Abstract
Purpose
To investigate the correlations of thickness of three retinal layers with retinal displacement after idiopathic macular hole surgery.
Study design
Retrospective, consecutive, case series.
Methods
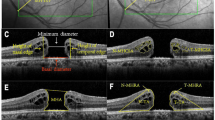
42 eyes of 42 patients undergoing macular hole surgery with internal limiting membrane peeling were studied. Retinal distance was measured with near-infrared images between the optic nerve and the intersection of retinal vessels at four quadrants. Retinal thicknesses of inner retinal layer, inner nuclear layer and outer retinal layer were measured 1000 μm away from the central fovea using Spectralis.
Results
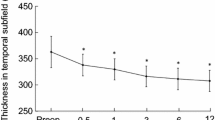
Retinal distances other than the nasal quadrant decreased postoperatively (p < 0.001). Retinal displacement (%) correlated significantly with the change in inner nuclear layer thickness in the temporal sector at 1, 3, and 6 months, in the superior sector at 2 weeks, 1, and 6 months, and in the inferior sector at 3 and 6 months postoperatively (r = 0.319–0.570, p < 0.001–0.040), but not in the inner or outer retinal layers.
Conclusion
Internal limiting membrane peeling for macular hole enhances retinal displacement toward the optic disc, whose distances correlate with the changes in inner nuclear layer thickness.






Similar content being viewed by others
References
Gass JD. Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol. 1988;106:629–39.
Gass JD. Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol. 1995;119:752–9.
Steel DHW, Lotery AJ. Idiopathic vitreomacular traction and macular hole: a comprehensive review of pathophysiology, diagnosis, and treatment. Eye (Lond). 2013;27(suppl 1):S1-21.
Wendel RT, Patel AC, Kelly NE, Salzano TC, Wells JW, Novack GD. Vitreous surgery for macular holes. Ophthalmology. 1993;100:1671–6.
Brooks HL. Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology. 2000;107:1939–48.
Christensen UC, Krøyer K, Sander B, Larsen M, Henning V, Villumsen J, et al. Value of internal limiting membrane peeling in surgery for idiopathic macular hole stage 2 and 3: a randomized clinical trial. Br J Ophthalmol. 2009;93:1005–15.
Lois N, Burr J, Norrie J, Vale L, Cook J, McDonald A, et al. Internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole: A pragmatic randomized controlled trial. Invest Ophthalmol Vis Sci. 2011;52:1586–92.
Kawano K, Ito Y, Kondo M, Ishikawa K, Kachi S, Ueno S, et al. Displacement of foveal area toward optic disc after macular hole surgery with internal limiting membrane peeling. Eye (Lond). 2013;27:871–7.
Ishida M, Ichikawa Y, Higashida R, Tsutsumi Y, Ishikawa A, Imamura Y. Retinal displacement toward optic disc after internal limiting membrane peeling for idiopathic macular hole. Am J Ophthalmol. 2014;157:971–7.
Pak KY, Park KH, Kim KH, Park SW, Byon IS, Kim HW, et al. Topographic changes of the macula after closure of idiopathic macular hole. Retina. 2017;37:667–72.
Akahori T, Iwase T, Yamamoto K, Ra EM, Kawano K, Ito Y, et al. Macular displacement after vitrectomy in eyes with idiopathic macular hole determined by optical coherence tomography angiography. Am J Ophthalmol. 2018;189:111–21.
Imamura Y, Ishida M. Retinal thinning after internal limiting membrane peeling for idiopathic macular hole. Jpn J Ophthalmol. 2018;62:158–62.
Yoshikawa M, Murakami T, Nishijima K, Uji A, Ogino K, Horii T, et al. Macular migration toward the optic disc after inner limiting membrane peeling for diabetic macular edema. Invest Ophthalmol Vis Sci. 2013;54:629–35.
Wollensak G, Spoerl E. Biomechanical characteristics of retina. Retina. 2004;24:967–70.
Conde C, Cáceres A. Microtubule assembly, organization and dynamics in axons and dendrites. Nat Rev Neurosci. 2009;10:319–32.
Hogan MJ, Alvarado JA, Weddell JE. Histology of the human eye: an atlas and textbook. Philadelphia: Saunders; 1971. p. 523–606.
Sheidow TG, Blinder KJ, Holekamp N, Joseph D, Shah G, Grand MG, et al. Outcome results in macular hole surgery: an evaluation of internal limiting membrane peeling with and without indocyanine green. Ophthalmology. 2003;110:1697–701.
Hashimoto Y, Saito W, Fujiya A, Yoshizawa C, Hirooka K, Mori S, et al. Changes in inner and outer retinal layer thicknesses after vitrectomy for idiopathic macular hole: implications for visual prognosis. PLoS ONE. 2015;10:e0135925.
Bringmann A, Pannicke T, Grosche J, Francke M, Wiedemann P, Skatchkov SV, et al. Müller cells in the healthy and diseased retina. Prog Retin Eye Res. 2006;25:397–424.
Matet A, Savastano MC, Rispoli M, Bergin C, Moulin A, Crisanti P, et al. En face optical coherence tomography of foveal microstructure in full-thickness macular hole: a model to study perifoveal Müller cells. Am J Ophthalmol. 2015;159:1142–51.
Hogan MJ, Alvarado JA, Weddell JE. Histology of the human eye: an atlas and textbook. Philadelphia: Saunders; 1971. p. 457–88.
Luby-Phelps K. Cytoarchitecture and physical properties of cytoplasm: volume, viscosity, diffusion, intracellular surface area. Int Rev Cytol. 2000;192:189–221.
Reichenbach A, Bringman A. Cell biology of retinal glia. In: Schachat A, editor. Ryan’s Retina. 6th ed. Amsterdam, The Netherlands: Elsevier; 2018. p. 466–87.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
A. Takeyama, None; Y. Imamura, None; T. Fujimoto, None; T. Iida, None; Y. Komiya, None; M. Shibata, None; M. Ishida, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Asuka Takeyama
About this article
Cite this article
Takeyama, A., Imamura, Y., Fujimoto, T. et al. Retinal displacement and intraretinal structural changes after idiopathic macular hole surgery. Jpn J Ophthalmol 66, 173–182 (2022). https://doi.org/10.1007/s10384-021-00887-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-021-00887-9