Abstract
The present study aimed to identify and compare the microbial signatures between periodontally healthy and periodontitis subjects using 454 sequences of 16S rRNA genes. Subgingival plaque samples were collected from ten periodontally healthy subjects and ten matched chronic periodontitis patients. Bacterial DNA was extracted and next-generation sequencing of 16S rRNA genes was performed. The microbial composition differed between healthy subjects and periodontitis patients at all phylogenetic levels. Particularly, 16 species, including Lautropia mirabilis and Neisseria subflava predominated in healthy subjects, whereas nine species, including Porphyromonas gingivalis and Filifactor alocis predominated in periodontitis. UniFrac, a principal coordinate and network analysis, confirmed distinct community profiles in healthy subjects and periodontitis patients. Using predicted function profiling, pathways involved in phenylpropanoid, GPI-anchor biosynthesis, and metabolism of alanine, arginine, aspartate, butanoate, cyanoamino acid, fatty acid, glutamate, methane, proline, and vitamin B6 were significantly over-represented in periodontitis patients. These results highlight the oral microbiota alterations in microbial composition in periodontitis and suggest the genes and metabolic pathways associated with health and periodontitis. Our findings help to further elucidate microbial composition and interactions in health and periodontitis.






Similar content being viewed by others
References
Burt B, Research SiaTCotAAoP. Position paper: epidemiology of periodontal diseases. J Periodontol. 2005;76(8):1406–19. https://doi.org/10.1902/jop.2005.76.8.1406.
Dewhirst FE, Chen T, Izard J, Paster BJ, Tanner ACR, Yu WH, et al. The human oral microbiome. J Bacteriol. 2010;192(19):5002–17. https://doi.org/10.1128/jb.00542-10.
Jenkinson HF, Lamont RJ. Oral microbial communities in sickness and in health. Trends Microbiol. 2005;13(12):589–95. https://doi.org/10.1016/j.tim.2005.09.006.
Aas JA, Paster BJ, Stokes LN, Olsen I, Dewhirst FE. Defining the normal bacterial flora of the oral cavity. J Clin Microbiol. 2005;43(11):5721–32. https://doi.org/10.1128/JCM.43.11.5721-5732.2005.
Costalonga M, Herzberg MC. The oral microbiome and the immunobiology of periodontal disease and caries. Immunol Lett. 2014;162(2 Pt A):22–38. https://doi.org/10.1016/j.imlet.2014.08.017.
Kilian M, Chapple IL, Hannig M, Marsh PD, Meuric V, Pedersen AM, et al. The oral microbiome—an update for oral healthcare professionals. Br Dent J. 2016;221(10):657–66. https://doi.org/10.1038/sj.bdj.2016.865.
Holt SC, Ebersole JL. Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia: the “red complex”, a prototype polybacterial pathogenic consortium in periodontitis. Periodontology. 2000;2005(38):72–122. https://doi.org/10.1111/j.1600-0757.2005.00113.x.
Lamont RJ, Koo H, Hajishengallis G. The oral microbiota: dynamic communities and host interactions. Nat Rev Microbiol. 2018;16(12):745–59. https://doi.org/10.1038/s41579-018-0089-x.
Griffen AL, Beall CJ, Campbell JH, Firestone ND, Kumar PS, Yang ZK, et al. Distinct and complex bacterial profiles in human periodontitis and health revealed by 16S pyrosequencing. ISME J. 2012;6(6):1176–85. https://doi.org/10.1038/ismej.2011.191.
Li Y, He J, He Z, Zhou Y, Yuan M, Xu X, et al. Phylogenetic and functional gene structure shifts of the oral microbiomes in periodontitis patients. ISME J. 2014;8(9):1879–91. https://doi.org/10.1038/ismej.2014.28.
Duran-Pinedo AE, Chen T, Teles R, Starr JR, Wang X, Krishnan K, et al. Community-wide transcriptome of the oral microbiome in subjects with and without periodontitis. ISME J. 2014;8(8):1659–72. https://doi.org/10.1038/ismej.2014.23.
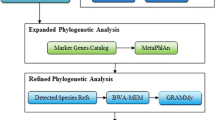
Ai D, Huang R, Wen J, Li C, Zhu J, Xia LC. Integrated metagenomic data analysis demonstrates that a loss of diversity in oral microbiota is associated with periodontitis. BMC Genomics. 2017;18(Suppl 1):1041. https://doi.org/10.1186/s12864-016-3254-5.
Park OJ, Yi H, Jeon JH, Kang SS, Koo KT, Kum KY, et al. Pyrosequencing analysis of subgingival microbiota in distinct periodontal conditions. J Dent Res. 2015;94(7):921–7. https://doi.org/10.1177/0022034515583531.
Abusleme L, Dupuy AK, Dutzan N, Silva N, Burleson JA, Strausbaugh LD, et al. The subgingival microbiome in health and periodontitis and its relationship with community biomass and inflammation. ISME J. 2013;7(5):1016–25. https://doi.org/10.1038/ismej.2012.174.
Duran-Pinedo AE, Yost S, Frias-Lopez J. Small RNA transcriptome of the oral microbiome during periodontitis progression. Appl Environ Microbiol. 2015;81(19):6688–99. https://doi.org/10.1128/AEM.01782-15.
Wang J, Qi J, Zhao H, He S, Zhang Y, Wei S, et al. Metagenomic sequencing reveals microbiota and its functional potential associated with periodontal disease. Sci Rep. 2013;3:1843. https://doi.org/10.1038/srep01843.
Ganesan SM, Joshi V, Fellows M, Dabdoub SM, Nagaraja HN, O’Donnell B, et al. A tale of two risks: smoking, diabetes and the subgingival microbiome. ISME J. 2017;11(9):2075–89. https://doi.org/10.1038/ismej.2017.73.
Graves DT, Correa JD, Silva TA. The oral microbiota is modified by systemic diseases. J Dent Res. 2019;98(2):148–56. https://doi.org/10.1177/0022034518805739.
Beyer K, Zaura E, Brandt BW, Buijs MJ, Brun JG, Crielaard W, et al. Subgingival microbiome of rheumatoid arthritis patients in relation to their disease status and periodontal health. PLoS One. 2018;13(9):e0202278. https://doi.org/10.1371/journal.pone.0202278.
Nasidze I, Li J, Schroeder R, Creasey JL, Li M, Stoneking M. High diversity of the saliva microbiome in Batwa Pygmies. PLoS One. 2011;6(8):e23352. https://doi.org/10.1371/journal.pone.0023352.
Takeshita T, Matsuo K, Furuta M, Shibata Y, Fukami K, Shimazaki Y, et al. Distinct composition of the oral indigenous microbiota in South Korean and Japanese adults. Sci Rep. 2014;4:6990. https://doi.org/10.1038/srep06990.
Asakawa M, Takeshita T, Furuta M, Kageyama S, Takeuchi K, Hata J, et al. Tongue microbiota and oral health status in community-dwelling elderly adults. mSphere. 2018;3:4. https://doi.org/10.1128/msphere.00332-18.
Takeshita T, Kageyama S, Furuta M, Tsuboi H, Takeuchi K, Shibata Y, et al. Bacterial diversity in saliva and oral health-related conditions: the Hisayama study. Sci Rep. 2016;6:22164. https://doi.org/10.1038/srep22164.
Simón-Soro A, Tomás I, Cabrera-Rubio R, Catalan MD, Nyvad B, Mira A. Microbial geography of the oral cavity. J Dent Res. 2013;92(7):616–21. https://doi.org/10.1177/0022034513488119.
Shiba T, Watanabe T, Kachi H, Koyanagi T, Maruyama N, Murase K, et al. Distinct interacting core taxa in co-occurrence networks enable discrimination of polymicrobial oral diseases with similar symptoms. Sci Rep. 2016;6:30997. https://doi.org/10.1038/srep30997.
Maruyama N, Maruyama F, Takeuchi Y, Aikawa C, Izumi Y, Nakagawa I. Intraindividual variation in core microbiota in peri-implantitis and periodontitis. Sci Rep. 2014;4:6602. https://doi.org/10.1038/srep06602.
Rosier BT, Marsh PD, Mira A. Resilience of the oral microbiota in health: mechanisms that prevent dysbiosis. J Dent Res. 2018;97(4):371–80. https://doi.org/10.1177/0022034517742139.
Said HS, Suda W, Nakagome S, Chinen H, Oshima K, Kim S, et al. Dysbiosis of salivary microbiota in inflammatory bowel disease and its association with oral immunological biomarkers. DNA Res. 2014;21(1):15–25. https://doi.org/10.1093/dnares/dst037.
Kim SW, Suda W, Kim S, Oshima K, Fukuda S, Ohno H, et al. Robustness of gut microbiota of healthy adults in response to probiotic intervention revealed by high-throughput pyrosequencing. DNA Res. 2013;20(3):241–53. https://doi.org/10.1093/dnares/dst006.
Berry D, Widder S. Deciphering microbial interactions and detecting keystone species with co-occurrence networks. Front Microbiol. 2014;5:219. https://doi.org/10.3389/fmicb.2014.00219.
Milici M, Deng ZL, Tomasch J, Decelle J, Wos-Oxley ML, Wang H, et al. Co-occurrence analysis of microbial taxa in the atlantic ocean reveals high connectivity in the free-living bacterioplankton. Front Microbiol. 2016;7:649. https://doi.org/10.3389/fmicb.2016.00649.
Friedman J, Alm EJ. Inferring correlation networks from genomic survey data. PLoS Comput Biol. 2012;8(9):e1002687. https://doi.org/10.1371/journal.pcbi.1002687.
Smoot ME, Ono K, Ruscheinski J, Wang PL, Ideker T. Cytoscape 2.8: new features for data integration and network visualization. Bioinformatics. 2011;27(3):431–2. https://doi.org/10.1093/bioinformatics/btq675.
Iwai S, Weinmaier T, Schmidt BL, Albertson DG, Poloso NJ, Dabbagh K, et al. Piphillin: improved prediction of metagenomic content by direct inference from human microbiomes. PLoS One. 2016;11(11):e0166104. https://doi.org/10.1371/journal.pone.0166104.
Perez-Chaparro PJ, Goncalves C, Figueiredo LC, Faveri M, Lobao E, Tamashiro N, et al. Newly identified pathogens associated with periodontitis: a systematic review. J Dent Res. 2014;93(9):846–58. https://doi.org/10.1177/0022034514542468.
Chen H, Liu Y, Zhang M, Wang G, Qi Z, Bridgewater L, et al. A Filifactor alocis-centered co-occurrence group associates with periodontitis across different oral habitats. Sci Rep. 2015;5:9053. https://doi.org/10.1038/srep09053.
Armstrong CL, Miralda I, Neff AC, Tian S, Vashishta A, Perez L, et al. Filifactor alocis promotes neutrophil degranulation and chemotactic activity. Infect Immun. 2016;84(12):3423–33. https://doi.org/10.1128/IAI.00496-16.
Szafranski SP, Wos-Oxley ML, Vilchez-Vargas R, Jauregui R, Plumeier I, Klawonn F, et al. High-Resolution taxonomic profiling of the subgingival microbiome for biomarker discovery and periodontitis diagnosis. Appl Environ Microbiol. 2015;81(3):1047–58. https://doi.org/10.1128/aem.03534-14.
Kirst ME, Li EC, Alfant B, Chi YY, Walker C, Magnusson I, et al. Dysbiosis and alterations in predicted functions of the subgingival microbiome in chronic periodontitis. Appl Environ Microbiol. 2015;81(2):783–93. https://doi.org/10.1128/aem.02712-14.
Hajishengallis G, Lamont RJ. Beyond the red complex and into more complexity: the polymicrobial synergy and dysbiosis (PSD) model of periodontal disease etiology. Mol Oral Microbiol. 2012;27(6):409–19. https://doi.org/10.1111/j.2041-1014.2012.00663.x.
Duran-Pinedo AE, Paster B, Teles R, Frias-Lopez J. Correlation network analysis applied to complex biofilm communities. PLoS One. 2011;6(12):e28438. https://doi.org/10.1371/journal.pone.0028438.
Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL. Microbial complexes in subgingival plaque. J Clin Periodontol. 1998;25(2):134–44.
Hajishengallis G, Liang S, Payne MA, Hashim A, Jotwani R, Eskan MA, et al. Low-abundance biofilm species orchestrates inflammatory periodontal disease through the commensal microbiota and complement. Cell Host Microbe. 2011;10(5):497–506. https://doi.org/10.1016/j.chom.2011.10.006.
Sturgeon A, Stull JW, Costa MC, Weese JS. Metagenomic analysis of the canine oral cavity as revealed by high-throughput pyrosequencing of the 16S rRNA gene. Vet Microbiol. 2013;162(2–4):891–8. https://doi.org/10.1016/j.vetmic.2012.11.018.
Gerner-Smidt P, Keiser-Nielsen H, Dorsch M, Stackebrandt E, Ursing J, Blom J, et al. Lautropia mirabilis gen. nov., sp. nov., a gram-negative motile coccus with unusual morphology isolated from the human mouth. Microbiology. 1994;140(Pt 7):1787–97. https://doi.org/10.1099/13500872-140-7-1787.
Zhang SM, Tian F, Huang QF, Zhao YF, Guo XK, Zhang FQ. Bacterial diversity of subgingival plaque in 6 healthy Chinese individuals. Exp Ther Med. 2011;2(5):1023–9. https://doi.org/10.3892/etm.2011.311.
Jorth P, Turner KH, Gumus P, Nizam N, Buduneli N, Whiteley M. Metatranscriptomics of the human oral microbiome during health and disease. MBio. 2014;5(2):e01012–4. https://doi.org/10.1128/mBio.01012-14.
Langille MG, Zaneveld J, Caporaso JG, McDonald D, Knights D, Reyes JA, et al. Predictive functional profiling of microbial communities using 16S rRNA marker gene sequences. Nat Biotechnol. 2013;31(9):814–21. https://doi.org/10.1038/nbt.2676.
Liu B, Faller LL, Klitgord N, Mazumdar V, Ghodsi M, Sommer DD, et al. Deep sequencing of the oral microbiome reveals signatures of periodontal disease. PLoS One. 2012;7(6):e37919. https://doi.org/10.1371/journal.pone.0037919.
Naqvi AZ, Buettner C, Phillips RS, Davis RB, Mukamal KJ. n-3 fatty acids and periodontitis in US adults. J Am Diet Assoc. 2010;110(11):1669–75. https://doi.org/10.1016/j.jada.2010.08.009.
Fischer CL, Walters KS, Drake DR, Dawson DV, Blanchette DR, Brogden KA, et al. Oral mucosal lipids are antibacterial against Porphyromonas gingivalis, induce ultrastructural damage, and alter bacterial lipid and protein compositions. Int J Oral Sci. 2013;5(3):130–40. https://doi.org/10.1038/ijos.2013.28.
Kim H. Glutamine as an immunonutrient. Yonsei Med J. 2011;52(6):892–7. https://doi.org/10.3349/ymj.2011.52.6.892.
Efron D, Barbul A. Role of arginine in immunonutrition. J Gastroenterol. 2000;35(Suppl 12):20–3.
Morita M, Wang HL. Relationship of sulcular sulfide level to severity of periodontal disease and BANA test. J Periodontol. 2001;72(1):74–8. https://doi.org/10.1902/jop.2001.72.1.74.
Waler SM. On the transformation of sulfur-containing amino acids and peptides to volatile sulfur compounds (VSC) in the human mouth. Eur J Oral Sci. 1997;105(5 Pt 2):534–7.
Zhang JH, Dong Z, Chu L. Hydrogen sulfide induces apoptosis in human periodontium cells. J Periodontal Res. 2010;45(1):71–8. https://doi.org/10.1111/j.1600-0765.2009.01202.x.
Ikeda E, Shiba T, Ikeda Y, Suda W, Nakasato A, Takeuchi Y, et al. Deep sequencing reveals specific bacterial signatures in the subgingival microbiota of healthy subjects. Clin Oral Investig. 2019. https://doi.org/10.1007/s00784-019-02805-3.
Acknowledgements
This work was supported by the Japan Society for the Promotion of Science KAKENHI; under Grant 26463129 and under Grant 17K11981. We also thank Dr. Walter Meinzer and Dr. Daiki Tanaka for critical reading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interests.
Research involving human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of Tokyo Medical and Dental University Institutional Review Board (No. 1138) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from all enrolled individuals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ikeda, E., Shiba, T., Ikeda, Y. et al. Japanese subgingival microbiota in health vs disease and their roles in predicted functions associated with periodontitis. Odontology 108, 280–291 (2020). https://doi.org/10.1007/s10266-019-00452-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-019-00452-4