Abstract
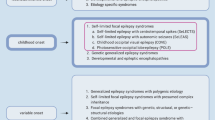
The co-occurrence of self-limited focal epilepsies of childhood (SelFEC) and epileptiform discharges in the context of SelFEC (EDSelFEC) in children with structural focal epilepsies and with brain lesions has received little attention in the literature to date, mainly in the form of case reports. The few reports on the occurrence of EDSelFEC and SelFEC in children who have undergone presurgical evaluation due to focal seizures that cannot be controlled by medication also suggests that these are relatively rare constellations. Recent publications, on the other hand, are showing that in children who have suffered pre-/perinatal complications, the incidence and prevalence of EDSelFEC and SelFEC are relatively high, especially when the white matter is damaged. The pathophysiology that leads to the generation of EDSelFEC and SelFEC, when the white matter is damaged, is not fully understood. A surprisingly high number of abnormalities is detected when magnetic resonance imaging is performed systematically on children with self-limited epilepsy with centrotemporal spikes (SelECTS). A misunderstanding of EDSelFEC and SelFEC as expressions of epileptogenic focal structural (cortical) lesions can, in individual cases, lead to a significant deterioration of epilepsy due to the administration of potentially aggravating medications, such as sodium channel blockers, and in children who have suffered pre-/perinatal complications the parents may not be informed about the relatively positive long-term prognosis of their child’s epilepsy. This article reviews recent findings on the prevalence of EDSelFEC and SelFEC in children with structural focal epilepsies and with brain lesions and their potential impact on diagnosis and treatment.
Zusammenfassung
Das gleichzeitige Auftreten von selbstlimitierenden fokalen Epilepsien des Kindesalters (SelFEK) und epileptiformen Entladungen im Kontext von SelFEK (EDSelFEK) bei Kindern mit Hirnläsionen und Kindern mit strukturellen fokalen Epilepsien hat in der medizinischen Literatur bisher nur wenig Beachtung gefunden, hauptsächlich in Form von Fallberichten. Berichte über das Auftreten von SelFEK und EDSelFEK bei Kindern, bei denen wegen fokaler epileptischer Anfälle, die nicht durch Medikamente zu kontrollieren sind, eine prächirurgische Diagnostik durchgeführt wurde, vermitteln ebenfalls den Eindruck, dass es sich eher um seltene Konstellationen handelt. Neuere Publikationen zeigen andererseits auf, dass bei Kindern, bei welchen Hirnläsionen aufgrund prä-/perinataler Komplikationen aufgetreten sind, die Inzidenz und Prävalenz von SelFEK und EDSelFEK relativ hoch ist, insbesondere dann, wenn eine Schädigung der weißen Substanz vorliegt. Die Pathophysiologie, welche zu einer vermehrten Generierung von EDSelFEK und SelFEK bei einer Schädigung der weißen Substanz führt, ist noch unklar. Eine überraschend hohe Zahl von neuroradiologischen Auffälligkeiten zeigt sich in systematischen Magnetresonanztomographie-Untersuchungen von Kindern mit selbstlimitierenden fokalen Epilepsien mit zentro-temporalen spikes (englischsprachige Abkürzung SELECTS). Das Verkennen von EDSelFEK und SelFEK als Ausdruck von strukturellen (kortikalen) Läsionen kann in Einzelfällen durch die Verabreichung von potenziell aggravierenden Medikamenten, z. B. Natrium-Kanal-Blocker, zu einer erheblichen Verschlechterung der Epilepsie führen, und bei Kindern, bei denen prä-/perinatale Komplikationen aufgetreten sind, werden die Eltern möglicherweise nicht über die eher günstige Langzeitprognose der Epilepsie ihres Kindes informiert. In der vorliegenden Arbeit werden aktuelle Ergebnisse zur Prävalenz von EDSelFEK und SelFEK bei Kindern mit strukturellen fokalen Epilepsien und Hirnläsionen sowie deren mögliche Auswirkungen auf die Diagnose und Behandlung erörtert.






Similar content being viewed by others
References
Altenmüller DM, Schulze-Bonhage A (2007) Differentiating between benign and less benign: epilepsy surgery in symptomatic frontal lobe epilepsy associated with benign focal epileptiform discharges of childhood. J Child Neurol 22(4):456–461
An O, Nagae LM, Winesett SP (2021) A self-limited childhood epilepsy as co-incidental in cerebral palsy. Int Med Case Rep J 14:509–517
Berg AT, Berkovic SF, Brodie MJ et al (2010) Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia 51(4):676–685. https://doi.org/10.1111/j.1528-1167.2010.02522
Blom S, Heijbel J, Bergfors P (1972) Benign epilepsy of children with centro-temporal EEG foci. Prevalence and follow-up study of 40 patients. Epilepsia 13(5):609–619
Boxerman JL, Hawash K, Bali B, Clarke T, Rogg J, Pal DK (2007) Is Rolandic epilepsy associated with abnormal findings on cranial MRI. Epilepsy Res 75(2–3):180–185
Brockhaus A, von Stülpnagel C, Holthausen H Benigne idiopathische fokale Sharp waves / – Epilepsien des Kindesalters bei Hirnläsionen: diagnostische, klassifikatorische und therapeutische Herausforderungen; oral presentation. 31st annual meeting of the German Pediatric Neurology Society, Erlangen, 21.–23.04.2005
Ciumas C, Saignavongs M, Ilski F, Herbillon V, Laurent A et al (2014) White matter development in children with benign childhood epilepsy with centro-temporal spikes. Brain 137(4):1095–1106
Clancy RR, Tharp BR (1984) Electroencephalogr Clin Neurophysiol 57(5):395–404. https://doi.org/10.1016/0013-4694(84)90068-3
Commission on Classification and Terminology of the International League Against Epilepsy (1989) Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia 30(4):389–399. https://doi.org/10.1111/j.1528-1157.1989.tb05316
Cooper MS, Mackay MT, Dagia C et al (2023) Epilepsy syndromes in cerebral palsy: varied, evolving and mostly self-limited. Brain 146(2):587–599
Cooper MS, Mackay MT, Fahey M et al (2017) Seizures in children with cerebral palsy and white matter injury. Pediatrics 139(3):e20162975. https://doi.org/10.1542/peds.2016-2975
Degen R, Holthausen H, Pieper T, Tuxhorn I, Wolf P (1999) Benign epileptic discharges in patients with lesional partial epilepsies. Pediatr Neurol 20(5):354–359
Gelisse P, Corda D, Raybaud C, Dravet C, Bureau M, Genton P (2003) Abnormal neuroimaging in patients with benign epilepsy with centrotemporal spikes. Epilepsia 44(3):372–378
Groeppel G, Dorfer C, Dressler A, Muehlebern A, Porsche B, Haunfellner JA, Czech T, Feucht M (2016) Immediate termination of electrical status epilepticus in sleep after hemispherotomy is associated with significant progress in language development. Dev Med Child Neurol. https://doi.org/10.1111/dmcn.13233
Holthausen H, Brockhaus A Kombinationen von symptomatisch fokalen Epilepsien/cerebralen Läsionen und benignen fokalen Epilepsien / benignen fokalen sharp waves des Kindesalters. Oral presentation; 24th Vogtareuther Epilepsie-Seminar, 23 Oct 2010
Jiang Y, Song L, Li X et al (2019) Dysfunctional white-matter networks in medicated and unmedicated benign epilepsy with centrotemporal spikes. Hum Brain Mapp 40(10):3113–3124. https://doi.org/10.1002/hbm.24584
Kelemen A (2003) Benign epilepsy of childhood with malformations of cortical development. Epilepsia 44(9):1259–1260
Kramer U, Zelnik N, Lerman-Sagie T, Shahar E (2002) Benign childhood epilepsy with centrotemporal spikes: clinical characteristics and identification of patients at risk for multiple seizures. J Child Neurol 17(1):17–19
Lerman P, Kivity S (1975) Benign focal epilepsy of childhood. A follow-up study of 100 recovered patients. Arch Neurol 32(4):261–264
Loddenkemper T, Cosmo G, Kotagal P, Haut J, Klaas P, Gupta A, Lachhwani DK, Wyllie E (2009) Epilepsy surgery in children with electrical status epilepticus in sleep. Neurosurgery 64(2):328–337. https://doi.org/10.1227/01.NEU.0000336767.14252.76 (discussion 337)
Lundberg S, Eeg-Olofsson O, Raininko R, Eeg-Olofsson K (1999) Hippocampal asymmetries and white matter abnormalities on MRI in benign childhood epilepsy with centrotemporal spikes. Epilepsia 40:1808–1815
Mambelli M, Mascano FC, Masoni P, Marchia G, Franzoni E (1985) Epilepsia rolandica. Consierazione su una casistica di 40 bambini. Boll Lega Int 51:79–80
Morikawa T, Osawa T, Ishihara O, Seino M (1979) A reappraisal of “benign epilepsy of children with centro-temporal EEG foci”. Brain Dev 1(4):257–265
Mukhin Yu K, Mironov MB, Borovikov KS, Bobylova Yu. Holthausen MH (2015) Unexpected favorable prognosis in children with focal epilepsy due to perinatal brain damage. Epilepsia 56(173):S1 (p.0707, abstr)
Okumura A, Hayakawa F, Kato T, Kuno K, Watanabe K (1999) Epilepsy in patients with spastic cerebral palsy: correlation with MRI findings at 5 years of age. Brain Dev 21(8):540–543. https://doi.org/10.1016/s0387-7604(99)00070-4
Okumura A, Hayakawa F, Kato T, Kuno K, Watanabe K (1999) Neuropediatrics 30(6):278–282. https://doi.org/10.1055/S-2007-973505
Ostrowski LM, Song DY, Thorn EL et al (2019) Dysmature superficial white matter microstructure in developmental focal epilepsy. Brain Commun 1(1):fcz2
Pan A, Gupta A, Wyllie E, Lüders H, Bingaman W (2004) Benign focal epileptiform discharges of childhood and hippocampal sclerosis. Epilepsia 45(3):284–288
Ramchandran NE, Ochi A, Benifla M, Rutka JT, Snead O, Otsubo H (2007) Benign epileptiform discharges in Rolandic Region with mesial temporal lobe epilepsy: MEG, scalp and intracranial EEG features. Acta Neurol Scand 116(1):59–64
Santanelli P, Bureau M, Magaudda A, Gobbi G, Roger J (1989) Benign partial epilepsy with centrotemporal (or rolandic) spikes and brain lesion. Epilepsia 30:182–188
Sarkis RA, Jehi LE, Bingaman WE, Najm IM (2010) Surgical outcome following resection of rolandic focal cortical dysplasia. Epilepsy Res 90(3):240–247
Sarnat HB et al (2018) Clin Neuropathol (6):262–276
Scheffer IE, Berkovic S, Capovilla G et al (2017) ILAE classification of the epilepsies: position paper of the ILAE commission for classification and terminology. Epilepsia 58(4):512–521. https://doi.org/10.1111/epi.13709
Sheth RD, Gutierrez AR, Riggs JE (1997) Rolandic epilepsy and cortical dysplasia: MRI correlation of epileptiform discharges. Pediatr Neurol 17:177–179
Specchio N, Wirrell EC, Scheffer IE, Nabbout R, Riney K, Samia P, Auvin S (2022) International league against epilepsy classification and definition of epilepsy syndromes with onset in childhood: position paper by the ILAE task force on nosology and definitions. Epilepsia. https://doi.org/10.1111/epi.17241
Stephani U, Doose H (1999) Benign idiopathic partial epilepsy and brain lesion. Epilepsia 40(3):373–376
Tarta-Arsene O, Winkler P, Pieper T, Hartlieb T, Zsoter A, Stan I, Kudernatsch M, Berweck S, Holthausen H Epileptiform discharges in the context of self-limited pediatric focal epilepsy (EDSelPFE) in pediatric hemispherotomy patients, submitted.
Vadlamudi L, Kjeldsen MJ, Corey LA, Solaas MH, Friis ML, Pellock JM, Nakken KO, Milne RL, Scheffer IE, Harvey AS, Hopper JL, Berkovic SF (2006) Analyzing the etiology of benign rolandic epilepsy: a multicenter twin collaboration. Epilepsia 47:550–555
Wang F, Zheng H, Zhang X, Li Y, Gao Z, Wang Y, Liu X, Yao Y (2016) Successful surgery in lesional epilepsy secondary to posterior quadrant ulegyria coexisting with benign childhood focal epilepsy: a case report. Clin Neurol Neurosurg 149:94–97
Wang S, Weil IGM, Fallah A, Korman B, Ragheb J, Bhatia S, Duchowny M (2020) Surgical management of pediatric patients with encephalopathy due to electrical status epilepticus during sleep (ESES). Epileptic Disord 22(1):39–54. https://doi.org/10.1684/epd.2020.1129
Wanigasinghe J, Reid SM, Mackay MT, Reddihough DS, Harvey AS, Freeman JL (2010) Epilepsy in hemiplegic cerebral palsy due to perinatal arterial ischemic stroke. Dev Med Child Neurol 52(11):1021–1027. https://doi.org/10.1111/j.1469-8749.2010.03699
Wehner T, Lachhwani DK, Bingaman W et al (2011) Epilepsy surgery outcome in coexisting symptomatic refractory focal epilepsy and benign focal epilepsy of childhood. Pediatr Neurol 44(1):52–56
Wirrell EC, Camfield PR, Camfield CS (1995) Benign Rolandic epilepsy: atypical features are very common. J Child Neurol 10:455–458
Wirrel EC, Nabbout R, Scheffer IE, Taoufik A, Bogacz A, French JA, Hirsch E et al (2022) Methodology for classification and definition of epilepsy syndromes with list of syndromes: report of the ILAE Task Force on Nosology and Definitions. Epilepsia 63:1333–1134
Xiao F, Chen Q, Yu X, Tang Y, Luo C, Fang J et al (2014) Hemispheric lateralization of microstructural white matter abnormalities in children with active benign childhood epilepsy with centro-temporal spikes (BECTS): a preliminary DTI study. J Neurol Sci 336:1
Further reading
Metsähonkala EL, Holthausen H, Ng YT, Gaily E (2017) Vascular causes and perinatal hypoxic-ischemic events. In: Pediatric epilepsy surgery. John Libbey Eurotext,
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H. Holthausen, A. Brockhaus, C. von Stülpnagel, T. Pieper, A. Zsoter, G. Kluger, S. Berweck and T. Hartlieb declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Scan QR code & read article online
Rights and permissions
About this article
Cite this article
Holthausen, H., Brockhaus, A., von Stülpnagel, C. et al. Co-existence of self-limited focal epilepsies of childhood (SelFEC) and epileptiform discharges in the context of SelFEC in children with structural focal epilepsies and in children with brain lesions. Clin Epileptol 37, 25–35 (2024). https://doi.org/10.1007/s10309-023-00653-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10309-023-00653-6