Abstract
Background
Gastroesophageal reflux disease (GERD) is a common gastrointestinal disorder. Proton pump inhibitors (PPIs) are first-line drugs for GERD. For those who fail to respond to PPIs, adding prokinetics to PPIs is recommended and several trials have been conducted to evaluate the efficacy of prokinetic–PPI combination therapy.
Methods
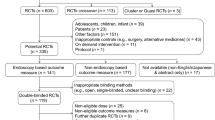
A systematic literature search was performed using PubMed and the Cochrane Library databases before February 2019 for randomized controlled trials (RCTs), which compared the efficacy of prokinetics plus PPI treatment with that of PPI monotherapy. Relevant studies were examined and data were extracted independently by two investigators. The risk ratios (RRs) with 95% CIs were used to evaluate the responder rate, and standard mean differences (SMDs) or mean differences (MDs) with 95% CIs were used for symptom score changes. Statistical heterogeneity was evaluated by the I2 statistic. Either a fixed-effect or a random-effect model was established for calculating the pooled data.
Results
A total of 14 studies, comprising 1,437 patients were ultimately included in the meta-analysis. The pooled analysis showed that compared to PPI monotherapy, addition of prokinetics to PPI did not elevate the rate of endoscopic responders (RR = 0.996, 95% CI 0.929 − 1.068, p = 0.917), but improved symptom response (RR = 1.185, 95% CI 1.042 − 1.348, p = 0.010). Additionally, the combined therapy achieved a greater symptom relief than monotherapy both in FSSG and GERD-Q subgroups (MD = − 2.978, 95% CI − 3.319 to − 2.638, p < 0.001; MD = − 0.723, 95% CI − 0.968 to − 0.478, p < 0.001).
Conclusions
Adding prokinetics to PPIs achieves symptomatic improvement compared to PPI monotherapy, thus can enhance life quality of GERD patients. However, the combined treatment seems to have no significant effect on mucosal healing.



Similar content being viewed by others
References
Vakil N, van Zanten SV, Kahrilas P, et al. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–20 (quiz 1943).
El-Serag HB, Sweet S, Winchester CC, et al. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63:871–80.
Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67:1351–62.
Richter JE, Rubenstein JH. Presentation and epidemiology of gastroesophageal reflux disease. Gastroenterology. 2018;154:267–76.
Fock KM, Talley N, Goh KL, et al. Asia-Pacific consensus on the management of gastro-oesophageal reflux disease: an update focusing on refractory reflux disease and Barrett's oesophagus. Gut. 2016;65:1402–15.
Gyawali CP, Azagury DE, Chan WW, et al. Nonerosive reflux disease: clinical concepts. Ann NY Acad Sci. 2018;1434:290–303.
Iwakiri K, Kinoshita Y, Habu Y, et al. Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2015. J Gastroenterol. 2016;51:751–67.
Gyawali CP, Fass R. Management of gastroesophageal reflux disease. Gastroenterology. 2018;154:302–18.
Hershcovici T, Fass R. Pharmacological management of GERD: where does it stand now? Trends Pharmacol Sci. 2011;32:258–64.
Fass R, Shapiro M, Dekel R, et al. Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease–where next? Aliment Pharmacol Ther. 2005;22:79–94.
Marakhouski KY, Karaseva GA, Ulasivich DN, et al. Omeprazole-domperidone fixed dose combination vs omeprazole monotherapy: a phase 4, open-label, comparative, parallel randomized controlled study in mild to moderate gastroesophageal reflux disease. Clin Med Insights Gastroenterol. 2017;10:1179552217709456.
Zhang Q, Lehmann A, Rigda R, et al. Control of transient lower oesophageal sphincter relaxations and reflux by the GABA(B) agonist baclofen in patients with gastro-oesophageal reflux disease. Gut. 2002;50:19–24.
Yamashita H, Okada A, Naora K, et al. Adding acotiamide to gastric acid inhibitors is effective for treating refractory symptoms in patients with non-erosive reflux disease. Dig Dis Sci. 2019;64:823–31.
Lee JY, Kim SK, Cho KB, et al. A double-blind, randomized, multicenter clinical trial investigating the efficacy and safety of esomeprazole single therapy versus mosapride and esomeprazole combined therapy in patients with esophageal reflux disease. J Neurogastroenterol Motility. 2017;23:218–28.
Madan K, Ahuja V, Kashyap PC, et al. Comparison of efficacy of pantoprazole alone versus pantoprazole plus mosapride in therapy of gastroesophageal reflux disease: a randomized trial. Dis Esophagus. 2004;17:274–8.
van Rensburg CJ, Bardhan KD. No clinical benefit of adding cisapride to pantoprazole for treatment of gastro-oesophageal reflux disease. Eur J Gastroenterol Hepatol. 2001;13:909–14.
Kimmig JM. Treatment and prevention of relapse of mild oesophagitis with omeprazole and cisapride: comparison of two strategies. Aliment Pharmacol Ther. 1995;9:281–6.
Takeuchi T, Takahashi Y, Kawaguchi S, et al. Therapy of gastroesophageal reflux disease and functional dyspepsia overlaps with symptoms after usual-dose proton pump inhibitor: acotiamide plus usual-dose proton pump inhibitor versus double-dose proton pump inhibitor. J Gastroenterol Hepatol. 2018;33:623–30.
Yamashita H, Kanamori A, Okada A. Efficacy of acotiamide in patients with gastroesophageal reflux disease unresponsive to proton pump inhibitor therapy. United Eur Gastroenterol J. 2016;4:A22–A23.
Wang YP, Ji LS, Ni M, et al. Clinical effects of esomeprazole combined with mosapride for treatment of gastroesophageal reflux disease. World Chin J Digestol. 2014;22:5671–4.
Cho YK, Choi MG, Park EY, et al. Effect of mosapride combined with esomeprazole improves esophageal peristaltic function in patients with gastroesophageal reflux disease: a study using high resolution manometry. Dig Dis Sci. 2013;58:1035–41.
Miwa H, Inoue K, Ashida K, et al. Randomised clinical trial: efficacy of the addition of a prokinetic, mosapride citrate, to omeprazole in the treatment of patients with non-erosive reflux disease - a double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2011;33:323–32.
Yamaji Y, Isomura Y, Yoshida S, et al. Randomized controlled trial comparing the efficacy of mosapride plus omeprazole combination therapy to omeprazole monotherapy in gastroesophageal reflux disease. J Digest Dis. 2014;15:469–76.
Abbasinazari M, Panahi Y, Mortazavi SA, et al. Effect of a combination of omeprazole plus sustained release baclofen versus omeprazole alone on symptoms of patients with Gastroesophageal Reflux Disease (GERD). Iran J Pharmaceutical Res. 2014;13:1221–6.
Ndraha S. Combination of PPI with a prokinetic drug in gastroesophageal reflux disease. Acta medica indonesiana. 2011;43:233–6.
Hsu YC, Yang TH, Hsu WL, et al. Mosapride as an adjunct to lansoprazole for symptom relief of reflux oesophagitis. Br J Clin Pharmacol. 2010;70:171–9.
Marakhouski KY, Karaseva GA, Ulasivich DN, et al. Omeprazole-domperidone fixed dose combination vs omeprazole monotherapy: a phase 4, open-label, comparative, parallel randomized controlled study in mild to moderate gastroesophageal reflux disease. Clin Med Insights. 2017;10:1179552217709456.
Sigterman KE, van Pinxteren B, Bonis PA, et al (2013) Short-term treatment with proton pump inhibitors, H2-receptor antagonists and prokinetics for gastro-oesophageal reflux disease-like symptoms and endoscopy negative reflux disease. Cochrane Database Syst Rev Cd002095.
Sifrim D, Zerbib F. Diagnosis and management of patients with reflux symptoms refractory to proton pump inhibitors. Gut. 2012;61:1340–54.
Mermelstein J, Chait Mermelstein A, Chait MM. Proton pump inhibitor-refractory gastroesophageal reflux disease: challenges and solutions. Clin Exp Gastroenterol. 2018;11:119–34.
Gralnek IM, Dulai GS, Fennerty MB, et al. Esomeprazole versus other proton pump inhibitors in erosive esophagitis: a meta-analysis of randomized clinical trials. Clin Gastroenterol Hepatol. 2006;4:1452–8.
Khan M, Santana J, Donnellan C, et al (2007) Medical treatments in the short term management of reflux oesophagitis. Cochrane Database Syst Rev Cd003244.
Kung YM, Hsu WH, Wu MC, et al. Recent advances in the pharmacological management of gastroesophageal reflux disease. Dig Dis Sci. 2017;62:3298–316.
Funding
The work was supported by Jiangsu Provincial Key Research and Development Plan (No. BE2018659) and Provincial Key Laboratory Program of Higher Education (No. KJS1867).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
All analyses were based on previous published studies, thus no ethical approval and patient consent are required.
Conflict of interest
The authors deny any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10388_2020_753_MOESM1_ESM.tif
Supplementary Figure 1 Sensitivity analysis in which the meta-analysis of symptom score changes is re-estimated by omitting each study in turn (TIF 1498 kb)
10388_2020_753_MOESM2_ESM.tif
Supplementary Figure 2 Meta-analysis of the symptom response. a: symptom response in NERD patients; b: symptom response in RE patients (TIF 5366 kb)
Rights and permissions
About this article
Cite this article
Xi, L., Zhu, J., Zhang, H. et al. The treatment efficacy of adding prokinetics to PPIs for gastroesophageal reflux disease: a meta-analysis. Esophagus 18, 144–151 (2021). https://doi.org/10.1007/s10388-020-00753-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-020-00753-6