents/RRA-COVID19-update10-2020-06-11.pdf. Accessed 15 Dec 2022
Farseev A, Chu-Farseeva YY, Qi Y, Loo DB (2020) Understanding economic and health factors impacting the spread of COVID-19 disease. medRxiv. https://doi.org/10.1101/2020.04.10.20058222
Ferrer R (2020) COVID-19 pandemic: the greatest challenge in the history of critical care. Med Int 44(6):323–324. https://doi.org/10.1016/j.medine.2020.04.005
Field A (2009) Discovering statistics using SPSS (and sex and drugs and rock ‘n’ roll), Third edition, SAGE Publications, London
García CN (2021) Socioeconomic, demographic and healthcare determinants of the COVID-19 pandemic: an ecological study of Spain. BMC Public Health 21:1–8. https://doi.org/10.1186/s12889-021-10658-3
Gayawan E, Awe OO, OseniBM UIC, Adekunle A, Samuel G, Eisen DP, Adegboye OA (2020) The spatio-temporal epidemic dynamics of COVID-19 outbreak in Africa. Epidemiol Infect 148:e212. https://doi.org/10.1017/S0950268820001983
Goh HP, Mahari WI, Ahad NI, Chaw L, Kifli N, Goh BH et al (2020) Risk factors affecting COVID-19 case fatality rate: A quantitative analysis of top 50 affected countries. medRxiv. https://doi.org/10.1101/2020.05.20.20108449
Gültekin F (2013) Regresyon analizi. http://w3.balikesir.edu.tr/~bsentuna/wp-content/uploads/2013/03/Regresyon-Analizi.pdf Accessed 19 July 2022
Hashim MJ, Alsuwaidi AR, Khan G (2020) Population risk factors for COVID-19 mortality in 93 countries. J Epidemiol Global Health 10(3):204. https://doi.org/10.2991/jegh.k.200721.001
Hiam L, Yates R (2021) Will the COVID-19 crisis catalyse universal health reforms? Lancet 398(10301):646–648. https://doi.org/10.1016/S0140-6736(21)01650-0
Hussain R, Arif S (2021) Universal health coverage and COVID-19: recent developments and implications. J Pharm Policy Pract 14:23. https://doi.org/10.1186/s40545-021-00306-x
Jabłońska K, Aballéa S, Toumi M (2021) Factors influencing the COVID-19 daily deaths' peak across European countries. Public Health 194:135–142. https://doi.org/10.1016/j.puhe.2021.02.037
Johns Hopkins CSSE (2022) COVID-19 Map. Johns Hopkins Coronavirus Resouce Center, Baltimore MD. https://coronavirus.jhu.edu/map.html Accessed 27 June 2022
Karagöz Y (2016) SPSS ve AMOS23 uygulamalı istatistiksel analizler. Nobel Akademik Yayıncılık, Ankara
Kelley E, Hurst J (2006) Health care quality indicators project: conceptual framework paper. OECD Health Working Papers, No. 23. OECD Publishing, Paris. https://doi.org/10.1787/440134737301
Khan JR, Awan N, Islam M, Muurlink O (2020) Healthcare capacity, health expenditure, and civil society as predictors of COVID-19 case fatalities: a global analysis. Front Public Health 8:347. https://doi.org/10.3389/fpubh.2020.00347
Koç İ, Saraç M (2020) Socio-economic, demographic and health determinants of the coronavirus pandemic: Analysis of data from OECD countries. Turkish. J Public Health 18(COVID-19 Special):1–13. https://doi.org/10.20518/tjph.721921
Li WX (2020) Worldwide inverse correlation between Bacille Calmette–Guérin immunization and COVID-19 morbidity and mortality. Infection 49(3):463–473. https://doi.org/10.1007/s15010-020-01566-6
Li AY, Hannah TC, Durbin J, Dreher N, McAuley FM, Marayati NF, Choudhri TF (2020) Multivariate analysis of factors affecting COVID-19 case and death rate in US counties: the significant effects of black race and temperature. medRxiv. https://doi.org/10.1101/2020.04.17.20069708
Lupu D, Maha LG, Viorică ED (2020) COVID-19 incidence in Europe: drivers and government interventions. Transylvanian Rev Administrative Sci 16(SI):80–93. https://doi.org/10.24193/tras.SI2020.5
Macedo MC, Pinheiro IM, Carvalho CJ, Fraga HC, Araujo IP, Montes SS, Souza AC (2020) Correlation between hospitalized patients’ demographics, symptoms, comorbidities, and COVID-19 pandemic in Bahia, Brazil. PloS One 15(12):e0243966. https://doi.org/10.1371/journal.pone.0243966
Mattke S, Epstein AM, Leatherman S (2006) The OECD health care quality indicators project: history and background. Int J Qual Health Care 18:1–4. https://doi.org/10.1093/intqhc/mzl019
OECD (2021) Access to COVID-19 vaccines: global approaches in a global crisis. OECD Publishing, Paris. https://read.oecd-ilibrary.org/view/?ref=1069_1069384-ewmqrw9sx2&title=Access-to-COVID-19-vaccines-Global-approaches-in-a-global-crisis. Accessed 15 Dec 2022
Oliver L (2020) Coronavirus: a pandemic in the age of inequality. Paper presented at the World Economic Forum. https://www.weforum.org/agenda/2020/03/coronavirus-pandemic-inequality-among-workers/ 14 Dec 2022.
Özdamar K (2011) Paket programlar ile statistiksel veri nalizi. 5. Baskı. Kaan Kitabevi, Eskişehir
Öztürk A, Çınar D (2021) Cancer care management during Covid-19 pandemic. BANU J Health Sci Res 3(1):45–51. https://doi.org/10.46413/boneyusbad.864878
Prüβ BM (2021) Current state of the first COVID-19 vaccines. Vaccines 9(1):30. https://doi.org/10.3390/vaccines9010030
Rana R, Kant R, Huirem RS, Bohra D, Ganguly NK (2022) Omicron variant: Current insights and future directions. Microbiol Res 265:127204. https://doi.org/10.1016/j.micres.2022.127204
Rod J, Oviedo-Trespalacios O, Cortes-Ramirez J (2020) A brief review of the risk factors for COVID-19 severity. Rev Saude Publica 54:60. https://doi.org/10.11606/s1518-8787.2020054002481
Semenzato L, Botton J, Drouin J, Cuenot F, Dray-Spira R, Weill A, Zureik M (2021) Chronic diseases, health conditions and risk of COVID-19-related hospitalization and in-hospital mortality during the first wave of the epidemic in France: a cohort study of 66 million people. Lancet Region Health-Europe 8:100158. https://doi.org/10.1016/j.lanepe.2021.100158
Şen S (2016). Regresyon analizi. https://sedatsen.files.wordpress.com/2016/11/8-sunum.pdf Accessed: 15 July 2022
Tabachnick BG, Fidell LS (1996) Using multivariate statistics. Third edition. Harper Collins College Publishers, New York
Unruh L, Allin S, Marchildon G, Burke S, Barry S, Siersbaek R, Thomas S, Rajan S, Koval A, Alexander M, Merkur S, Webb E, Williams GA (2021) A comparison of health policy responses to the COVID-19 pandemic in Canada, Ireland, the United Kingdom and the United States of America. Health Policy 126:427–437. https://doi.org/10.1016/j.healthpol.2021.06.012
Upadhyaya A, Koirala S, Ressler R, Upadhyaya K (2020) Factors affecting COVID-19 mortality: an exploratory study. J Health Res 36(1):166–175. https://doi.org/10.1108/JHR-09-2020-0448
Velevan TP, Meyer CG (2020) The COVID-19 epidemic. Trop Med Int Health 25(3):278–280. https://doi.org/10.1111/tmi.13383
Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC (2022) Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis 22(9):1293–1302. https://doi.org/10.1016/S1473-3099(22)00320-6
Wirawan GBS, Januraga PP (2021) Correlation of demographics, healthcare availability, and COVID-19 outcome: Indonesian ecological study. Front Public Health 9:605290. https://doi.org/10.3389/fpubh.2021.605290
World Bank (2021) Cause of death, by non-communicable diseases (% of total). World Bank, Washington DC. https://data.worldbank.org/indicator/SH.DTH.NCOM.ZS
Xie L, Yang H, Zheng X, Wu Y, Lin X, Shen Z (2021) Medical resources and coronavirus disease (COVID-19) mortality rate: evidence and implications from Hubei province in China. PLoS One 16(1):e0244867. https://doi.org/10.1371/journal.pone.0244867
Author information
Authors and Affiliations
Contributions
BT was responsible for the study design and writing the paper. MMG was responsible for methodology and statistical analysis. GO and MT were responsible for the literature and results, and for providing comments on the writing. All authors were responsible for supervising the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tekerek, B., Günaltay, M.M., Ozler, G. et al. Determinants of COVID-19 cases and deaths in OECD countries. J Public Health (Berl.) 32, 473–484 (2024). https://doi.org/10.1007/s10389-023-01820-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-023-01820-9