Abstract
Purpose
There are only a few epidemiological studies of dry eye syndrome (DES) in populations with a common academic background. in this study, the prevalence of DES and associated factors were evaluated separately in men and women physical education and sports science graduates.
Study design
Cross-sectional survey.
Methods
A questionnaire about the diagnosis of DES and associated factors was mailed to 9507 graduates of the Faculty of Health and Sports Science, Juntendo University. The questions covered subjective DES using Schaumberg et al.’s questionnaire and the prevalence of diagnosed DES. Associated factors, age, sex, smoking, alcohol consumption, body mass index, daily screen viewing time, and contact lens (CL) use were analyzed.
Results
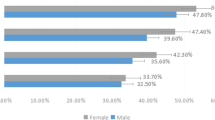
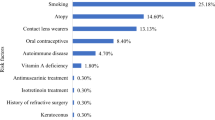
A total of 2048 valid responses were received. The prevalence of diagnosed DES was 2.9% in men and 9.3% in women. For subjective DES, the prevalence was 14.8% in men and 39.8% in women. The odds ratio for DES was high in men and women who used CLs and women whose daily screen viewing time was ≥ 4 h.
Conclusion
Both diagnosed and subjective DES were highly prevalent in men and women of all ages, particularly among those in their 20 and 30s. CL use was associated with DES in both men and women. Measures to deal with the factors that can be corrected might have a positive effect on the ocular health and quality of life of physical education and sports science graduates.
Similar content being viewed by others
References
Shimazaki J, Yokoi N, Watanabe H, Amano S, Ohashi Y, Kinoshita S, et al. Definition and diagnosis of dry eye in Japan, 2016. Atarashii Ganka. 2017;34:309–13. (in Japanese).
Miljanović B, Dana R, Sullivan DA, Schaumberg DA. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol. 2007;143:409–15.
Management and therapy of dry eye disease: report of the Management and Therapy Subcommittee of the International Dry Eye Workshop (2007). Ocul Surf. 2007;5:163 – 78.
Murakami S, Ohto-Fujita E, Kohmura Y, Shiraishi Y, Aoki K, Sawaki K, et al. Current situation regarding visual correction methods in university athletes and associated issues. Jpn J Clin Sports Med. 2013;21:658–63.
Murakami S, Kohmura Y, Shiraishi Y, Aoki K, Nakata M, Hamano R, et al. Dry eye among undergraduate students studying sports-related subjects: current status and associated issues. Gazz Med Ital. 2019;178:126–31.
Uchino M, Schaumberg DA, Dogru M, Uchino Y, Fukagawa K, Shimmura S, et al. Prevalence of dry eye disease among japanese visual display terminal users. Ophthalmology. 2008;115:1982–8.
Uchino M, Yokoi N, Uchino Y, Dogru M, Kawashima M, Komuro A, et al. Prevalence of dry eye disease and its risk factors in visual display terminal users: the Osaka study. Am J Ophthalmol. 2013;156:759–66.
Uchino M, Dogru M, Uchino Y, Fukagawa K, Shimmura S, Takebayashi T, et al. Japan Ministry of Health study on prevalence of dry eye disease among japanese high school students. Am J Ophthalmol. 2008;146:925–9.
Uchino M, Nishiwaki Y, Michikawa T, Shirakawa K, Kuwahara E, Yamada M, et al. Prevalence and risk factors of dry eye disease in Japan: Koumi study. Ophthalmology. 2011;118:2361–7.
Inomata T, Iwagami M, Nakamura M, Shiang T, Yoshimura Y, Fujimoto K, et al. Characteristics and risk factors associated with diagnosed and undiagnosed symptomatic dry eye using a smartphone application. JAMA Ophthalmol. 2019;138:58–68.
Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136:318–26.
Gulati A, Sullivan R, Buring JE, Sullivan DA, Dana R, Schaumberg DA. Validation and repeatability of a short questionnaire for dry eye syndrome. Am J Opthalmol. 2006;142:125–31.
Schaumberg DA, Buring JE, Sullivan DA, Dana MR. Hormone replacement therapy and dry eye syndrome. JAMA. 2001;286:2114–9.
Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, et al. TFOS DEWS II Epidemiology Report. Ocul Surf. 2017;15:334–65.
Tsugane S, Sasaki S, Tsubono Y. Under- and overweight impact on mortality among middle-aged japanese men and women: a 10-y follow-up of JPHC study cohort I. Int J Obes Relat Metab Disord. 2002;26:529–37.
Lee AJ, Lee J, Saw S-M, Gazzard G, Koh D, Widjaja D, et al. Prevalence and risk factors associated with dry eye symptoms: a population based study in Indonesia. Brit J Ophthalmol. 2002;86:1347–51.
Sato N, Yamada M, Tsubota K. Visual display terminal work and dry eye. Atarashii Ganka. 1992;9:2103–6. (in Japanese).
Nichols JJ, King-Smith PE. Thickness of the pre-and post-contact lens tear film measured in vivo by interferometry. Investig Opthalmol Vis Sci. 2003;44:68–77.
Maruyama K, Yokoi N, Takamata A, Kinoshita S. Effect of environmental conditions on tear dynamics in soft contact lens wearers. Invest Ophthalmol Vis Sci. 2004;45:2563–8.
Chalmers R, Long B, Dillehay S, Begley C. Improving contact-lens related dryness symptoms with silicone hydrogel lenses. Optom Vis Sci. 2008;85:778–84.
Sand BB, Marner K, Norn MS. Sodium hyaluronate in the treatment of keratoconjunctivitis sicca. A double masked clinical trial. Acta Ophthalmol. 1989;67:181–3.
Hori Y, Muramatsu R. Tear supplementation: artificial tear and hyaluronate eye drops. Atarashii Ganka. 2015;32:931–4. (in Japanese).
Nakamura M, Hikida M, Nakano T, Ito S, Hamano T, Kinoshita S. Characterization of water retentive properties of hyaluronan. Cornea. 1993;12:433–6.
Yokoi N, Kato H, Kinoshita S. Facilitation of tear fluid secretion by 3% diquafosol ophthalmic solution in normal human eyes. Am J Ophthalmol. 2014;157:85–92.
Koh S, Ikeda C, Takai T, Watanabe H, Maeda N, Nishida K. Long-term results of treatment with diquafosol ophthalmic solution for aqueous-deficient dry eye. Jpn J Ophthalmol. 2013;57:440–6.
Shimazaki-Den S, Iseda H, Dogru M, Shimazaki J. Effects of diquafosol sodium eye drops on tear film stability in short BUT type of dry eye. Cornea. 2013;32:1120–5.
Yamaguchi M, Ohashi Y. 3% diquafosol ophthalmic solution promotes mucin and tear fluid. Atarashii Ganka. 2015;32:935–42. (in Japanese).
Kaido M, Uchino M, Kojima T, Dogru M, Tsubota K. Effect of diquafosol tetrasodium administration on visual function in short break-up time dry eye. J Ocul Pharmacol Ther. 2013;29:595–603.
Acknowledgements
The authors would like to thank the graduates and the J-Fit + Study for their cooperation.
This work was supported by the Joint Research Program of Juntendo University Faculty of Health and Sports Science and Institute of Health and Sports Science & Medicine, Juntendo University. The authors would also like to thank Forte Science Communications (Tokyo, Japan) for editorial assistance with the preparation of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
S. Murakami, None; Y. Kohmura, None; Y. Someya, None; K. Suzuki, None; K. Inoue, Grants or contracts (Teijin, Otsuka, Wakamoto), Lecture fee (Otsuka, HOYA, Pfizer, Senju, Santen, Allergan, Novartis, ZEISS); S. Amano, Payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events (Santen, AMO, Senju, Alcon, HOYA, Otsuka); K. Aoki, None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Shigeki Murakami
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Murakami, S., Kohmura, Y., Someya, Y. et al. Prevalence of dry eye syndrome and risk factors in physical education and sports science graduates. Jpn J Ophthalmol 67, 175–181 (2023). https://doi.org/10.1007/s10384-022-00973-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-022-00973-6