Abstract
Background
The presence of lymph node metastasis (LNmets) is a poor prognostic factor in oesophageal cancer (OeC) patients treated with neoadjuvant chemoradiotherapy (nCRT) followed by surgery. Tumour regression grade (TRG) in LNmets has been suggested as a predictor for survival. The aim of this study was to investigate whether TRG in LNmets is related to their location within the radiotherapy (RT) field.
Methods
Histopathological TRG was retrospectively classified in 2565 lymph nodes (LNs) from 117 OeC patients treated with nCRT and surgery as: (A) no tumour, no signs of regression; (B) tumour without regression; (C) viable tumour and regression; and (D) complete response. Multivariate survival analysis was used to investigate the relationship between LN location within the RT field, pathological TRG of the LN and TRG of the primary tumour.
Results
In 63 (54%) patients, viable tumour cells or signs of regression were seen in 264 (10.2%) LNs which were classified as TRG-B (n = 56), C (n = 104) or D (n = 104) LNs. 73% of B, C and D LNs were located within the RT field. There was a trend towards a relationship between LN response and anatomical LN location with respect to the RT field (p = 0.052). Multivariate analysis showed that only the presence of LNmets within the RT field with TRG-B is related to poor overall survival.
Conclusion
Patients have the best survival if all LNmets show tumour regression, even if LNmets are located outside the RT field. Response in LNmets to nCRT is heterogeneous which warrants further studies to better understand underlying mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The current standard treatment for patients with locally advanced resectable oesophageal cancer (OeC) with curative intent is multimodal therapy, either with neoadjuvant chemoradiotherapy (nCRT) according to the CROSS trial or combination chemotherapy according to the OE02 trial, both followed by surgical resection [1,2,3]. Although the addition of neoadjuvant treatment offers a survival benefit compared to surgery alone, survival remains poor with 5-year overall survival rates varying between 23 and 47% [3, 4].
A pathological complete response (tumour regression grade [TRG] 1 according to Mandard) of the primary tumour in the resected specimen has been reported in up to 29% of OeC patients treated with nCRT [2, 5]. On the other hand, 38% of OeC patients have limited or no signs of response (TRG 3-5). TRG of the primary tumour has been suggested as a prognostic factor [6]. However, presence of lymph node metastasis (LNmets), their anatomical location and TRG in LNmets (LN-TRG) are potentially better predictors of patient’s survival than TRG of the primary tumour [7,8,9,10]. Kadota et al. illustrated the relationship between nCRT response in lymph nodes (LNs) and prognosis in patients with OeC [10]. Furthermore, Philippron et al. showed that even if no viable tumour is found in LNs but LNs show signs of tumour regression, survival is worse compared to patients with truly negative LNs (no evidence of tumour or tumour regression) [11]. These studies suggest that LN-TRG after nCRT and location of LNmets in relation to the radiation field may be important factors for OeC patient’s prognosis. However, previous studies did not evaluate whether there is a relationship between LN location with respect to the radiotherapy (RT) field and LN-TRG.
Elective lymph node irradiation (ENI) and two-field lymphadenectomy are commonly used in OeC patient management to prevent local recurrence and distant metastases. Current ENI guidelines recommend focusing elective irradiation on locoregional LN stations; however, the optimal extent is still under debate [12, 13].
We hypothesized that all LNmets located within the radiotherapy (RT) field will show evidence of tumour regression, confirming current clinical practice [1].
The aim of this study was to investigate the pathological TRG in individual LNmets and relate the results to their location within the RT field in a series of OeC patients treated with nCRT followed by surgical resection.
Materials and methods
Patients and treatment
This research has been approved by the Medical Ethical Commission of the Zuyderland Medical Center (Heerlen, NL). All patients diagnosed with oesophageal cancer (OeC) between 2010 and 2016 at the Zuyderland Medical Center (Heerlen, The Netherlands) with clinical TNM 7th edition stage IB–IIIC disease treated with neoadjuvant chemoradiotherapy (nCRT) followed by surgery were included in this study. Clinical assessment according to the Dutch OeC guidelines included fluorodeoxyglucose positron emission tomography (FDG PET/CT) scanning [14]. Approximately 6–10 weeks after completion of nCRT, a re-evaluation PET/CT scan was performed to assess radiological response to therapy and rule out presence of distant metastatic disease. Most patients were treated according to the CROSS trial schedule [2]. Depending on primary tumour location and patient performance status either a minimally invasive transhiatal oesophagogastrectomy including a one-field low mediastinal lymph node (LN) dissection, or a minimal invasive transthoracic approach with Ivor-Lewis-type resection and a two-field LN dissection was performed. All patients had an oesophageal reconstruction using the stomach.
Radiotherapy planning
A respiratory-gated 4D CT scan was used for RT planning purposes and the following regions of interest were delineated using all diagnostic information available: the gross tumour volume (GTV) defined as the macroscopic outline of the primary tumour and any pathological LNs if applicable; the clinical target volume (CTV) defined as the GTV plus a radial margin of 0.5 cm for LNs or 1 cm for primary tumour, a 3 cm margin in proximal and distal direction and inclusion of elective regional LN regions [12]; the planning target volume (PTV) margin added to account for day-to-day variation in patient positioning and breathing movements. RT was planned to ensure that 99% of the PTV received 95% of the nominal dose of 41.4 Gy, while conforming to the dose constraints of the organs-at-risk (e.g., lungs, heart, and spinal cord). Most patients were radiated 5 days per week in fractions of 1.8 Gy, up to a total of 23 fractions. Concurrently, patients received weekly carboplatin (doses titrated to achieve an area under the curve of 2 mg per milliliter per minute) and paclitaxel (50 mg/m2 of body-surface area) for 5 weeks [2]. A minority of patients were treated with 28 × 1.8 Gy.
Pathology
The surgeon marked the anatomical location of individual LN stations with different coloured beads in the resected specimen according to Casson et al. [15, 16]. In the histopathology laboratory, the fatty tissue was dissected per marked LN station and searched for LNs. All LNs were completely embedded separately by LN station. Tissue was processed into paraffin blocks as per standard protocol. Histopathological examination of the Haematoxylin/Eosin (HE) stained slides was performed by experienced gastrointestinal pathologists. TNM classification 7th ed. was used for tumour staging, grade of differentiation was determined according to the WHO criteria, and the regression of the primary tumour was assessed using the tumour regression grading system according to Mandard [5, 17, 18].
For the current study, all HE slides from all patients were retrieved retrospectively from the pathology archive and scanned at 20 × magnification using a Panoramic 250 scanner (3DHistech, Budapest, Hungary). Scanned slides with LNs were identified, reviewed and classified according to Martin-Romano et al. by at least two observers as: TRG-A: ‘true-negative’ LN without evidence of tumour or tumour regression; TRG-B: LN with viable tumour without evidence of tumour regression (no fibrosis, no mucin pools); TRG-C: LN with viable tumour and evidence of tumour regression (fibrosis or mucin pools or both); TRG-D: LN without viable tumour and evidence of tumour regression (fibrosis or mucin pools or both) interpreted as ‘complete tumour regression’ [19] (Fig. 1). Patients with only TRG-A LNs were classified as ‘true_ypN0’; while, patients with only TRG-D LNs were classified as ‘complete responders’. All other patients were classified as ‘incomplete responders’ (see Table 1).
Data collection and statistics
Patients were followed up according to standard clinical practice in referring hospitals. Overall survival (OS) time was defined as the time from the last RT fraction to the date of death or last follow-up. Date of death was available from the Dutch population register, and median follow-up time was determined using the ‘inverse Kaplan–Meier’ method [20]. Patient and tumour characteristics (sex, age, tumour location and clinical TNM stage) were retrieved from hospital medical records. The relationship between patient and tumour characteristics and LN-TRG was investigated using the Chi-square test for categorical variables or single-factor ANOVA for continuous variables.
Based on the maps published by Casson et al., the anatomical location of resected LNs was determined using the surgery and histopathology reports [15, 16]. Planning CT scans, RT fields and tumour contours were retrospectively reviewed by two experienced radiation oncologists. Based on anatomical landmarks, individual anatomical LN stations were categorized as being ‘inside’ or ‘outside’ of the RT field/PTV.
Baseline characteristics were compared between the three LN-TRG groups. The relationship between pathological parameters and LN-TRG groups was only analyzed for patients with either TRG-B, TRG-C or TRG-D lymph nodes, thus excluding ‘true_ypN0 patients’ from the analyses. The same cohort was used in the multivariate survival analysis. The relationship between LN location within the RT field (yes/no), pathological TRG of individual LNs, primary tumour TRG and resection margin status was analyzed using multivariate Cox regression analysis. One patient was excluded from the survival analysis due to missing data. P-values less than 0.05 were considered significant.
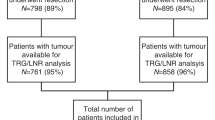
Results
In total, 117 patients with clinical stage IB–IIIC oesophageal cancer were included in this study. At the time of analysis, 60 patients were still alive; their median follow-up time was 37 months (95%CI: 29–44 months). Median (range) time between end of nCRT and surgery was 10 weeks (IQR: 9–12 weeks). Clinical characteristics of the patient cohort are provided in Table 2.
Resected lymph nodes
A total of 2565 LNs was resected, with a median (range) of 20 LNs per patient (6–51 LNs). LNmets were most commonly found in LN stations 17–20 (left gastric artery, common hepatic artery, splenic artery, and celiac axis). For a summary of the frequency of LNs and LNmets per resected LN station, see supplementary table S1. Histopathological characteristics of the resection specimens are available in Table 3.
Relationship between tumour regression in lymph nodes and overall survival
In 54 (46%) patients, none of the resected LNs contained tumour or had signs of tumour regression (i.e. all LNs were classified as TRG-A nodes). These patients were classified as ‘true_ypN0’. Overall survival (OS) of the ‘true_ypN0’ patients was significantly longer compared to all other patients (p = 0.002), with median overall survival of 52 months and 19 months, respectively, see Fig. 2.
In 63 (54%) patients, a total of 264 LNs contained tumour with or without evidence of regression: 56 (21%) TRG-B, 104 (39%) TRG-C and 104 (39%) TRG-D. 17 (27%) patients were classified as complete LN responders as they had only TRG-D LNs, and 46 (73%) as ‘incomplete LN responders’ as they had vital tumour in at least one LN. There was no difference in OS between true_ypN0 patients (n = 54) and patients in the complete LN responder group (n = 17) (Fig. 2, p = 0.969). There was a significant difference in OS between ypN + patients and true_ypN0/complete LN responders (Fig. 2, p < 0.001, p = 0.017, respectively).
Relationship between clinicopathological data and patients grouped by TRG in lymph nodes
As can be seen in Table 2, baseline clinical characteristics including age, sex, and histology were similar between the patients classified as ‘true_ypN0’, ‘complete LN responders’ or ‘incomplete LN responders’. For the following analyses, ‘true_ypN0’ patients were excluded, leaving 63 patients for analysis. There was a significant relationship between patients classified as ‘complete LN responders’ or ‘incomplete LN responders’ and ypT-stage (p = 0.042), number of resected LN stations (p = 0.033) and anatomical location of the resected LNs (p = 0.035). There was no significant relationship between ‘complete LN responders’ or ‘incomplete LN responders’ and total number of resected LNs (p = 0.693) and TRG of the primary tumour (p = 0.056).
Tumour regression in lymph nodes, location within the radiotherapy field and survival
In depth analysis of the LNs within/outside the RT field focused on the 63 patients with LNmets or LNs with signs of regression, i.e., the ‘complete LN responders’ and ‘incomplete LN responders’. 193 (73%) of the 264 LNmets were found to be located within the planned RT field. 13 of the 264 (5%) LNs from 9 patients were located outside the RT field. Four of these LNs were TRG-B LNs, 8 TRG-C LNs and one TRG-D LN. In 58 LNs (22%), the exact anatomical LN location and, thus, the relation to the RT field could not be ascertained, these were excluded from the analysis. In 7 (78%) of the 9 patients with LNmets outside the RT field, these were located paratracheal/subcarinal with the primary tumour located in the distal oesophagus (2 patients) or at the gastroesophageal junction (5 patients). The other 2 (22%) patients had a primary tumour above the diaphragm with LNmets outside the RT field in the abdominal LN stations. The RT plan of a patient with a LN showing complete regression outside the RT field is illustrated in Fig. 3. There was no significant relationship between LN-TRG and anatomical location of the LN within the RT field (p = 0.052, supplementary table S2), probably related to small number of patients. Outside the RT field, 69% of LNmets had signs of tumour regression (Fig. 4).
Univariate Cox regression revealed a significant relationship between OS and the number of TRG-B LNs located within the RT field [hazard ratio (HR) 1.1, 95% CI 1–1.3] (table S3). Patients with TRG-B LNs within the RT field had a significantly shorter OS than patients without TRG-B LNs within the RT field, 14 and 29 months, respectively (p < 0.001) (Fig. 5).
Univariate analysis comparing TRG of the primary tumour showed that patients with TRG-1 or TRG-2 in the primary tumour had significantly better survival compared to patients with TRG-3, TRG-4 or TRG-5 in the primary tumour (p = 0.009).
Multivariate overall survival analysis
In multivariate analysis, resection margin status (p = 0.04) and presence of TRG-B LNs in the RT field (p = 0.01) were the only factors significantly related to survival (for details, see Table 4). The regression grade of the primary tumour was not related to survival in multivariate analysis (p = 0.69).
Heterogeneity in lymph node TRG
Notably, in some patients, a highly heterogeneous LN-TRG was observed. Five (8%) patients had LNs within all three LN-TRG categories (B, C, D) and another 27 (42%) patients had LNs within two of the three categories. In two patients, TRG-D LNs and TRG-B LNs were observed within the same LN station.
Discussion
Major pathological response in the primary tumour has been related to better overall survival in oesophageal cancer (OeC) patients [6]. However, tumour regression (TRG) in LNmets might be a better predictor of survival than pathological response in the primary tumour [12]. In this study of OeC patients treated with neoadjuvant chemoradiotherapy (nCRT) followed by surgery, we aimed to analyze TRG in LNmets (LN-TRG) in relation to the LN location within the radiotherapy (RT) field and the relationship between LN-TRG and overall survival (OS).
We showed that patients without LNmets and without evidence of LN-TRG, e.g., the ‘true_ypN0’ patients, had a significantly better OS compared to patients with LNmets. Also, patients with evidence of a complete response in their LNs had a better survival than ypN+ patients. Patients in the ‘incomplete responder’ group with one or more LNmets without any sign of tumour regression (TRG-B LNs) had poorer survival than patients in this group with LNmets all showing signs of regression (TRG-C LNs) which was also confirmed in multivariate analysis. These findings support previous findings that LN-TRG might predict OeC patient survival [12]. Our study results suggest that LN-TRG might be related to primary tumour response, a finding which one might expect but to the best of our knowledge has not been reported in the literature. The presence of TRG-B LNs was significantly related to survival in multivariate analysis, when the TRG of the primary tumor was included in the model. Our finding that LN-TRG seems to be a better prognostic factor after chemoradiotherapy than TRG in the primary tumour validates results reported previously by Davies et al. and Urakawa et al. [21, 22].
After nCRT, 40% of OeC patients had evidence of LNmets, which is much lower than at time of diagnosis when 75% of the patients was staged as cN+. This difference can be explained by the complete LN responders (15% of all patients) and the fact that over 60% of the true_ypN0 patients were diagnosed as cN+ prior to treatment suggesting a clinical overdiagnosis of N+ patients. This could be due to false-positive detection in radiological imaging or an incorrect pathological N-stage due to an incomplete lymphadenectomy [23, 24].
We hypothesized that all LNmets within the RT field would show some degree of tumour regression; whereas, this would not apply to LNmets outside the RT field. However, our results do not entirely confirm this hypothesis, as there seems to be a relationship between the location of the LNmets and the regression seen in the LN. But this result is only borderline significant in our study, probably due to small number of patients. The tumour regression seen in LNmets outside the RT field could be explained by the concomitant administered systemic chemotherapy. This chemotherapy will reach the LNs outside the RT field and it is known, from the OE02 trial, that patients treated with chemotherapy have nodal response [11]. Another possibility is that LNs outside the RT field show tumour regression due to a systemic immunological response to the tumour, known as the abscopal effect [25]. However, the fact that LNs of the same patient found within the same LN station can have completely different responses to nCRT was surprising. We hypothesize that this might be due to a difference in blood supply, allowing more chemotherapy to reach the LNmet with the better blood supply. Second, it could be due to tumour clonality or be related to the immune cell population present in the lymph node. It is well known that cancer cells can be highly heterogeneous even within patients [26, 27]. Clonality can be a major factor contributing to resistance against neoadjuvant therapies [28]. Although we have currently no evidence for this, it might be that different clones of the tumour with different resistance patterns populated the LNs located within the same LN station.
Our study has some limitations. As treatment of OeC patients changed with the publication of the CROSS trial results, we do not have a contemporary group of non-neoadjuvant-treated OeC patients. So, we were unable to assess whether LNs can show fibrosis even if there has been no neoadjuvant treatment. Assessment with certainty, whether LNs were located in or outside the RT field, was difficult in borderline cases. However, the PTV was used as uncertainty margin which compensates this partly. From 24% of the resected LNs, the exact anatomical location was not traceable as they were located in undefined fatty tissue attached to the resected specimen. However, as most were found closely to the tumour, we assume that most of them were radiated. Unfortunately, data on recurrence pattern were not available to us for analysis in the current study. Urakawa et al. have shown that in the metastatic setting, the response of the LN to chemotherapy can predict long-term survival and recurrence [22]. They found that LN non-responders presented more often with lymphatic and/or haematogenous recurrence and dissemination compared to LN responders. Results that are statistically not significant can be a consequence from the low number of participants resulting in a lack of power, future studies including more patients are needed to confirm these results.
In conclusion, this study showed a number of novel potentially clinically relevant findings. First of all, if tumour-positive LNs are found, the more tumour regression LNs show, the better the survival. Second, LNs outside the RT field can show tumour regression and even though a LN has been irradiated with the full dose, it might not show any response. Third, TRG in the LN has been shown to be related to TRG in the primary tumour. And lastly, LN-TRG within a patient can be extremely heterogenous, even LNs within the same LN station of the same patient can respond differently. Given the low incidence of LNmets outside the RT field, mainly in remote regions, this study provides no evidence for enlarging the RT field. However, further research is needed to detect LNmets more accurately during clinical staging and to better understand the heterogeneous LN-TRG seen in OeC patients.
Abbreviations
- LN-TRG:
-
Tumour regression in lymph nodes
- nCRT:
-
Neoadjuvant chemoradiotherapy
- LNs:
-
Lymph nodes
- RT:
-
Radiotherapy
- OeC:
-
Oesophageal cancer
- TRG:
-
Tumour regression grade
- ENI:
-
Elective lymph node irradiation
- LNmets:
-
Lymph node metastasis
- LN:
-
Lymph node
- GTV:
-
Gross tumour volume
- CTV:
-
Clinical target volume
- PTV:
-
Planning target volume
References
Lordick F, Mariette C, Haustermans K, Obermannova R, Arnold D. Oesophageal cancer: eSMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v50–7.
van Hagen P, Hulshof MC, van Lanschot JJ, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366(22):2074–84.
Allum WH, Stenning SP, Bancewicz J, Clark PI, Langley RE. Long-term results of a randomized trial of surgery with or without preoperative chemotherapy in esophageal cancer. J Clin Oncol. 2009;27(30):5062–7.
Shapiro J, van Lanschot JJB, Hulshof M, et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 2015;16(9):1090–8.
Mandard AM, Dalibard F, Mandard JC, et al. Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma. Clinicopathologic correlations. Cancer. 1994;73(11):2680–6.
Tomasello G, Petrelli F, Ghidini M, et al. Tumor regression grade and survival after neoadjuvant treatment in gastro-esophageal cancer: a meta-analysis of 17 published studies. Eur J Surg Oncol. 2017;43(9):1607–16.
Smyth EC, Fassan M, Cunningham D, et al. Effect of pathologic tumor response and nodal status on survival in the medical research council adjuvant gastric infusional chemotherapy trial. J Clin Oncol. 2016;34(23):2721–7.
Davarzani N, Hutchins GGA, West NP, et al. Prognostic value of pathological lymph node status and primary tumour regression grading following neoadjuvant chemotherapy—results from the MRC OE02 oesophageal cancer trial. Histopathology. 2018;72(7):1180–8.
Anderegg MC, Lagarde SM, Jagadesham VP, et al. Prognostic significance of the location of lymph node metastases in patients with adenocarcinoma of the distal esophagus or gastroesophageal junction. Ann Surg. 2016;264(5):847–53.
Kadota T, Hatogai K, Yano T, et al. Pathological tumor regression grade of metastatic tumors in lymph node predicts prognosis in esophageal cancer patients. Cancer Sci. 2018;109(6):2046–55.
Philippron A, Bollschweiler E, Kunikata A, et al. Prognostic relevance of lymph node regression after neoadjuvant chemoradiation for esophageal cancer. Semin Thorac Cardiovasc Surg. 2016;28(2):549–58.
Van De Voorde L, Larue RTHM, Pijls M, et al. A qualitative synthesis of the evidence behind elective lymph node irradiation in oesophageal cancer. Radiother Oncol. 2014;113(2):166–74.
Li B, Chen H, Xiang J, et al. Pattern of lymphatic spread in thoracic esophageal squamous cell carcinoma: a single-institution experience. J Thorac Cardiovasc Surg. 2012;144(4):778–85 (discussion 785–776).
Oncoline. Dutch guidlines stomach carcinoma. 2014; https://www.oncoline.nl/maagcarcinoom. Accessed 15 Dec 2019.
Casson AG, Rusch VW, Inculet RI, Ginsberg RJ, Zankowicz N, Rosenberg JC, et al. Lymph node mapping for resectable carcinoma of the esophagus: a guide for thoracic surgeons. Princeton, NJ: Bristol-Myers Oncology Division; 1992.
Rice TW, Gress DM, Patil DT, Hofstetter WL, Kelsen DP, Blackstone EH. Cancer of the esophagus and esophagogastric junction—major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA. 2017;67(4):304–317.
Rice TW, Blackstone EH, Rusch VW. 7th edition of the AJCC Cancer Staging Manual: esophagus and esophagogastric junction. Ann Surg Oncol. 2010;17(7):1721–4.
Hamilton SR, Aaltonen LA. World Health Organization Classification of Tumours. Pathology and genetics of tumours of the digestive system. Lyonn: IARC Press; 2000.
Martin-Romano P, Sola JJ, Diaz-Gonzalez JA, et al. Role of histological regression grade after two neoadjuvant approaches with or without radiotherapy in locally advanced gastric cancer. Br J Cancer. 2016;115(6):655–63.
Schemper M, Smith TL. A note on quantifying follow-up in studies of failure time. Control Clin Trials. 1996;17(4):343–6.
Davies AR, Myoteri D, Zylstra J, et al. Lymph node regression and survival following neoadjuvant chemotherapy in oesophageal adenocarcinoma. Br J Surg. 2018;105(12):1639–49.
Urakawa S, Makino T, Yamasaki M, et al. Lymph node response to neoadjuvant chemotherapy as an independent prognostic factor in metastatic esophageal cancer. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003445.
Grimm H, Binmoeller KF, Hamper K, Koch J, Henne-Bruns D, Soehendra N. Endosonography for preoperative locoregional staging of esophageal and gastric cancer. Endoscopy. 1993;25(3):224–30.
Lerut T, Flamen P, Ectors N, et al. Histopathologic validation of lymph node staging with FDG-PET scan in cancer of the esophagus and gastroesophageal junction: a prospective study based on primary surgery with extensive lymphadenectomy. Ann Surg. 2000;232(6):743–52.
Yilmaz MT, Elmali A, Yazici G. Abscopal effect, from myth to reality: from radiation oncologists’ perspective. Cureus. 2019;11(1):e3860–e3860.
Meacham CE, Morrison SJ. Tumour heterogeneity and cancer cell plasticity. Nature. 2013;501(7467):328–37.
Burrell RA, Swanton C. Tumour heterogeneity and the evolution of polyclonal drug resistance. Mol Oncol. 2014;8(6):1095–111.
Findlay JM, Castro-Giner F, Makino S, et al. Differential clonal evolution in oesophageal cancers in response to neo-adjuvant chemotherapy. Nat Commun. 2016;7:11111.
Funding
This study received no funding.
Author information
Authors and Affiliations
Contributions
WJK: study design, data acquisition, data analysis, manuscript preparation and editing. RTHML: study design, data acquisition, data analysis, manuscript preparation and editing. MK: data analysis for the revision, manuscript editing, manuscript reviewing. JR: data analysis for the revision, manuscript editing, manuscript reviewing. IC: data analysis, manuscript editing, manuscript reviewing. RGR: data acquisition, manuscript reviewing. LH: data analysis, data acquisition, manuscript editing, manuscript reviewing. WE: data analysis, manuscript editing, manuscript reviewing. MB: data analysis, manuscript editing, manuscript reviewing. JB: data analysis, manuscript editing, manuscript reviewing. PL: data analysis, manuscript editing, manuscript reviewing. MNS: study design, data analysis, manuscript editing, manuscript reviewing. HIG: study design, slide review, data analysis, manuscript reviewing and editing.
Corresponding author
Ethics declarations
Ethical statement
This research has been approved by the Medical Ethical Commission of the Zuyderland medical center. The study was performed in accordance with the Declaration of Helsinki.
Conflict of interest
All authors declare to have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koemans, W.J., Larue, R.T.H.M., Kloft, M. et al. Lymph node response to chemoradiotherapy in oesophageal cancer patients: relationship with radiotherapy fields. Esophagus 18, 100–110 (2021). https://doi.org/10.1007/s10388-020-00777-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-020-00777-y