Summary
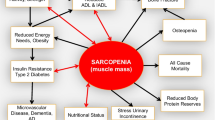
Sarcopenia is a very common, but frequently overlooked and undertreated geriatric syndrome comprising pronounced muscle mass and strength/performance loss. Estimated prevalence is between 5 and 40% in the general population, accompanied by an exponential incline with increasing age. Sarcopenia is connected to atrophy and loss of muscle fibers and motor units, affecting primarily the fast-twitch muscle fibers und their motor units. Fast-twitch muscle fibers seem to be more prone to failure of function and loss over time. Main causes for the development of sarcopenia are hormonal changes (reduced release of testosterone, estrogen, and growth hormone), nutritional deficiencies, chronic inflammation, and particularly a decrease in physical activity due to sedentary lifestyle with advancing age. Treatment options for sarcopenia comprise an active lifestyle with physical activity and exercise training, modifications of nutritional intake, and pharmacological therapies. Strength training and an adequate nutritional intake form the basis of successful sarcopenia treatment.
Zusammenfassung
Die Sarkopenie ist ein häufiges und oft übersehenes geriatrisches Syndrom mit einem verstärkten Verlust von Muskelmasse und Muskelkraft/Leistung. Die geschätzte Prävalenz liegt bei 5–40 % in der Bevölkerung – mit einem altersbezogenen exponentiellen Anstieg. Einer Sarkopenie liegen eine Atrophie und ein Verlust von Muskelfasern bzw. der motorischen Einheiten zugrunde. Sie betrifft vorrangig die schnellen Typ-II-Muskelfasern und deren motorische Einheiten. Schnelle Typ-II-Muskelfasern scheinen anfälliger für einen Funktionsverlust und einen Untergang der Muskelfasern zu sein. Wichtige Ursachen einer Sarkopenie sind hormonelle Veränderungen (abfallende Testosteron‑, Östrogen- und Wachstumshormonspiegel), Mangelernährung, chronische Entzündungsprozesse und insbesondere eine reduzierte körperliche Aktivität aufgrund eines vorwiegend bewegungsarmen Lebensstils. Behandlungsoptionen umfassen einen aktiven Lebensstil mit viel körperlicher Bewegung und sportlicher Aktivität, Anpassung der Ernährung und ggf. auch eine pharmakologische Therapie. Krafttraining und eine adäquate Ernährung stellen die Grundlage eines erfolgreichen Behandlungskonzepts einer Sarkopenie dar.





Similar content being viewed by others
References
von Haehling S, Morley JE, Anker SD. From muscle wasting to sarcopenia and myopenia: update 2012. J Cachexia Sarcopenia Muscle. 2012;3(4):213–7.
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147(8):755–63.
Ferris LT, Williams JS, Shen C‑L, O’Keefe KA, Hale KB. Resistance training improves sleep quality in older adults—a pilot study. J Sports Sci Med. 2005;4:354–60.
Surakka J. Power-type strength training in middle-aged men and women. J Sports Sci Med. 2005;4:1–35.
Palmer IJ, Runnels ED, Bemben MG, Bemben DA. Muscle-bone interactions across age in men. J Sports Sci Med. 2006;5:43–51.
Deschenes MR. Effects of aging on muscle fibre type and size. Sports Med. 2004;34(12):809–24.
Evans WJ. What is sarcopenia? J Gerontol A Biol Sci Med Sci. 1995;50:5–8.
Evans WJ, Campbell WW. Sarcopenia and age-related changes in body composition and functional capacity. J Nutr. 1993;123(Suppl 2):465–8.
Gallagher D, Ruts E, Visser M, Heshka S, Baumgartner RN, Wang J, et al. Weight stability masks sarcopenia in elderly men and women. Am J Physiol Endocrinol Metab. 2000;279(2):E366–E75.
Morrison S, Newell KM. Aging, neuromuscular decline, and the change in physiological and behavioral complexity of upper-limb movement dynamics. J Aging Res. 2012; https://doi.org/10.1155/2012/891218.
Keller K, Coldewey M, Engelhardt M. Muscle mass and strength loss with aging. Gazz Med Ital Arch Sci Med. 2014;173(9):477–83.
Keller K, Engelhardt M. Strength and muscle mass loss with aging process. Age and strength loss. Muscles Ligaments Tendons J. 2013;3(4):346–50.
McCurdy K, Langford G. The relationship between maximum unilateral squat strength and balance in young adult men and women. J Sports Sci Med. 2006;5:282–8.
Zatsiorsky VM, Kreamer WJ. Krafttraining in Praxis und Wissenschaft. Aachen: Meyer & Meyer; 2008.
Vaillancourt DE, Newell KM. Aging and the time and frequency structure of force output variability. J Appl Physiol. 2003;94(3):903–12.
Proctor DN, Balagopal P, Nair KS. Age-related sarcopenia in humans is associated with reduced synthetic rates of specific muscle proteins. J Nutr. 1998;128(2 Suppl):351S–5S.
Jones TE, Stephenson KW, King JG, Knight KR, Marshall TL, Scott WB. Sarcopenia—mechanisms and treatments. J Geriatr Phys Ther. 2009;32(2):83–9.
Doherty TJ. The influence of aging and sex on skeletal muscle mass and strength. Curr Opin Clin Nutr Metab Care. 2001;4(6):503–8.
Prochniewicz E, Thompson LV, Thomas DD. Age-related decline in actomyosin structure and function. Exp Gerontol. 2007;42(10):931–8.
Baumgartner RN, Waters DL, Gallagher D, Morley JE, Garry PJ. Predictors of skeletal muscle mass in elderly men and women. Mech Ageing Dev. 1999;107(2):123–36.
Morley JE, Baumgartner RN, Roubenoff R, Mayer J, Nair KS. Sarcopenia. J Lab Clin Med. 2001;137(4):231–43.
Lin J, Lopez EF, Jin Y, Van Remmen H, Bauch T, Han HC, et al. Age-related cardiac muscle sarcopenia: combining experimental and mathematical modeling to identify mechanisms. Exp Gerontol. 2008;43(4):296–306.
Thompson LV. Age-related muscle dysfunction. Exp Gerontol. 2009;44(1–2):106–11.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. 2010;39(4):412–23.
Bauer JM, Kaiser MJ, Sieber CC. Sarcopenia in nursing home residents. J Am Med Dir Assoc. 2008;9(8):545–51.
Doherty TJ. Invited review: aging and sarcopenia. J Appl Physiol. 2003;95(4):1717–27.
Siegrist M, Freiberger E, Geilhof B, Salb J, Hentschke C, Landendoerfer P, et al. Fall prevention in a primary care setting—the effects of a target complex exercise intervention in a cluster randomized trial. Dtsch Arztebl Int. 2016;113:365–72.
Cho SI, An DH. Effects of a fall prevention exercise program on muscle strength and balance of the old-old elderly. J Phys Ther Sci. 2014;26(11):1771–4.
Becker C, Kron M, Lindemann U, Sturm E, Eichner B, Walter-Jung B, et al. Effectiveness of a multifaceted intervention on falls in nursing home residents. J Am Geriatr Soc. 2003;51(3):306–13.
Jensen J, Lundin-Olsson L, Nyberg L, Gustafson Y. Fall and injury prevention in older people living in residential care facilities. A cluster randomized trial. Ann Intern Med. 2002;136(10):733–41.
Karamanidis K, Arampatzis A, Mademli L. Age-related deficit in dynamic stability control after forward falls is affected by muscle strength and tendon stiffness. J Electromyogr Kinesiol. 2008;18(6):980–9.
Keller K, Engelhardt M. AMI – Konsequenzen für die Rehabilitation. Man Ther. 2017;21(2):62–5.
Wall BT, Dirks ML, van Loon LJ. Skeletal muscle atrophy during short-term disuse: implications for age-related sarcopenia. Ageing Res Rev. 2013;12(4):898–906.
Lau EM, Lynn HS, Woo JW, Kwok TC, Melton LJ 3rd. Prevalence of and risk factors for sarcopenia in elderly Chinese men and women. J Gerontol A Biol Sci Med Sci. 2005;60(2):213–6.
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–56.
Muscaritoli M, Anker SD, Argiles J, Aversa Z, Bauer JM, Biolo G, et al. Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr. 2010;29(2):154–9.
Vermeulen A, Goemaere S, Kaufman JM. Testosterone, body composition and aging. J Endocrinol Invest. 1999;22(5 Suppl):110–6.
Berger MJ, Doherty TJ. Sarcopenia: prevalence, mechanisms, and functional consequences. Interdiscip Top Gerontol. 2010;37:94–114.
Bauer JM, Sieber CC. Sarcopenia and frailty: a clinician’s controversial point of view. Exp Gerontol. 2008;43(7):674–8.
Vermeulen A. Ageing, hormones, body composition, metabolic effects. World J Urol. 2002;20(1):23–7.
Klein CS, Rice CL, Marsh GD. Normalized force, activation, and coactivation in the arm muscles of young and old men. J Appl Physiol. 2001;91(3):1341–9.
Mitchell WK, Williams J, Atherton P, Larvin M, Lund J, Narici M. Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front Physiol. 2012;3:260.
Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61(10):1059–64.
Tseng LA, Delmonico MJ, Visser M, Boudreau RM, Goodpaster BH, Schwartz AV, et al. Body composition explains sex differential in physical performance among older adults. J Gerontol A Biol Sci Med Sci. 2014;69(1):93–100.
Janssen I, Baumgartner RN, Ross R, Rosenberg IH, Roubenoff R. Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. Am J Epidemiol. 2004;159(4):413–21.
Rosenberg I. Summary comments: epidemiological and methodological problems in determining nutritional status of older persons. Am J Clin Nutr. 1989;50:1231–3.
Visser M, Kritchevsky SB, Goodpaster BH, Newman AB, Nevitt M, Stamm E, et al. Leg muscle mass and composition in relation to lower extremity performance in men and women aged 70 to 79: the health, aging and body composition study. J Am Geriatr Soc. 2002;50(5):897–904.
Cesari M, Fielding RA, Pahor M, Goodpaster B, Hellerstein M, van Kan GA, et al. Biomarkers of sarcopenia in clinical trials-recommendations from the international working group on sarcopenia. J Cachexia Sarcopenia Muscle. 2012;3(3):181–90.
Delmonico MJ, Harris TB, Visser M, Park SW, Conroy MB, Velasquez-Mieyer P, et al. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr. 2009;90(6):1579–85.
Newman AB, Kupelian V, Visser M, Simonsick EM, Goodpaster BH, Kritchevsky SB, et al. Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J Gerontol A Biol Sci Med Sci. 2006;61(1):72–7.
Takamatsu Y, Koike W, Takenouchi T, Sugama S, Wei J, Waragai M, et al. Protection against neurodegenerative disease on Earth and in space. Npj Microgravity. 2016;2:16013.
Iannuzzi-Sucich M, Prestwood KM, Kenny AM. Prevalence of sarcopenia and predictors of skeletal muscle mass in healthy, older men and women. J Gerontol A Biol Sci Med Sci. 2002;57(12):M772–M7.
Kenny AM, Dawson L, Kleppinger A, Iannuzzi-Sucich M, Judge JO. Prevalence of sarcopenia and predictors of skeletal muscle mass in nonobese women who are long-term users of estrogen-replacement therapy. J Gerontol A Biol Sci Med Sci. 2003;58(5):M436–M40.
Rolland Y, Abellan van Kan G, Gillette-Guyonnet S, Vellas B. Cachexia versus sarcopenia. Curr Opin Clin Nutr Metab Care. 2011;14(1):15–21.
Collins J, Noble S, Chester J, Coles B, Byrne A. The assessment and impact of sarcopenia in lung cancer: a systematic literature review. BMJ Open. 2014;4(1):e3697.
Xue QL. The frailty syndrome: definition and natural history. Clin Geriatr Med. 2011;27(1):1–15.
Atkins JL, Whincup PH, Morris RW, Lennon LT, Papacosta O, Wannamethee SG. Sarcopenic obesity and risk of cardiovascular disease and mortality: a population-based cohort study of older men. J Am Geriatr Soc. 2014;62(2):253–60.
Prado CM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 2008;9(7):629–35.
Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997;127(5 Suppl):990S–1S.
Özkaya GY, Aydin H, Toraman FN, Kizilay F, Özdemir Ö, Cetinkaya V. Effect of strength and endurance training on cognition in older people. J Sports Sci Med. 2005;4:300–13.
Erim Z, Beg MF, Burke DT, de Luca CJ. Effects of aging on motor-unit control properties. J Neurophysiol. 1999;82(5):2081–91.
Burton LA, Sumukadas D. Optimal management of sarcopenia. Clin Interv Aging. 2010;5:217–28.
Saini A, Faulkner S, Al-Shanti N, Stewart C. Powerful signals for weak muscles. Ageing Res Rev. 2009;8(4):251–67.
Kamen G, Roy A. Motor unit synchronization in young and elderly adults. Eur J Appl Physiol. 2000;81(5):403–10.
Schwarz ER, Phan A, Willix RD Jr.. Andropause and the development of cardiovascular disease presentation-more than an epi-phenomenon. J Geriatr Cardiol. 2011;8(1):35–43.
Palacios S, Henderson VW, Siseles N, Tan D, Villaseca P. Age of menopause and impact of climacteric symptoms by geographical region. Climacteric. 2010;13(5):419–28.
Kicman AT. Pharmacology of anabolic steroids. Br J Pharmacol. 2008;154(3):502–21.
Hohmann E, Tetsworth K, Hohmann S, Bryant AL. Anabolic steroids after total knee arthroplasty. A double blinded prospective pilot study. J Orthop Surg Res. 2010;5:93.
Morley JE, Kaiser FE, Perry HM 3rd, Patrick P, Morley PM, Stauber PM, et al. Longitudinal changes in testosterone, luteinizing hormone, and follicle-stimulating hormone in healthy older men. Metab Clin Exp. 1997;46(4):410–3.
Basualto-Alarcon C, Varela D, Duran J, Maass R, Estrada M. Sarcopenia and androgens: a link between pathology and treatment. Front Endocrinol (Lausanne). 2014;5:217.
Sorensen MB, Rosenfalck AM, Hojgaard L, Ottesen B. Obesity and sarcopenia after menopause are reversed by sex hormone replacement therapy. Obes Res. 2001;9(10):622–6.
Maltais ML, Desroches J, Dionne IJ. Changes in muscle mass and strength after menopause. J Musculoskelet Neuronal Interact. 2009;9(4):186–97.
Sakuma K, Yamaguchi A. Sarcopenia and age-related endocrine function. Int J Endocrinol. 2012; https://doi.org/10.1155/2012/127362.
Kenny AM, Kleppinger A, Wang Y, Prestwood KM. Effects of ultra-low-dose estrogen therapy on muscle and physical function in older women. J Am Geriatr Soc. 2005;53(11):1973–7.
La Colla A, Pronsato L, Milanesi L, Vasconsuelo A. 17beta-estradiol and testosterone in sarcopenia: role of satellite cells. Ageing Res Rev. 2015;24(Pt B):166–77.
Urban RJ, Dillon EL, Choudhary S, Zhao Y, Horstman AM, Tilton RG, et al. Translational studies in older men using testosterone to treat sarcopenia. Trans Am Clin Climatol Assoc. 2014;125:27–42. discussion 4.
Wahlin-Larsson B, Carnac G, Kadi F. The influence of systemic inflammation on skeletal muscle in physically active elderly women. Age (dordr). 2014;36(5):9718.
Rocha R, Santana GO, Almeida N, Lyra AC. Analysis of fat and muscle mass in patients with inflammatory bowel disease during remission and active phase. Br J Nutr. 2009;101(5):676–9.
Krüger K. The increasing importance of immune regulatory effects by physical activity. Dtsch Z Sportmed. 2017;68(12):277–9.
Srikanthan P, Hevener AL, Karlamangla AS. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: findings from the National Health and Nutrition Examination Survey III. PLoS ONE. 2010;5(5):e10805.
Keller K, Engelhardt M. Muscle atrophy caused by limited mobilisation. Sportverletz Sportschaden. 2013;27(2):91–5. Muskelatrophie durch Mobilisationseinschränkung.
Kortebein P, Symons TB, Ferrando A, Paddon-Jones D, Ronsen O, Protas E, et al. Functional impact of 10 days of bed rest in healthy older adults. J Gerontol A Biol Sci Med Sci. 2008;63(10):1076–81.
Kortebein P, Ferrando A, Lombeida J, Wolfe R, Evans WJ. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA. 2007;297(16):1772–4.
Alley DE, Koster A, Mackey D, Cawthon P, Ferrucci L, Simonsick EM, et al. Hospitalization and change in body composition and strength in a population-based cohort of older persons. J Am Geriatr Soc. 2010;58(11):2085–91.
Wackerhage H. Sarcopenia: causes and treatments. Dtsch Z Sportmed. 2017;68(7–8):178–83.
Chin SO, Rhee SY, Chon S, Hwang YC, Jeong IK, Oh S, et al. Sarcopenia is independently associated with cardiovascular disease in older Korean adults: the Korea National Health and Nutrition Examination Survey (KNHANES) from 2009. PLoS ONE. 2013;8(3):e60119.
Landi F, Liperoti R, Fusco D, Mastropaolo S, Quattrociocchi D, Proia A, et al. Prevalence and risk factors of sarcopenia among nursing home older residents. J Gerontol A Biol Sci Med Sci. 2012;67(1):48–55.
Tudorache V, Oancea C, Avram C, Fira-Mladinescu O. Changes in physical activity in healthy people and COPD patients. Wien Klin Wochenschr. 2014;126(1–2):30–5.
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12(5):489–95.
Haran PH, Rivas DA, Fielding RA. Role and potential mechanisms of anabolic resistance in sarcopenia. J Cachexia Sarcopenia Muscle. 2012;3(3):157–62.
Castillo EM, Goodman-Gruen D, Kritz-Silverstein D, Morton DJ, Wingard DL, Barrett-Connor E. Sarcopenia in elderly men and women: the Rancho Bernardo study. Am J Prev Med. 2003;25(3):226–31.
Plurphanswat N, Rodu B. The association of smoking and demographic characteristics on body mass index and obesity among adults in the U.S., 1999–2012. BMC Obes. 2014;1:18.
Sneve M, Jorde R. Cross-sectional study on the relationship between body mass index and smoking, and longitudinal changes in body mass index in relation to change in smoking status: the Tromso Study. Scand J Public Health. 2008;36(4):397–407.
Landbo C, Prescott E, Lange P, Vestbo J, Almdal TP. Prognostic value of nutritional status in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;160(6):1856–61.
Morley JE, Abbatecola AM, Argiles JM, Baracos V, Bauer J, Bhasin S, et al. Sarcopenia with limited mobility: an international consensus. J Am Med Dir Assoc. 2011;12(6):403–9.
Cooper C, Fielding R, Visser M, van Loon LJ, Rolland Y, Orwoll E, et al. Tools in the assessment of sarcopenia. Calcif Tissue Int. 2013;93(3):201–10.
Lee DC, Shook RP, Drenowatz C, Blair SN. Physical activity and sarcopenic obesity: definition, assessment, prevalence and mechanism. Future Sci OA. 2016;2(3):FSO127.
Kawakami R, Murakami H, Sanada K, Tanaka N, Sawada SS, Tabata I, et al. Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women. Geriatr Gerontol Int. 2015;15(8):969–76.
Keller K, Mortier J, Freiwald J, Engelhardt M. The effect of intraarticular medications on the early rehabilitation of knee patients. Dtsch Z Sportmed. 2010;61(7–8):163–70.
Nishimura Y, Tsutsumi M, Nakata H, Tsunenari T, Maeda H, Yokoyama M. Relationship between respiratory muscle strength and lean body mass in men with COPD. Chest. 1995;107(5):1232–6.
Zarzeczny R, Nawrat-Szoltysik A, Polak A, Maliszewski J, Kieltyka A, Matyja B, et al. Aging effect on the instrumented timed-up-and-go test variables in nursing home women aged 80–93 years. Biogerontology. 2017;18(4):651–63.
Sartorio A, Lafortuna CL, Agosti F, Proietti M, Maffiuletti NA. Elderly obese women display the greatest improvement in stair climbing performance after a 3-week body mass reduction program. Int J Obes Relat Metab Disord. 2004;28(9):1097–104.
Musselman K, Brouwer B. Gender-related differences in physical performance among seniors. J Aging Phys Act. 2005;13(3):239–53.
Leyk D. The preventive and therapeutic roles of regular physical activity. Dtsch Arztebl Int. 2009;106(44):713–4.
Halle M, Schoenberg MH. Physical activity in the prevention and treatment of colorectal carcinoma. Dtsch Arztebl Int. 2009;106(44):722–7.
Reimers CD, Knapp G, Reimers AK. Exercise as stroke prophylaxis. Dtsch Arztebl Int. 2009;106(44):715–21.
Wilms B, Schmid SM, Luley K, Wiskemann J, Lehnert H. Prevention and treatment of cachexia : exercise and nutritional therapy. Internist (Berl). 2016;57(10):971–7. Pravention und Behandlung der Kachexie : Bewegungs- und Ernahrungstherapie.
Evans WJ. Skeletal muscle loss: cachexia, sarcopenia, and inactivity. Am J Clin Nutr. 2010;91(4):1123S–7S.
Roubenoff R. Sarcopenia: a major modifiable cause of frailty in the elderly. J Nutr Health Aging. 2000;4(3):140–2.
Roth SM, Ferrell RF, Hurley BF. Strength training for the prevention and treatment of sarcopenia. J Nutr Health Aging. 2000;4(3):143–55.
Mayer F, Scharhag-Rosenberger F, Carlsohn A, Cassel M, Muller S, Scharhag J. The intensity and effects of strength training in the elderly. Dtsch Arztebl Int. 2011;108(21):359–64.
Leyk D, Ruther T, Wunderlich M, Sievert A, Essfeld D, Witzki A, et al. Physical performance in middle age and old age: good news for our sedentary and aging society. Dtsch Arztebl Int. 2010;107(46):809–16.
Suetta C, Hvid LG, Justesen L, Christensen U, Neergaard K, Simonsen L, et al. Effects of aging on human skeletal muscle after immobilization and retraining. J Appl Physiol. 2009;107(4):1172–80.
Becker C, Rapp K. Falling in geriatrics. Diagnosis and treatment. Internist (Berl). 2011;52(8):939–45. Stürze in der Geriatrie. Diagnostik und Therapie.
Albert US, Kreienberg R, Schulz KD. Prävention und Brustkrebsfrüherkennung. Onkologe. 2002;8:797–807.
Guadalupe-Grau A, Perez-Gomez J, Olmedillas H, Chavarren J, Dorado C, Santana A, et al. Strength training combined with plyometric jumps in adults: sex differences in fat-bone axis adaptations. J Appl Physiol. 2009;106(4):1100–11.
Kelley G. Dynamic resistance exercise and resting blood pressure in adults: a meta-analysis. J Appl Physiol. 1997;82(5):1559–65.
Etgen T, Sander D, Bickel H, Forstl H. Mild cognitive impairment and dementia: the importance of modifiable risk factors. Dtsch Arztebl Int. 2011;108(44):743–50.
Bauer JM. Nutrition in older persons. Basis for functionality and quality of life. Internist (Berl). 2011;52(8):946–54. Ernährung im Alter. Grundlage für den Erhalt von Funktionalität und Lebensqualität.
Malafarina V, Uriz-Otano F, Iniesta R, Gil-Guerrero L. Effectiveness of nutritional supplementation on muscle mass in treatment of sarcopenia in old age: a systematic review. J Am Med Dir Assoc. 2012; https://doi.org/10.1016/j.jamda.2012.08.001.
Houston DK, Nicklas BJ, Ding J, Harris TB, Tylavsky FA, Newman AB, et al. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the health, aging, and body composition (Health ABC) study. Am J Clin Nutr. 2008;87(1):150–5.
Dreyer HC, Volpi E. Role of protein and amino acids in the pathophysiology and treatment of sarcopenia. J Am Coll Nutr. 2005;24(2):140S–5S.
Paddon-Jones D, Sheffield-Moore M, Katsanos CS, Zhang XJ, Wolfe RR. Differential stimulation of muscle protein synthesis in elderly humans following isocaloric ingestion of amino acids or whey protein. Exp Gerontol. 2006;41(2):215–9.
Katsanos CS, Kobayashi H, Sheffield-Moore M, Aarsland A, Wolfe RR. Aging is associated with diminished accretion of muscle proteins after the ingestion of a small bolus of essential amino acids. Am J Clin Nutr. 2005;82(5):1065–73.
Brotto M, Abreu EL. Sarcopenia: pharmacology of today and tomorrow. J Pharmacol Exp Ther. 2012;343(3):540–6.
Ledl-Kurkowski E, Niebauer J. Doping und seine Auswirkungen auf das vaskuläre System. J Kardiol. 2009;16(9–10):345–50.
vandenBerg P, Neumark-Sztainer D, Cafri G, Wall M. Steroid use among adolescents: longitudinal findings from Project EAT. Pediatrics. 2007;119(3):476–86.
Clasing D. Doping – verbotene Arzneimittel im Sport. Stuttgart: Gustav Fischer; 1992.
Evans NA. Current concepts in anabolic-androgenic steroids. Am J Sports Med. 2004;32(2):534–42.
Wood RI, Stanton SJ. Testosterone and sport: current perspectives. Horm Behav. 2012;61(1):147–55.
Rooks D, Praestgaard J, Hariry S, Laurent D, Petricoul O, Perry RG, et al. Treatment of sarcopenia with Bimagrumab: results from a phase II, randomized, controlled, proof-of-concept study. J Am Geriatr Soc. 2017;65(9):1988–95.
Beveridge LA, Ramage L, McMurdo ME, George J, Witham MD. Allopurinol use is associated with greater functional gains in older rehabilitation patients. Age Ageing. 2013;42(3):400–4.
Lynch JE, Henderson NR, Ramage L, McMurdo ME, Witham MD. Association between statin medication use and improved outcomes during inpatient rehabilitation in older people. Age Ageing. 2012;41(2):260–2.
Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. 2009;374(9696):1196–208.
Christensen K, Thinggaard M, McGue M, Rexbye H, Hjelmborg JV, Aviv A, et al. Perceived age as clinically useful biomarker of ageing: cohort study. BMJ. 2009;339:b5262.
Brito LB, Ricardo DR, Araujo DS, Ramos PS, Myers J, Araujo CG. Ability to sit and rise from the floor as a predictor of all-cause mortality. Eur J Prev Cardiol. 2014;21(7):892–8.
Landi F, Liperoti R, Russo A, Giovannini S, Tosato M, Capoluongo E, et al. Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr. 2012;31(5):652–8.
Landi F, Liperoti R, Fusco D, Mastropaolo S, Quattrociocchi D, Proia A, et al. Sarcopenia and mortality among older nursing home residents. J Am Med Dir Assoc. 2012;13(2):121–6.
Janssen I. Influence of sarcopenia on the development of physical disability: the cardiovascular health study. J Am Geriatr Soc. 2006;54(1):56–62.
Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002;50(5):889–96.
Cesari M, Pahor M, Lauretani F, Zamboni V, Bandinelli S, Bernabei R, et al. Skeletal muscle and mortality results from the InCHIANTI Study. J Gerontol A Biol Sci Med Sci. 2009;64(3):377–84.
Ruiz JR, Sui X, Lobelo F, Morrow JR Jr., Jackson AW, Sjostrom M, et al. Association between muscular strength and mortality in men: prospective cohort study. BMJ. 2008;337:a439.
Clark BC, Manini TM. Sarcopenia \(\neq\) dynapenia A Biol Sci Med Sci. 2008;63(8):829–34.
Di Nisio M, Di Iorio A, Porreca E, Abate M, Ferrante N, Bandinelli S, et al. Obesity, poor muscle strength, and venous thromboembolism in older persons: the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2011;66(3):320–5.
Kyrle PA, Minar E, Bialonczyk C, Hirschl M, Weltermann A, Eichinger S. The risk of recurrent venous thromboembolism in men and women. N Engl J Med. 2004;350(25):2558–63.
Oger E. Incidence of venous thromboembolism: a community-based study in Western France. EPI-GETBP Study Group. Groupe d’Etude de la Thrombose de Bretagne Occidentale. Thromb Haemost. 2000;83(5):657–60.
Silverstein MD, Heit JA, Mohr DN, Petterson TM, O’Fallon WM, Melton LJ 3rd. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 1998;158(6):585–93.
Stein PD, Hull RD, Kayali F, Ghali WA, Alshab AK, Olson RE. Venous thromboembolism according to age: the impact of an aging population. Arch Intern Med. 2004;164(20):2260–5.
Hippisley-Cox J, Coupland C. Development and validation of risk prediction algorithm (QThrombosis) to estimate future risk of venous thromboembolism: prospective cohort study. BMJ. 2011;343:d4656.
Keller K, Beule J, Coldewey M, Dippold W, Balzer JO. Impact of advanced age on the severity of normotensive pulmonary embolism. Heart Vessels. 2015;30(5):647–56.
Owen BA, Xue A, Heit JA, Owen WG. Procoagulant activity, but not number, of microparticles increases with age and in individuals after a single venous thromboembolism. Thromb Res. 2011;127(1):39–46.
Engbers MJ, van Hylckama Vlieg A, Rosendaal FR. Venous thrombosis in the elderly: incidence, risk factors and risk groups. J Thromb Haemost. 2010;8(10):2105–12.
Lavie CJ, Carbone S, Agarwal MA. An obesity paradox with myocardial infarction in the elderly. Nutrition. 2017; https://doi.org/10.1016/j.nut.2017.08.003.
Keller K, Munzel T, Ostad MA. Sex-specific differences in mortality and the obesity paradox of patients with myocardial infarction ages >70 y. Nutrition. 2017; https://doi.org/10.1016/j.nut.2017.09.004.
Roubenoff R. Sarcopenia and its implications for the elderly. Eur J Clin Nutr. 2000;54(Suppl 3):S40–S7.
Funding
This study was supported by the German Federal Ministry of Education and Research (BMBF 01EO1003 and BMBF 01EO1503). The author is responsible for the contents of this publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K. Keller declares that he has no competing interests.
Rights and permissions
About this article
Cite this article
Keller, K. Sarcopenia. Wien Med Wochenschr 169, 157–172 (2019). https://doi.org/10.1007/s10354-018-0618-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-018-0618-2