Abstract
Purpose
Arterial stiffness is independently associated with orthostatic hypotension in older individuals. The relationship between orthostatic blood pressure adaptation and aortic stiffness has not been thoroughly examined in a younger population. We investigated the relationship between orthostatic blood pressure adaptations, central aortic hemodynamics, and aortic stiffness in a cohort of predominantly younger and middle-aged adults.
Methods
We analyzed an observational, population-based study of 5259 individuals living in Malmö, Sweden. We related aortic stiffness and central hemodynamics assessed by carotid–femoral pulse wave velocity and pulse wave analysis at the arteria radialis using Sphygmocor to orthostatic blood pressure adaptation after 3 min standing.
Results
The mean age of the population was 41.9 ± 14.5 years, and 52.1% were women. We observed the highest aortic stiffness and central aortic blood pressure measurements in the lowest and highest quartiles of orthostatic systolic blood pressure differences (p < 0.001). Aortic stiffness and central aortic blood pressure gradually decreased across increasing quartiles of orthostatic diastolic blood pressure difference (p < 0.001). After full adjustment, orthostatic diastolic blood pressure remained significantly associated with aortic stiffness (p = 0.001) and central aortic blood pressure (p < 0.001), whereas orthostatic systolic blood pressure was significantly associated only with central aortic systolic blood pressure (p = 0.009). No significant associations were found between subclinical orthostatic hypotension, aortic stiffness, and central hemodynamics.
Conclusions
Our findings demonstrate that altered blood pressure responses to orthostatic challenges, both blood pressure reductions and blood pressure increases, are independently and inversely associated with markers of aortic stiffness (vascular aging) in a predominantly young to middle-aged population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Standing up imposes a major hemodynamic burden such that abnormalities in autonomic cardiovascular control or in cardiovascular structure may be unmasked. Therefore, orthostatic testing in addition to diagnosing autonomic cardiovascular impairments provides information regarding cardiovascular risk. Indeed, orthostatic hypotension (OH) defined as a decrease in brachial systolic blood pressure (SBP) of ≥ 20 mmHg and/or a decrease in diastolic blood pressure (DBP) of 10 mmHg or more within 3 min upon standing [1], independently predicts falls, mortality, and cardiovascular diseases in older adults [2,3,4]. Moreover, abnormalities in orthostatic blood pressure regulation including abnormal SBP decrease ≥ 20 mmHg [5] or increase ≥ 20 mmHg [6] upon standing, a so-called orthostatic hypertension, as well as abnormal BP variability [7] may be associated with cardiovascular disease and death. However, considerably fewer data exist regarding potential cardiovascular risks associated with subclinical orthostatic BP abnormalities, which are more common than full-blown orthostatic hypo- or hypertension, especially in younger persons.
Even in large-scale epidemiological studies, extremely long follow-up periods would be required to show an association between putative cardiovascular risk factors and morbidity and mortality in younger persons. Aortic stiffness mirrors structural changes in the aortic wall and adjacent large arteries and is, therefore, an established vascular aging marker in the setting of epidemiological studies and in the clinic [8,9,10,11]. Noninvasive measurement of carotid–femoral pulse wave velocity (c-f PWV) allows direct quantification of aortic stiffness and is considered the gold-standard method [11]. Aortic augmentation index (AIx) is based on pulse-wave reflection to the heart, and is an indirect measure of aortic stiffness [12]. Both c-f PWV and OH predict future cardiovascular events in middle-aged and older subjects [3, 13]. However, considerably fewer data are available on the potential relationships between subtle abnormalities in BP homeostasis and early markers of vascular aging in younger subjects.
In a Swedish population-based cohort, we tested the hypothesis that orthostatic BP responses are associated with vascular aging markers in younger to middle-aged persons.
Methods
Study population and design
The Malmö Offspring Study (MOS) is a population-based study consisting of children and grandchildren to the index participants in the well-established Malmö Diet and Cancer Study (MDCS) launched in the early 1990s with over 20 years of follow-up [14]. The data collection within MOS started in 2013 and was completed by the end of 2021. To ensure that participants in the different generations were directly related, a national taxation authority register in Sweden (NAVET) was used. A total of 5259 individuals were included in MOS. Of these, 3966 individuals had complete recordings of measurements of orthostatic BP reactions, aortic stiffness, and central hemodynamics, and were thus included in the final study population.
Outcome measures
The primary outcome was increased aortic stiffness (c-f PWV) in relation to orthostatic BP differences. Secondary outcomes included increased aortic stiffness and BP reaction on standing in relation to sex and increasing age, respectively.
Assessment of blood pressure, vascular aging, and aortic stiffness
Supine systolic (SBP) and diastolic blood pressure (DBP) were reported after 5 min rest as the mean of two readings, using an automatic device (Omron M5-1 IntelliSense, the Netherlands). Subjects were thereafter asked to stand up, and the mean SBP and DBP of two consecutive readings performed after 3 min of standing was reported as the orthostatic blood pressure. Aortic stiffness was directly assessed noninvasively after 5 min of supine rest using the gold-standard measurement of c-f PWV by Sphygmocor (AtCor, Australia) [15]. The distance from the carotid to femoral artery was measured directly between each artery and the suprasternal notch. PWV was calculated by measuring the time delay between two characteristic timepoints on two pressure waveforms at a known distance apart. The SphygmoCor method uses the foot of the waveform as an onset point for calculating the time differences between the R wave of the electrocardiogram and the pulse waveforms at each site. PWV was automatically generated as the carotid–femoral artery distance divided by the wave traveling time between the above two sites.
Aortic augmentation index (AIx), an indirect measurement of aortic stiffness, was together with variables reflecting central aortic hemodynamics (central aortic SBP and central aortic DBP) acquired by radial applanation tonometry using PWA Sphygmocor (AtCor, Australia). SphygmoCor also measures and calculates the AIX standardized to a heart rate of 75 beats per minute (AIx@75), by adjusting the AIX by −4.8 for each 10 bpm above and +4.8 for each 10 bpm below a resting heart rate of 75 bpm.
Brachial SBP and DBP were used to calibrate the radial and aortic pressure waveform. This technology has good reproducibility under major hemodynamic changes, analyzing a central (ascending aortic) pressure waveform from the radial pressure waveform using a validated generalized transfer function [16].
Definition of variables and clinical characteristics
Data on prevalent diseases at baseline were collected from The Swedish National Patient Register. “Orthostatic BP difference” (mmHg) was defined as [standing BP − supine BP], i.e., a positive value denotes an increase in BP upon standing. Antihypertensive treatment at baseline was defined as self-reported intake of antihypertensive drugs. Estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI Creatinine Equation [17]. Current smoking (defined as regular or occasional smoking) and educational level were self-reported in the questionnaire.
Ethical approval
The MOS study was approved by the Regional Ethics Committee at Lund University (Dnr. 2012/594). All participants provided written informed consent.
Statistical analyses
Continuous data (of which all were normally distributed) are shown as mean ± standard deviation, whereas frequencies are used to describe categorical data. We first assessed aortic stiffness and central hemodynamic measurements by quartiles of orthostatic BP differences using one-way analysis of variance (ANOVA). Then, a linear regression model was constructed to assess the association of standing BP differences and subclinical orthostatic hypotension with aortic stiffness and central hemodynamics after different adjustments. The basic model was adjusted for age and sex. The multivariable model was adjusted for age, sex, body mass index (BMI), current smoking, fasting glucose, eGFR, antihypertensive medication, and supine SBP/DBP, as appropriate. Orthostatic diastolic BP reaction and aortic stiffness displayed a linear relationship, and was additionally adjusted for supine diastolic BP. In contrast, orthostatic systolic BP reaction displayed a U-shaped association with the outcome variables and was entered as mean-centered orthostatic systolic BP and adjusted for mean-centered supine systolic BP in addition to remaining covariates. For the secondary outcomes, analyses were performed separately according to sex and median age 44 years, respectively.
All statistical analyses were performed in IBM SPSS Statistics 27 (IBM Corporation, Armonk, NY, USA).
Results
Clinical characteristics of the study population are presented in Table 1. The mean age was 42.1 ± 14.4 years (median 44 years, range 18–73 years), and 51.8% were women. A total of 14.2% reported current smoking, and less than 5% were diagnosed with prevalent hypertension and reported intake of antihypertensive medications. Following orthostatic blood pressure measurements, 1.3% fulfilled the diagnostic criteria of OH and 1.7% showed an orthostatic SPB increase of ≥ 20 mmHg, which is commonly used as diagnostic cutoff value for orthostatic hypertension [6].
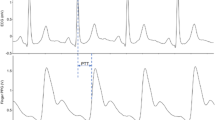
The mean orthostatic SBP difference upon standing was 1.3 ± 8.6 mmHg, whereas the corresponding orthostatic DBP difference was 9.5 ± 6.1 mmHg. Orthostatic blood pressure reactions were all normally distributed (Fig. 1). Mean aortic stiffness measurements are provided in Table 1.
Association between aortic stiffness, central hemodynamics, and orthostatic BP reactions
We observed a U-shaped association between orthostatic systolic BP differences, aortic stiffness, and central hemodynamics, i.e., subjects in the lowest and highest quartiles of orthostatic systolic BP differences demonstrated the highest degree of aortic stiffness and central aortic BP (all p < 0.001 in ANOVA; Fig. 2, Supplementary Fig. S1, Table 2). In contrast, orthostatic diastolic BP reaction displayed a linear association, with a gradual reduction in aortic stiffness and central aortic BP across all four quartiles of increasing orthostatic diastolic BP reaction (all p < 0.001 in ANOVA; Fig. 3, Supplementary Fig. S2, Table 2). No difference was observed in the sensitivity analysis after exclusion of subjects ≥ 60 years old (n = 372, 9.4%) (Supplementary Table S1).
Aortic stiffness measured by pulse wave velocity stratified according to quartiles of orthostatic systolic blood pressure reaction. Boxplot illustrating aortic stiffness stratified according to quartiles of orthostatic systolic blood pressure reaction in the general population with reported ANOVA p value
Aortic stiffness measured by pulse wave velocity stratified according to quartiles of orthostatic diastolic blood pressure reaction. Boxplot illustrating aortic stiffness stratified according to quartiles of orthostatic systolic blood pressure reaction in the general population with reported ANOVA p value
After full adjustments, orthostatic diastolic BP remained significantly associated with aortic stiffness (c-f PWV p = 0.001, Aix p = 0.005, and Aix@75 p = 0.007) and central aortic BP (p < 0.001), whereas orthostatic systolic BP was significantly associated only with indirect aortic stiffness adjusted for HR (Aix@75 p = 0.04) and central aortic systolic BP (p = 0.009) (data not shown). No significant associations were found between subclinical manifest orthostatic hypotension, aortic stiffness, and central hemodynamics (Supplementary Table S2).
Subgroup analysis stratified by age and sex
We performed fully adjusted subgroup analysis of aortic stiffness and central hemodynamics stratified by median age (Table 3). Overall, orthostatic diastolic BP was inversely associated with indirect aortic stiffness (AIX@75) (p = 0.003 and p < 0.001, Table 3), and central aortic systolic as well as diastolic BP in both age groups (p < 0.001). Orthostatic systolic BP was associated only with indirect aortic stiffness in older individuals (Aix p = 0.008, Aix@75 p = 0.008), whereas it was inversely associated with central aortic systolic BP in both age groups (p = 0.008 versus p = 0.049). Manifest subclinical OH was associated with central aortic systolic BP in the above-median-age group only.
Following sex stratification, orthostatic diastolic BP was inversely associated with direct aortic stiffness (c-f PWV p = 0.03 versus p = 0.006, Table 4), and central aortic systolic and diastolic BP (all p < 0.001) in both sexes. Only women displayed an inverse association between aortic stiffness and orthostatic diastolic BP (AIx p = 0.03 and p = 0.04), and a positive association between orthostatic hypotension and central aortic systolic BP (p = 0.02). Likewise, central aortic systolic and diastolic BP was significantly associated only with orthostatic systolic BP in women (all p = 0.02).
Discussion
In this population-based study of predominantly young to middle-aged subjects, we assessed the relationship between orthostatic BP adaptations and aortic stiffness as well as central aortic BP. We found that a more pronounced (higher) diastolic BP increase upon standing is associated with lower aortic stiffness (c-f PWV), whereas the systolic blood pressure reaction upon standing displayed a U-shaped association with aortic stiffness (c-f PWV).
To date, manifest orthostatic hypotension (OH) has been widely examined in older populations, and the prevalence of OH in the general population increases with age and comorbidities such as neurodegenerative, cardiovascular, metabolic, and renal disorders [18, 19]. Considerably fewer data exist for OH as well as the potential risks of subclinical blood pressure abnormalities in younger subjects.
In the current observational study, we provide evidence supporting the view that even subtle abnormalities in blood pressure reactions upon standing are associated with markers of increased vascular aging (arterial stiffness) in an otherwise predominantly young and healthy population.
Results compared with previous studies
A distinct increase in diastolic BP of approximately 10 mmHg upon standing is considered the normal reaction [20], and accordingly we observed that persons with a diastolic BP increase on standing of ≥ 14 mmHg had the lowest aortic stiffness. This is in line with previous data from the Framingham Heart Study Third Generation cohort, even though mean arterial pressure (MAP) was used in that study [8]. For the systolic BP increase upon standing, an U-shaped association with aortic stiffness was noted, which is in line with data suggesting that both marked systolic blood pressure decrease [5] and increase [6] upon standing is associated with adverse cardiovascular outcomes [21].
Aortic stiffness is an important risk factor/marker for cardiovascular disease (CVD) and a key element in the pathogenesis of CVD. Growing evidence shows that increased aortic stiffness can predict both cardiovascular mortality and all-cause mortality [22, 23].
An epidemiological study such as ours cannot prove causality but may generate hypotheses for mechanism-oriented investigations. While we cannot discern whether altered orthostatic blood pressure control promoted vascular damage or vice versa, our study provides an impetus to investigate mutual interactions between cardiovascular autonomic control and vascular structure in more detail. For example, baroreflex counter-regulation, which stabilizes blood pressure upon standing, could be impeded by changes in vascular structure. In a previous study, we found that proteins associated with atherosclerosis were also related to impaired blood pressure control [19, 24]. Diminished baroreflexes often occur in patients with arterial stiffness due to impaired stretch of the baroreceptors and reduced neural input to the brain stem’s autonomic control centers, causing decreased output to the cardiovascular system. Another study demonstrated that asymptomatic subjects with subclinical coronary atherosclerosis display severely blunted baroreflexes and may also have advanced coronary atherosclerosis [25]. Conversely, blood pressure swings elicited through poor cardiovascular autonomic control could negatively affect vascular structure [7].
The current study, Malmö Offspring Study, is unique since it contains a wealth of data on younger and rather healthy individuals (mean age of 41 years) with few comorbidities. For example, the hypertension prevalence (based on use of antihypertensive drugs) was only 5%. In addition, this is the first population-based cohort to investigate the association of orthostatic BP reactions with well-established and validated assessments of aortic stiffness and central hemodynamics, including the gold-standard method c-f PWV, as well as central aortic hemodynamic measurements such as AIX and central aortic BP [26,27,28]. Previous studies have only assessed aortic stiffness by c-f PWV in this context [8, 21, 29,30,31] or brachial-to-ankle PWV [32]. Moreover, the abovementioned studies have focused on older individuals (mean age ranging from 44 to 80 years) with higher prevalence of established comorbidities such as type 2 diabetes or hypertension, ranging between 20% and 60%.
Strengths and limitations of the study
To our knowledge, this is the first and largest observational study investigating the association between orthostatic blood pressure reactions and markers of aortic stiffness in nearly 4000 individuals with a mean age of 41 years. The Malmö Offspring (MOS) cohort was recently completed at the end of December 2021, providing unique data on study participants from national Swedish registers with complete coverage of public healthcare in Sweden, making our findings reliable and robust. Moreover, we assessed aortic stiffness by robust and validated methods with over 1000 peer-reviewed studies published reporting data derived from the well-validated tonometry-based SphygmoCor devices [33]. Our findings provide additional knowledge related to the potential importance of evaluating orthostatic BP adaptations at an early adult age in terms of risk assessment and in relation to markers of vascular aging. Future investigations in MOS will enable us to assess novel aspects of vascular aging, with the unique possibility of national register-based follow-up for morbidity and mortality.
However, our study has also some important limitations that need to be addressed. Study participants were predominantly young- to middle-aged individuals of white European ancestry, and therefore, the results of this study may not be generalizable to other racial/ethnic groups. Likewise, information on BP levels was obtained at a single visit, meaning that we were not able to assess the day-to-day reproducibility of our measurements. Furthermore, we could not draw any conclusions on causality from the cross-sectional design of the study, i.e., whether increased aortic stiffness leads to abnormal orthostatic BP reactions or vice versa, or if there is a common cause contributing to both aortic stiffness and abnormal orthostatic blood pressure reactions, for example, the influence of genetics or early life programming [34]. Since the MOS cohort was recently completed (end of 2021), we currently lack longitudinal data to perform prospective analyses.
Study relevance and clinical implications
The co-existence of orthostatic hypotension, increased BP variability, and arterial stiffness represents a hemodynamic aging syndrome [10] with important prognostic implications for public health. These three entities are independent risk markers for CVD, and their confluence, therefore, is of impactful significance. In addition, increasing data indicate that also orthostatic hypertension confers an increased risk of CVD [6].
We demonstrate here that even subtle, subclinical abnormalities in orthostatic BP regulation are associated with changes in central hemodynamics and arterial stiffness—a marker of early vascular aging (EVA) [35]—in a population-based cohort of predominantly young adult and middle-aged healthy subjects, whereas the prevalence of subclinical OH was low. Only individuals above the median age of 44 years showed a positive correlation between a subclinical OH diagnosis and worsened central aortic hemodynamics, i.e., aortic stiffness, in the fully adjusted model, suggesting that clinical OH is likely a marker of more advanced vascular aging [30].
Conclusions
Our findings support the hypothesis that impaired hemodynamic response to standing, traditionally observed in older individuals, is also associated with markers of vascular aging in a predominantly younger and healthy population. Further studies should assess the relationship between impaired blood pressure adaptations on standing in younger subjects and risk of future incident cardiovascular events. The clinical implication is that, in addition to diagnosing abnormalities in cardiovascular autonomic control, orthostatic testing may identify individuals at increased cardiovascular risk for preventive risk factor control.
Data availability
Anonymized data are available upon reasonable request to the corresponding author. Details on procedures can be found here: https://www.malmo-kohorter.lu.se/malmo-cohorts.
References
Brignole M, Moya A, de Lange FJ, Deharo JC, Elliott PM, Fanciulli A, Fedorowski A, Furlan R, Kenny RA, Martin A et al (2018) 2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J 39(21):1883–1948
Johansson M, Rogmark C, Sutton R, Fedorowski A, Hamrefors V (2021) Risk of incident fractures in individuals hospitalised due to unexplained syncope and orthostatic hypotension. BMC Med 19(1):188
Fedorowski A, Stavenow L, Hedblad B, Berglund G, Nilsson PM, Melander O (2010) Orthostatic hypotension predicts all-cause mortality and coronary events in middle-aged individuals (The Malmo Preventive Project). Eur Heart J 31(1):85–91
Cooper LL, Himali JJ, Torjesen A, Tsao CW, Beiser A, Hamburg NM, DeCarli C, Vasan RS, Seshadri S, Pase MP et al (2017) Inter-relations of orthostatic blood pressure change, aortic stiffness, and brain structure and function in young adults. J Am Heart Assoc 6(8):e006206
Fedorowski A, Hedblad B, Melander O (2011) Early postural blood pressure response and cause-specific mortality among middle-aged adults. Eur J Epidemiol 26(7):537–546
Jordan J, Ricci F, Hoffmann F, Hamrefors V, Fedorowski A (2020) Orthostatic hypertension: critical appraisal of an overlooked condition. Hypertension 75(5):1151–1158
Mehlum MH, Liestol K, Kjeldsen SE, Julius S, Hua TA, Rothwell PM, Mancia G, Parati G, Weber MA, Berge E (2018) Blood pressure variability and risk of cardiovascular events and death in patients with hypertension and different baseline risks. Eur Heart J 39(24):2243–2251
Torjesen A, Cooper LL, Rong J, Larson MG, Hamburg NM, Levy D, Benjamin EJ, Vasan RS, Mitchell GF (2017) Relations of arterial stiffness with postural change in mean arterial pressure in middle-aged adults: the Framingham Heart Study. Hypertension 69(4):685–690
Okada Y, Galbreath MM, Shibata S, Jarvis SS, VanGundy TB, Meier RL, Vongpatanasin W, Levine BD, Fu Q (2012) Relationship between sympathetic baroreflex sensitivity and arterial stiffness in elderly men and women. Hypertension 59(1):98–104
Nilsson PM (2014) Hemodynamic aging as the consequence of structural changes associated with early vascular aging (EVA). Aging Dis 5(2):109–113
Van Bortel LM, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank JK, De Backer T, Filipovsky J, Huybrechts S, Mattace-Raso FU, Protogerou AD et al (2012) Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J Hypertens 30(3):445–448
Janner JH, Godtfredsen NS, Ladelund S, Vestbo J, Prescott E (2010) Aortic augmentation index: reference values in a large unselected population by means of the SphygmoCor device. Am J Hypertens 23(2):180–185
Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, Vita JA, Levy D, Benjamin EJ (2010) Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation 121(4):505–511
Brunkwall L, Jonsson D, Ericson U, Hellstrand S, Kennback C, Ostling G, Jujic A, Melander O, Engstrom G, Nilsson J et al (2021) The Malmo Offspring Study (MOS): design, methods and first results. Eur J Epidemiol 36(1):103–116
Taimour S, Gottsater A, Jujic A, Nilsson PM (2021) Hyperglycemia and arterial stiffness across two generations. J Hypertens 39(3):471–475
Holland DJ, Sacre JW, McFarlane SJ, Coombes JS, Sharman JE (2008) Pulse wave analysis is a reproducible technique for measuring central blood pressure during hemodynamic perturbations induced by exercise. Am J Hypertens 21(10):1100–1106
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Benvenuto LJ, Krakoff LR (2011) Morbidity and mortality of orthostatic hypotension: implications for management of cardiovascular disease. Am J Hypertens 24(2):135–144
Johansson M, Ricci F, Aung N, Sutton R, Melander O, Fedorowski A (2018) Proteomic profiling for cardiovascular biomarker discovery in orthostatic hypotension. Hypertension 71(3):465–472
Smit AA, Halliwill JR, Low PA, Wieling W (1999) Pathophysiological basis of orthostatic hypotension in autonomic failure. J Physiol 519(Pt 1):1–10
Nolde JM, Lugo-Gavidia LM, Kannenkeril D, Chan J, Matthews VB, Carnagarin R, Azzam O, Kiuchi MG, Schlaich MP (2021) Increased pulse wave velocity in patients with an orthostatic blood pressure rise independent of other cardiovascular risk factors. J Hypertens 39(7):1352–1360
Boutouyrie P, Chowienczyk P, Humphrey JD, Mitchell GF (2021) Arterial stiffness and cardiovascular risk in hypertension. Circ Res 128(7):864–886
Nilsson Wadstrom B, Persson M, Engstrom G, Nilsson PM (2022) Aortic stiffness, inflammation, and incidence of cardiovascular events in elderly participants from the general population. Angiology 73(1):51–59
Ziegler MG (2018) Atherosclerosis and blood pressure variability. Hypertension 71(3):403–405
Simula S, Laitinen T, Vanninen E, Pajunen P, Syvanne M, Hedman A, Hartikainen J (2013) Baroreflex sensitivity in asymptomatic coronary atherosclerosis. Clin Physiol Funct Imaging 33(1):70–74
Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C (2010) Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J 31(15):1865–1871
Yannoutsos A, Rinaldi ER, Zhang Y, Protogerou AD, Safar ME, Blacher J (2015) Central hemodynamics in risk assessment strategies: additive value over and above brachial blood pressure. Curr Pharm Des 21(6):719–729
Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, Boutouyrie P, Cameron J, Chen CH, Cruickshank JK et al (2014) Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol 63(7):636–646
Suojanen LJ, Koskela JK, Wilenius M, Choudhary MK, Hautaniemi EJ, Viik J, Mustonen JT, Porsti IH (2021) Individual changes of central blood pressure in response to upright posture: different hemodynamic phenotypes. J Hypertens 39(12):2403–2412
Cremer A, Boutouyrie P, Laurent S, Gosse P, Tzourio C (2020) Orthostatic hypotension: a marker of blood pressure variability and arterial stiffness: a cross-sectional study on an elderly population: the 3-City study. J Hypertens 38(6):1103–1109
Mattace-Raso FU, van der Cammen TJ, Knetsch AM, van den Meiracker AH, Schalekamp MA, Hofman A, Witteman JC (2006) Arterial stiffness as the candidate underlying mechanism for postural blood pressure changes and orthostatic hypotension in older adults: the Rotterdam Study. J Hypertens 24(2):339–344
Takahashi M, Miyai N, Nagano S, Utsumi M, Oka M, Yamamoto M, Shiba M, Uematsu Y, Nishimura Y, Takeshita T et al (2015) Orthostatic blood pressure changes and subclinical markers of atherosclerosis. Am J Hypertens 28(9):1134–1140
Butlin M, Qasem A (2017) Large artery stiffness assessment using SphygmoCor technology. Pulse (Basel) 4(4):180–192
Sperling J, Nilsson PM (2020) Does early life programming influence arterial stiffness and central hemodynamics in adulthood? J Hypertens 38(3):481–488
Kotsis V, Stabouli S, Karafillis I, Nilsson P (2011) Early vascular aging and the role of central blood pressure. J Hypertens 29(10):1847–1853
Acknowledgements
Concept and design: P.M.N., M.J., V.H., A.F., J.J., G.E. Acquisition of data: P.M.N. Statistical analysis: M.J. and V.H. Interpretation of data: M.J., V.H., A.F., P.M.N., J.J., G.E. Drafting of the manuscript: M.J. Critical revision and approval of the manuscript: M.J., V.H., A.F., P.M.N., J.J., G.E. We acknowledge support from the Lund University Infrastructure grant to the “Malmö population-based cohorts” (LU STYR 2019/2046). We thank data manager Anders Dahlin for his extensive and exceptional work with quality control of MOS data, and the staff at the Clinical Research Unit, Department of Internal Medicine, SUS, Malmö, for their dedicated work.
Funding
Open access funding provided by Lund University. The Malmö Offspring Study (MOS) was funded by the Research Council of Sweden (Grant 521-2013-2756), the Swedish Heart and Lung Foundation (Grant 2015-0427), the local Region Skåne County Council, the European Research Council, the Ernhold Lundström Foundation, and Skåne University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A.F. received consultant and lecture fees from Medtronic Inc, Argenx BV and Finapres Medical Systems. J.J. received research support from Novo-Nordisk and Boehringer-Ingelheim and is co-founder of Eternygen GmbH. The remaining authors have no conflicts of interest to declare.
Ethical approval
This study was approved by the appropriate ethics committee and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants gave their written informed consent prior to inclusion.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Johansson, M., Fedorowski, A., Jordan, J. et al. Orthostatic blood pressure adaptations, aortic stiffness, and central hemodynamics in the general population: insights from the Malmö Offspring Study (MOS). Clin Auton Res 33, 29–40 (2023). https://doi.org/10.1007/s10286-022-00911-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-022-00911-z