Abstract
Purpose
Neurogenic orthostatic hypotension (nOH) is a frequent nonmotor feature of Parkinson’s disease (PD), associated with adverse outcomes. Recently, 24-h ambulatory blood pressure monitoring (ABPM) showed good accuracy in diagnosing nOH. This study aims at evaluating the prognostic role of ABPM-hypotensive episodes in predicting PD disability milestones and mortality and comparing it to the well-defined prognostic role of bedside nOH.
Methods
Patients with PD who underwent ABPM from January 2012 to December 2014 were retrospectively enrolled and assessed for the development of falls, fractures, dementia, bed/wheelchair confinement, hospitalization, and mortality, during an up-to-10-year follow-up. Significant ABPM-hypotensive episodes were identified when greater than or equal to two episodes of systolic BP drop ≥ 15 mmHg (compared with the average 24 h) were recorded during the awakening-to-lunch period.
Results
A total of 99 patients (74% male, age 64.0 ± 10.1 years, and PD duration 6.4 ± 4.0 years) were enrolled. At baseline, 38.4% of patients had ABPM-hypotensive episodes and 46.5% had bedside nOH.
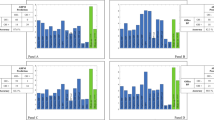
On Kaplan–Meier analysis, patients with ABPM-hypotensive episodes showed earlier onset of falls (p = 0.001), fractures (p = 0.004), hospitalizations (p = 0.009), bed/wheelchair confinement (p = 0.032), dementia (p = 0.001), and shorter survival (8.0 versus 9.5 years; p = 0.009). At Cox regression analysis (adjusted for age, disease duration, Charlson Comorbidity Index, and Hoehn and Yahr stage) a significant association was confirmed between ABPM-hypotensive episodes and falls [odds ratio (OR) 3.626; p = 0.001), hospitalizations (OR 2.016; p = 0.038), and dementia (OR 2.926; p = 0.008), while bedside nOH was only associated with falls (OR 2.022; p = 0.039) and dementia (OR 1.908; p = 0.048).
Conclusions
The presence of at least two ABPM-hypotensive episodes independently predicted the development of falls, dementia, and hospitalization, showing a stronger prognostic value than the simple bedside assessment.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, Fabrizio Vallelonga, upon reasonable request.
References
Merola A, Sawyer RP, Artusi CA et al (2018) Orthostatic hypotension in Parkinson disease: impact on health care utilization. Parkinsonism Relat Disord 47:45–49. https://doi.org/10.1016/j.parkreldis.2017.11.344
Velseboer DC, de Haan RJ, Wieling W et al (2011) Prevalence of orthostatic hypotension in Parkinson’s disease: a systematic review and meta-analysis. Parkinsonism Relat Disord 17:724–729. https://doi.org/10.1016/j.parkreldis.2011.04.016
Palma J-A, Gomez-Esteban JC, Norcliffe-Kaufmann L et al (2015) Orthostatic hypotension in Parkinson disease: how much you fall or how low you go? Mov Disord 30:639–645. https://doi.org/10.1002/mds.26079
Ricci F, Fedorowski A, Radico F et al (2015) Cardiovascular morbidity and mortality related to orthostatic hypotension: a meta-analysis of prospective observational studies. Eur Heart J 36:1609–1617. https://doi.org/10.1093/eurheartj/ehv093
Romagnolo A, Zibetti M, Merola A et al (2019) Cardiovascular autonomic neuropathy and falls in Parkinson disease: a prospective cohort study. J Neurol 266:85–91. https://doi.org/10.1007/s00415-018-9104-4
Longardner K, Merola A, Litvan I et al (2022) Differential impact of individual autonomic domains on clinical outcomes in Parkinson’s disease. J Neurol 269:5510–5520. https://doi.org/10.1007/s00415-022-11221-9
Pilotto A, Romagnolo A, Scalvini A et al (2021) Association of orthostatic hypotension with cerebral atrophy in patients with Lewy body disorders. Neurology 97:e814–e824. https://doi.org/10.1212/WNL.0000000000012342
McDonald C, Newton JL, Burn DJ (2016) Orthostatic hypotension and cognitive impairment in Parkinson’s disease: causation or association? Mov Disord 31:937–946. https://doi.org/10.1002/mds.26632
Udow SJ, Robertson AD, MacIntosh BJ et al (2016) “Under pressure”: is there a link between orthostatic hypotension and cognitive impairment in α-synucleinopathies? J Neurol Neurosurg Psychiatry 87:1311–1321. https://doi.org/10.1136/jnnp-2016-314123
Freeman R, Wieling W, Axelrod FB et al (2011) Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res Off J Clin Auton Res Soc 21:69–72. https://doi.org/10.1007/s10286-011-0119-5
Wieling W, Kaufmann H, Claydon VE et al (2022) Diagnosis and treatment of orthostatic hypotension. Lancet Neurol 21:735–746. https://doi.org/10.1016/S1474-4422(22)00169-7
Norcliffe-Kaufmann L, Kaufmann H (2014) Is ambulatory blood pressure monitoring useful in patients with chronic autonomic failure? Clin Auton Res Off J Clin Auton Res Soc 24:189–192. https://doi.org/10.1007/s10286-014-0229-y
Belmin J, Abderrhamane M, Medjahed S et al (2000) Variability of blood pressure response to orthostatism and reproducibility of the diagnosis of orthostatic hypotension in elderly subjects. J Gerontol A Biol Sci Med Sci 55:M667–M671. https://doi.org/10.1093/gerona/55.11.m667
Vara-González L, Arauzo Alonso S, González Fernández RM et al (2006) Reproducibility of postural changes of blood pressure in hypertensive elderly patients in primary care. Blood Press Monit 11:17–20. https://doi.org/10.1097/01.mbp.0000189786.59994.fb
Ward C, Kenny RA (1996) Reproducibility of orthostatic hypotension in symptomatic elderly. Am J Med 100:418–422. https://doi.org/10.1016/S0002-9343(97)89517-4
Parati G, Stergiou G, O’Brien E et al (2014) European society of hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens 32:1359–1366. https://doi.org/10.1097/HJH.0000000000000221
Milazzo V, Di Stefano C, Vallelonga F et al (2018) Reverse blood pressure dipping as marker of dysautonomia in Parkinson disease. Park Relat Disord 56:82–87. https://doi.org/10.1016/j.parkreldis.2018.06.032
Vallelonga F, Sobrero G, Giudici M et al (2021) Screening indexes for cardiovascular autonomic failure in Parkinson’s disease. J Neurol Sci 428:117571. https://doi.org/10.1016/j.jns.2021.117571
Vallelonga F, Romagnolo A, Merola A et al (2019) Detection of orthostatic hypotension with ambulatory blood pressure monitoring in parkinson’s disease. Hypertens Res 42:1552–1560. https://doi.org/10.1038/s41440-019-0267-x
Juraschek SP, Taylor AA, Wright JTJ et al (2020) Orthostatic hypotension, cardiovascular outcomes, and adverse events: results from SPRINT. Hypertens (Dallas, Tex 1979) 75:660–667. https://doi.org/10.1161/HYPERTENSIONAHA.119.14309
Gibb WRG (1988) Accuracy in the clinical diagnosis of parkinsonian syndromes. Postgrad Med J 64:345–351. https://doi.org/10.1136/PGMJ.64.751.345
Dineen J, Freeman R (2015) Autonomic neuropathy. Semin Neurol 35:458–468. https://doi.org/10.1055/s-0035-1558983
Jankovic J, McDermott M, Carter J et al (1990) Variable expression of Parkinson’s disease: a base-line analysis of the DATATOP cohort. The Parkinson Study. Group Neurol 40:1529–1534. https://doi.org/10.1212/wnl.40.10.1529
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Kaufmann H, Malamut R, Norcliffe-Kaufmann L et al (2012) The Orthostatic Hypotension Questionnaire (OHQ): validation of a novel symptom assessment scale. Clin Auton Res Off J Clin Auton Res Soc 22:79–90. https://doi.org/10.1007/s10286-011-0146-2
Norcliffe-Kaufmann L, Kaufmann H, Palma JA et al (2018) Orthostatic heart rate changes in patients with autonomic failure caused by neurodegenerative synucleinopathies. Ann Neurol 83:522–531. https://doi.org/10.1002/ana.25170
Jansen RW, Lipsitz LA (1995) Postprandial hypotension: epidemiology, pathophysiology, and clinical management. Ann Intern Med 122:286–295. https://doi.org/10.7326/0003-4819-122-4-199502150-00009
Dalrymple-Alford JC, MacAskill MR, Nakas CT et al (2010) The MoCA: well-suited screen for cognitive impairment in Parkinson disease. Neurology 75:1717–1725. https://doi.org/10.1212/WNL.0b013e3181fc29c9
(2013) Diagnostic and statistical manual of mental disorders: DSM-5TM, 5th edn. American Psychiatric Publishing, Inc., Arlington
Ganz DA, Latham NK (2020) Prevention of falls in community-dwelling older adults. N Engl J Med 382:734–743. https://doi.org/10.1056/NEJMcp1903252
Vallelonga F, Maule S (2019) Diagnostic and therapeutical management of supine hypertension in autonomic failure: a review of the literature. J Hypertens 37:1102–1111. https://doi.org/10.1097/HJH.0000000000002008
Merola A, Romagnolo A, Rosso M et al (2016) Orthostatic hypotension in Parkinson’s disease: does it matter if asymptomatic? Parkinsonism Relat Disord 33:65–71. https://doi.org/10.1016/j.parkreldis.2016.09.013
Cremer A, Soumaré A, Berr C et al (2017) Orthostatic hypotension and risk of incident dementia: results from a 12-year follow-up of the three-city study cohort. Hypertens (Dallas, Tex 1979) 70:44–49. https://doi.org/10.1161/HYPERTENSIONAHA.117.09048
Min M, Shi T, Sun C et al (2018) The association between orthostatic hypotension and dementia: a meta-analysis of prospective cohort studies. Int J Geriatr Psychiatry 33:1541–1547. https://doi.org/10.1002/gps.4964
Allan LM, Ballard CG, Allen J et al (2007) Autonomic dysfunction in dementia. J Neurol Neurosurg Psychiatry 78:671–677. https://doi.org/10.1136/jnnp.2006.102343
Robertson AD, Udow SJ, Espay AJ et al (2019) Orthostatic hypotension and dementia incidence: links and implications. Neuropsychiatr Dis Treat 15:2181–2194. https://doi.org/10.2147/NDT.S182123
Pilotto A, Romagnolo A, Tuazon JA et al (2019) Orthostatic hypotension and REM sleep behaviour disorder: impact on clinical outcomes in α-synucleinopathies. J Neurol Neurosurg Psychiatry 90:1257–1263. https://doi.org/10.1136/jnnp-2019-320846
Fereshtehnejad S-M, Romenets SR, Anang JBM et al (2015) New clinical subtypes of Parkinson disease and their longitudinal progression: a prospective cohort comparison with other phenotypes. JAMA Neurol 72:863–873. https://doi.org/10.1001/jamaneurol.2015.0703
Robertson AD, Messner MA, Shirzadi Z et al (2016) Orthostatic hypotension, cerebral hypoperfusion, and visuospatial deficits in Lewy body disorders. Parkinsonism Relat Disord 22:80–86. https://doi.org/10.1016/j.parkreldis.2015.11.019
Palma JA, Redel-Traub G, Porciuncula A et al (2020) The impact of supine hypertension on target organ damage and survival in patients with synucleinopathies and neurogenic orthostatic hypotension. Park Relat Disord 75:97–104. https://doi.org/10.1016/j.parkreldis.2020.04.011
Chen H, Xu E, Zhou F et al (2022) Impaired dynamic cerebral autoregulation: a potential mechanism of orthostatic hypotension and dementia in Parkinson’s disease. Front Aging Neurosci 14:927009. https://doi.org/10.3389/fnagi.2022.927009
Barrio IR, Miki Y, Jaunmuktane ZT et al (2022) Association between orthostatic hypotension and dementia in patients with Parkinson disease and multiple system atrophy. Neurology. https://doi.org/10.1212/WNL.0000000000201659
Asmuje NF, Mat S, Myint PK, Tan MP (2022) Blood pressure variability and cognitive function: a scoping review. Curr Hypertens Rep 24:375–383. https://doi.org/10.1007/s11906-022-01200-w
Shibao C, Grijalva CG, Raj SR et al (2007) Orthostatic hypotension-related hospitalizations in the United States. Am J Med 120:975–980. https://doi.org/10.1016/j.amjmed.2007.05.009
Grijalva CG, Biaggioni I, Griffin MR, Shibao CA (2017) Fludrocortisone is associated with a higher risk of all-cause hospitalizations compared with midodrine in patients with orthostatic hypotension. J Am Heart Assoc. https://doi.org/10.1161/JAHA.117.006848
Feldstein C, Weder AB (2012) Orthostatic hypotension: a common, serious and underrecognized problem in hospitalized patients. J Am Soc Hypertens 6:27–39. https://doi.org/10.1016/j.jash.2011.08.008
Finucane C, O’Connell MDL, Donoghue O et al (2017) Impaired orthostatic blood pressure recovery is associated with unexplained and injurious falls. J Am Geriatr Soc 65:474–482. https://doi.org/10.1111/jgs.14563
Nakamura T, Suzuki M, Ueda M et al (2020) Impact of orthostatic hypotension on wheelchair use in patients with Parkinson’s disease. J Neural Transm 127:379–383. https://doi.org/10.1007/s00702-019-02127-4
Koo HY, Bin CE, Kong SH et al (2023) Fracture risk in Parkinson’s disease according to its severity and duration. Osteoporos Int J Establ Result Coop Between Eur Found Osteoporos Natl Osteoporos Found USA 34:81–89. https://doi.org/10.1007/s00198-022-06562-0
De Pablo-Fernández E, Lees AJ, Holton JL, Warner TT (2019) Prognosis and neuropathologic correlation of clinical subtypes of Parkinson disease. JAMA Neurol 76:470–479. https://doi.org/10.1001/jamaneurol.2018.4377
Zhang L, Hou Y, Gu X et al (2023) Prediction of early-wheelchair dependence in multiple system atrophy based on machine learning algorithm: a prospective cohort study. Clin Park Relat Disord 8:100183. https://doi.org/10.1016/j.prdoa.2023.100183
De Pablo-Fernandez E, Tur C, Revesz T et al (2017) Association of autonomic dysfunction with disease progression and survival in Parkinson disease. JAMA Neurol 74:970–976. https://doi.org/10.1001/jamaneurol.2017.1125
Goldstein DS, Holmes C, Sharabi Y, Wu T (2015) Survival in synucleinopathies: a prospective cohort study. Neurology 85:1554–1561. https://doi.org/10.1212/WNL.0000000000002086
Funding
None.
Author information
Authors and Affiliations
Contributions
(1) Research project: A. Conception: F.Va., S.M., and A.R., B. Organization: F.Va., M.V., S.M., A.R., F.Ve., and L.L., C. Execution: M.V., M.M.T., A.C., G.S., V.M., C.D., and M.G. (2) Statistical analysis: A. Design: F.Va., A.R., and A.M., B. Execution: F.Va. and A.R., C. Review and critique: all authors. (3) Manuscript: A. Writing of the first draft: F.Va., M.V. and A.R. B. Review and critique: all authors.
Corresponding author
Ethics declarations
Conflict of interest
F.Va., M.V., M.M.T., A.C., V.M., C.D., G.S., M.G., F.Ve., L.L., and S.M. report no conflict of interest. AR received grant support and speaker honoraria from Abbvie, speaker honoraria from Chiesi Farmaceutici, and travel grants from Lusofarmaco, ChiesiFarmaceutici, Medtronic, and UCB Pharma. A.M. received supported from the NIH (KL2 TR001426), speaker honoraria from CSL Behring, Abbvie, Abbott, Theravance, and Cynapsus Therapeutics; he also received grant support from Lundbeck and Abbvie.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vallelonga, F., Valente, M., Tangari, M.M. et al. Hypotensive episodes at 24-h ambulatory blood pressure monitoring predict adverse outcomes in Parkinson’s disease. Clin Auton Res 34, 281–291 (2024). https://doi.org/10.1007/s10286-024-01030-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-024-01030-7