Abstract
Purpose
Our aim was to review the success rates of dacryoendoscopy-guided probing for recalcitrant congenital nasolacrimal duct obstruction (CNLDO).
Methods
We reviewed the medical records of 498 patients (521 eyes) diagnosed with CNLDO between January 2011 and November 2013. Of these, 54 eyes met the eligibility criteria and underwent probing with a dacryoendoscope.
Results
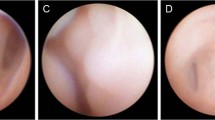
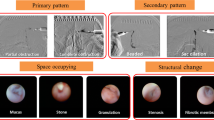
Of the 54 eyes, 21 were classified as failed cases at other hospitals, 13 as cases requiring conversion from blind to dacryoendoscopy-guided probing during surgery at our hospital, and 20 as cases requiring intervention under general anesthesia because of difficulty with topical anesthesia. The overall success rate with dacryoendoscopy was 98.1 % (53/54 eyes) at postoperative week 2 and 97.1 % (33/34 eyes) a year after surgery. Among the cases that failed at other hospitals, one showed the formation of five false passages in the middle area of the nasolacrimal duct. In 11 eyes, slit-like adhesion was confirmed as a blurred linear line at the distal end of the nasolacrimal duct. Patency could be smoothly achieved by releasing the adhesion.
Conclusions
Our study showed a high success rate for dacryoendoscopy-guided probing in CNLDO patients. The use of a dacryoendoscope allows direct visualization of the lacrimal passage and is likely to become necessary for managing CNLDO.



Similar content being viewed by others
References
Robb RM. Success rates of nasolacrimal duct probing at time intervals after 1 year of age. Ophthalmology. 1998;105:1307–9.
Kapadia MK, Freitag SK, Woog JJ. Evaluation and management of congenital nasolacrimal duct obstruction. Otolaryngol Clin N Am. 2006;39:959–77.
Kakizaki H, Takahashi Y, Kinoshita S, Shiraki K, Iwaki M. The rate of symptomatic improvement of congenital nasolacrimal duct obstruction in Japanese infants treated with conservative management during the 1st year of age. Clin Ophthalmol. 2008;2:291–4.
Nucci P, Capoferri C, Alfarano R, Brancato R. Conservative management of congenital nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus. 1989;26:39–43.
Petersen RA, Robb RM. The natural course of congenital obstruction of the nasolacrimal duct. J Pediatr Ophthalmol Strabismus. 1978;15:246–50.
Miller AM, Chandler DL, Repka MX, Hoover DL, Lee KA, Melia M, et al. Office probing for treatment of nasolacrimal duct obstruction in infants. J AAPOS. 2014;18:26–30.
Zwaan J. Treatment of congenital nasolacrimal duct obstruction before and after the age of 1 year. Ophthalmic Surg Lasers. 1997;28:932–6.
Repka MX, Chandler DL, Beck RW, Crouch ER 3rd, Donahue S, Holmes JM, et al. Primary treatment of nasolacrimal duct obstruction with probing in children younger than 4 years. Ophthalmology. 2008;115:577–84.
Honavar SG, Prakash VE, Rao GN. Outcome of probing for congenital nasolacrimal duct obstruction in older children. Am J Ophthalmol. 2000;130:42–8.
Cha DS, Lee H, Park MS, Lee JM, Baek SH. Clinical outcomes of initial and repeated nasolacrimal duct office-based probing for congenital nasolacrimal duct obstruction. Korean J Ophthalmol. 2010;24:261–6.
Katowitz JA, Welsh MG. Timing of initial probing and irrigation in congenital nasolacrimal duct obstruction. Ophthalmology. 1987;94:698–705.
Mannor GE, Rose GE, Frimpong-Ansah K, Ezra E. Factors affecting the success of nasolacrimal duct probing for congenital nasolacrimal duct obstruction. Am J Ophthalmol. 1999;127:616–7.
Kashkouli MB, Beigi B, Parvaresh MM, Kassaee A, Tabatabaee Z. Late and very late initial probing for congenital nasolacrimal duct obstruction: what is the cause of failure? Br J Ophthalmol. 2003;87:1151–3.
Perveen S, Sufi AR, Rashid S, Khan A. Success rate of probing for congenital nasolacrimal duct obstruction at various ages. J Ophthalmic Vis Res. 2014;9:60–9.
Kushner BJ. The management of nasolacrimal duct obstruction in children between 18 months and 4 years old. J AAPOS. 1998;2:57–60.
Medghalchi A, Mohammadi MJ, SoltaniMoghadam R, Dalili H. Results of nasolacrimal duct probing in children between 9–48 months. Acta Med Iran. 2014;52:545–51.
Al-Faky YH, Mousa A, Kalantan H, Al-Otaibi A, Alodan H, Alsuhaibani AH. A prospective, randomised comparison of probing versus bicanalicular silastic intubation for congenital nasolacrimal duct obstruction. Br J Ophthalmol. 2015;99:246–50.
Andalib D, Nabei R. Intraoperative prognostic factors for probing outcome in children with congenital nasolacrimal duct obstruction. Eur J Ophthalmol. 2013;23:329–32.
Maheshwari R. Success rate and cause of failure for late probing for congenital nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus. 2008;45:168–71.
Takahashi Y, Iwaki M, Nakamura Y, Kakizaki H. Dacryoendoscopic findings of intracanalicular punctal plug migration with or without canaliculitis. Ophthalmic Plast Reconstr Surg. 2013;29:128–30.
Sasaki T, Sounou T, Sugiyama K. Dacryoendoscopic surgery and tube insertion in patients with common canalicular obstruction and ductal stenosis as a frequent complication. Jpn J Ophthalmol. 2009;53:145–50.
Sasaki T, Nagata Y, Sugiyama K. Nasolacrimal duct obstruction classified by dacryoendoscopy and treated with inferior meatal dacryorhinotomy: part II. Inferior meatal dacryorhinotomy. Am J Ophthalmol. 2005;140:1070–4.
Theodoropoulou S, Sutherland MS, Haddow K, Blaikie A. Success rates of endoscopic-assisted probing for congenital nasolacrimal duct obstruction in children. J Laryngol Otol. 2013;127:794–8.
Kato K, Matsunaga K, Takashima Y, Kondo M. Probing of congenital nasolacrimal duct obstruction with dacryoendoscope. Clin Ophthalmol. 2014;8:977–80.
Young JD, MacEwen CJ. Managing congenital lacrimal obstruction in general practice. BMJ. 1997;315:293–6.
MacEwen CJ, Young JD. The fluorescein disappearance test (FDT): an evaluation of its use in infants. J Pediatr Ophthalmol Strabismus. 1991;28:302–5.
Weiss AH, Baran F, Kelly J. Congenital nasolacrimal duct obstruction: delineation of anatomic abnormalities with 3-dimensional reconstruction. Arch Ophthalmol. 2012;130:842–8.
Lee H, Ha S, Lee Y, Park M, Baek S. Anatomical and morphometric study of the bony nasolacrimal canal using computed tomography. Ophthalmologica. 2012;227:153–9.
Abrishami M, Bagheri A, Salour SH, Mirdehghan SA. Late probing for congenital nasolacrimal duct obstruction. J Ophthalmic Vis Res. 2009;4:102–4.
Alanon-Fernandez MA, Alanon-Fernandez FJ, Martinez-Fernandez A, del Mar Gorgora M, Calero B, Lopez-Marin I, et al. Comparative study of primary intention lacrimal probing with and without nasal endoscopy. Acta Otorrinolaringol Esp. 2014;65:297–301.
Acknowledgments
We would like to thank Editage (http://www.editage.jp) for English language editing.
Conflicts of interest
M. Fujimoto, None; K. Ogino, None; H. Matsuyama, None; C. Miyazaki, None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Fujimoto, M., Ogino, K., Matsuyama, H. et al. Success rates of dacryoendoscopy-guided probing for recalcitrant congenital nasolacrimal duct obstruction. Jpn J Ophthalmol 60, 274–279 (2016). https://doi.org/10.1007/s10384-016-0445-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-016-0445-1