Abstract
Background
Development of gastroesophageal reflux disease (GERD) after gastrostomy remains debatable. Therefore, this study aimed to evaluate whether laparoscopy-aided gastrostomy (LAG) influence on the occurrence of GERD in neurologically impaired (NI) patients. Furthermore, we investigated whether preoperatively excluding NI patients with GERD can reduce the number of patients requiring subsequent anti-reflux surgery (ARS) after LAG.
Methods
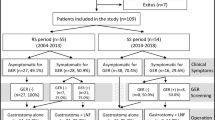
This retrospective study included 35 NI patients (median age: 11.0; interquartile range 5.0–23.5 years) who underwent LAG according to our criterion from October 2012 to June 2020 and MII-pH before and after LAG. MII-pH parameters were compared in all patients and among three age groups between before and after LAG.
Results
There were no significant differences in MII-pH parameters before and 1 year after LAG in all patients, and no patient underwent subsequent ARS. Only one paediatric patient with 64 number of reflux episodes before LAG required subsequent ARS 3 years after LAG.
Conclusions
Generally, LAG did not influence the postoperative GERD at 1 year after LAG, and our criteria could reduce the number of patients requiring subsequent ARS. However, paediatric NI patients with higher number of reflux episodes in preoperative MII-pH study may need careful long-term follow-up after LAG.


Similar content being viewed by others
References
Kawahara H, Kubota A, Okuyama H, et al. One-trocar laparoscopy-aided gastrostomy in handicapped children. J Pediatr Surg. 2006;41:2076–80.
Suksamanapun N, Mauritz FA, Franken J, et al. Laparoscopic versus percutaneous endoscopic gastrostomy placement in children: results of a systematic review and meta-analysis. J Minim Access Surg. 2017;13:81–8.
Khattak IU, Kimber C, Kiely EM, et al. Percutaneous endoscopic gastrostomy in paediatric practice: complications and outcome. J Pediatr Surg. 1998;33:67–72.
Sulaeman E, Udall JN, Brown RF, et al. Gastroesophageal reflux and Nissen fundoplication following percutaneous endoscopic gastrostomy in children. J Pediatr Gastroenterol Nutr. 1998;26:269–73.
Kawahara H, Tazuke Y, Soh H, et al. Does laparoscopy-aided gastrostomy placement improve or worsen gastroesophageal reflux in patients with neurological impairment? J Pediatr Surg. 2014;49:1742–5.
Franken J, Stellato RK, Tytgat SHAJ, et al. Gastro-esophageal reflux after laparoscopic gastrostomy placement in children. J Pediatr Gastroenterol Nutr. 2020;70:e41–7.
Toporowska Kowalska E, Gębora Kowalska B, Jabłoński J, et al. Influence of percutaneous endoscopic gastrostomy on gastro-oesophageal reflux evaluated by multiple intraluminal impedance in children with neurological impairment. Dev Med Child Neurol. 2011;53:938–43.
Thomson M, Rao P, Rawat D, et al. Percutaneous endoscopic gastrostomy and gastro-oesophageal reflux in neurologically impaired children. World J Gastroenterol. 2011;17:191–6.
Berman L, Sharif I, Rothstein D, et al. Concomitant fundoplication increases morbidity of gastrostomy tube placement. J Pediatr Surg. 2015;50:1104–8.
Kawahara H, Mitani Y, Nose K, et al. Should fundoplication be added at the time of gastrostomy placement in patients who are neurologically impaired? J Pediatr Surg. 2010;45:2373–6.
Plantin I, Arnbjörnsson E, Larsson L-T. No increase in gastroesophageal reflux after laparoscopic gastrostomy in children. Pediatr Surg Int. 2006;22:581–4.
Heine RG, Reddihough DS, Catto Smith AG. Gastro-oesophageal reflux and feeding problems after gastrostomy in children with severe neurological impairment. Dev Med Child Neurol. 1995;37:320–9.
Wenzl TG, Benninga MA, Loots CM, et al. Indications, methodology, and interpretation of combined esophageal impedance-pH monitoring in children: ESPGHAN EURO-PIG. J Pediatr Gastroenterol Nutr. 2012;55(2):230–4.
Quitadamo P, Tambucci R, Mancini V, et al. Esophageal pH-impedance monitoring in children: position paper on indications, methodology and interpretation by the SIGENP working group. Dig Liver Dis. 2019;51:1522–36.
Fukahori S, Kawahara H, Oyama T, et al. Standard protocol devised by the Japanese Pediatric Impedance Working Group for combined multichannel intraluminal impedance-pH measurements in children. Surg Today. 2020;50:664–71.
Fukahori S, Yagi M, Ishii S, et al. Analyses of the relationship between a “number of reflux episodes” exceeding 70 and the pH index in neurologically impaired children by evaluating esophageal combined pH-multichannel intraluminal impedance measurements. Scand J Gastroenterol. 2018;53:519–26.
Samuel M, Holmes K. Quantitative and qualitative analysis of gastroesophageal reflux after percutaneous endoscopic gastrostomy. J Pediatr Surg. 2002;37:256–61.
Wilson GJP, van der Zee DC, Bax NMA. Endoscopic gastrostomy placement in the child with gastroesophageal reflux: is concomitant antireflux surgery indicated? J Pediatr Surg. 2006;41:1441–5.
Aumar M, Lalanne A, Guimber D, et al. Influence of percutaneous endoscopic gastrostomy on gastroesophageal reflux disease in children. J Pediatr. 2018;197:116–20.
Mousa HM, Rosen R, Woodley FW, et al. Esophageal impedance monitoring for gastroesophageal reflux. J Pediatr Gastroenterol Nutr. 2011;52:129–39.
Cresi F, Cester EA, Salvatore S, et al. Multichannel intraluminal impedance and ph monitoring: a step towards pediatric reference values. J Neurogastroenterol Motil. 2020;26:370–7.
Rosen R, Nurko S. The importance of multichannel intraluminal impedance in the evaluation of children with persistent respiratory symptoms. Am J Gastroenterol. 2004;99:2452–8.
Pandolfino JE, Vela MF. Esophageal-reflux monitoring. Gastrointest Endosc. 2009;69:917–30.
Pilic D, Fröhlich T, Nöh F, et al. Detection of gastroesophageal reflux in children using combined multichannel intraluminal impedance and pH measurement: data from the German Pediatric Impedance Group. J Pediatr. 2011;158:650–4.
Yap BKY, Nah SA, Chen Y, et al. Fundoplication with gastrostomy vs gastrostomy alone: a systematic review and meta-analysis of outcomes and complications. Pediatr Surg Int. 2017;33:217–28.
Acknowledgements
The authors thank ENAGO for editing this manuscript.
Funding
No funding declared.
Author information
Authors and Affiliations
Contributions
DM and SF designed the research study, analyzed the data, and wrote the paper; YT designed the research study and wrote the paper; SI and NH analyzed the data; NS, NH, YK, SS, ST, and HN performed the research.
Corresponding author
Ethics declarations
Ethical statement
The protocol of this study has been approved by the Kurume University Ethical Committee (No. 20133). Informed consent was obtained from the families before starting this study.
Conflict of interest
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Masui, D., Fukahori, S., Hashizume, N. et al. Influence of laparoscopy-aided gastrostomy on gastroesophageal reflux in neurologically impaired patients using multichannel intraluminal impedance pH measurements. Esophagus 19, 360–366 (2022). https://doi.org/10.1007/s10388-021-00888-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-021-00888-0