Abstract
Systemic lupus erythematosus (SLE) is an autoimmune disease associated with hyperactive innate and adaptive immune systems that cause dermatological, cardiovascular, renal, and neuropsychiatric problems in patients. SLE's multifactorial nature and complex pathogenesis present significant challenges in its clinical classification. In addition, unpredictable treatment responses in patients emphasize the need for highly specific and sensitive SLE biomarkers that can assist in understanding the exact pathogenesis and, thereby, lead to the identification of novel therapeutic targets. Recent studies on microRNA (miRNA), a non-coding region involved in the regulation of gene expression, indicate its importance in the development of the immune system and thus in the pathogenesis of various autoimmune disorders such as SLE. miRNAs are fascinating biomarker prospects for SLE categorization and disease monitoring owing to their small size and high stability. In this paper, we have discussed the involvement of a wide range of miRNAs in the regulation of SLE inflammation and how their modulation can be a potential therapeutic approach.



Similar content being viewed by others
Data availability
Not applicable.
Abbreviations
- AGO:
-
Argonaute
- BAFF:
-
B-cell-activating-factor
- BBB:
-
Blood-brain barrier
- BLIMP:
-
B-lymphocyte-induced-maturation-protein-1
- CD4+ :
-
Cluster-of-differentiation-4
- CD40L:
-
CD40 ligand
- CRKL:
-
Crk-like
- CXCL2:
-
Chemokine-C-X-C-motif-ligand-2
- DGCR8:
-
DiGeorge-Syndrome-critical-region-8
- DNMTs:
-
DNA methyltransferases
- DUSP:
-
Dual-specificity-protein-phosphatase
- EGR1:
-
Early-growth-response-protein-1
- Foxo1:
-
Forkhead-box-protein-O-1
- Gadd45a:
-
Growth-arrest-and-DNA-damage-inducible-protein-45-alpha
- IFIT1:
-
Interferon-induced-protein-with-tetratricopeptide-repeats-1
- IFN:
-
Interferon
- Ig:
-
Immunoglobulin
- IL:
-
Interleukin
- IRAK1:
-
IL-1-receptor-associated-kinase-1
- IRAKM:
-
Interleukin-1-receptor-associated-kinase-M
- IRF5:
-
Interferon-regulatory-factor-5
- JAK-STAT:
-
Janus-kinase-signal-transducers-and-activators-of-transcription
- KLF13:
-
Kruppel-like-factor 13
- miRNA:
-
MicroRNA
- MyD88:
-
Myeloid-differentiation-protein-88
- NETs:
-
Neutrophil Extracellular Traps
- NFκB:
-
Nuclear-factor-kappa-B
- PBMCs:
-
Peripheral blood mononuclear cells
- PDCD4:
-
Programmed-cell-death 4
- pDCs:
-
Plasmacytoid dendritic cells
- pre-miRNA:
-
Precursor-miRNA
- pri-miRNA:
-
Primary miRNA
- PRRs:
-
Pattern recognition receptors
- PTEN:
-
Phosphatase-and-tensin-homolog
- PTPN22:
-
Protein-tyrosine-phosphatase-non-receptor-type 22
- Ran:
-
RAs-related-nuclear-protein
- RASGRP1:
-
RAS-guanyl- nucleotide-releasing-protein
- RIG:
-
Retinoic-acid inducible gene
- RISC:
-
RNA-induced-silencing-complex
- SHP-2:
-
Src-homology-region-2
- SLE:
-
Systemic lupus erythematosus
- SNP:
-
Single-nucleotide polymorphism
- SOCS:
-
Suppressors-of-cytokine-signaling
- SPI1 or PU.1:
-
Spi-1-proto-oncogene
- STAM:
-
Signal-transducing-adapter-molecule
- STAT1:
-
Signal-transducer-and-activator-of-transcription-1
- TAB2:
-
TGF-beta-activated-kinase-1-(MAP3K7)-binding-protein-2
- TCR:
-
T-cell receptors
- Th:
-
T-helper
- TLRs:
-
Toll-like receptors
- TRAF6:
-
TNF-receptor-associated-factor-6
- T-reg:
-
T regulatory
- UTRs:
-
Untranslated regions
- XPO5:
-
Exportin 5
References
Barber MRW, Drenkard C, Falasinnu T, et al. Global epidemiology of systemic lupus erythematosus. Nat Rev Rheumatol. 2021;17:515–32. https://doi.org/10.1038/s41584-021-00668-1.
Kane BS, Niasse M, Ndiaye AA, et al. Systemic diseases in Dakar (Senegal): spectrum, epidemiological aspect and diagnostic time-limit. Open J Intern Med. 2018;08:196–206. https://doi.org/10.4236/ojim.2018.83019.
Grennan DM, Bossingham D. Systemic lupus erythematosus (SLE): different prevalences in different populations of Australian aboriginals. Aust N Z J Med. 1995;25:182–3. https://doi.org/10.1111/j.1445-5994.1995.tb02843.x.
Magro R, Borg AA. Characterisation of patients with systemic lupus erythematosus in Malta: a population based cohort cross-sectional study. BioMed Res Int. 2018;2018:2385386. https://doi.org/10.1155/2018/2385386.
Anstey NM, Bastian I, Dunckley H, Currie BJ. Systemic lupus erythematosus in Australian aborigines: high prevalence, morbidity and mortality. Aust N Z J Med. 1993;23:646–51. https://doi.org/10.1111/j.1445-5994.1993.tb04720.x.
Tan G, Baby B, Zhou Y, Wu T. Emerging molecular markers towards potential diagnostic panels for lupus. Front Immunol. 2021;12:808839. https://doi.org/10.3389/fimmu.2021.808839.
Nossent J, Kiss E, Rozman B, et al. Disease activity and damage accrual during the early disease course in a multinational inception cohort of patients with systemic lupus erythematosus. Lupus. 2010;19:949–56. https://doi.org/10.1177/0961203310366572.
Katsuyama T, Tsokos GC, Moulton VR. Aberrant T cell signaling and subsets in systemic lupus erythematosus. Front Immunol. 2018;9:1088. https://doi.org/10.3389/fimmu.2018.01088.
Karrar S, Cunninghame Graham DS. Abnormal B cell development in systemic lupus erythematosus. Arthritis Rheumatol. 2018;70:496–507. https://doi.org/10.1002/art.40396.
Yu H, Nagafuchi Y, Fujio K. Clinical and immunological biomarkers for systemic lupus erythematosus. Biomolecules. 2021;11:928. https://doi.org/10.3390/biom11070928.
Wang W, Yue C, Gao S, et al. Promising roles of exosomal microRNAs in systemic lupus erythematosus. Front Immunol. 2021;12:757096. https://doi.org/10.3389/fimmu.2021.757096.
Hong SM, Liu C, Yin Z, Wu L, Qu B, Shen N. MicroRNAs in systemic lupus erythematosus: a perspective on the path from biological discoveries to clinical practice. Curr Rheumatol Rep. 2020;22:17. https://doi.org/10.1007/s11926-020-00895-7.
Zhang L, Wu H, Zhao M, Chang C, Lu Q. Clinical significance of miRNAs in autoimmunity. J Autoimmun. 2020;109:102438. https://doi.org/10.1016/j.jaut.2020.102438.
Kai K, Dittmar RL, Sen S. Secretory microRNAs as biomarkers of cancer. Semin Cell Dev Biol. 2018;78:22–36. https://doi.org/10.1016/j.semcdb.2017.12.011.
O’Brien J, Hayder H, Zayed Y, Peng C. Overview of MicroRNA biogenesis, mechanisms of actions, and circulation. Front Endocrinol. 2018;9:402. https://doi.org/10.3389/fendo.2018.00402.
Pal AS, Kasinski AL. Animal models to study microRNA function. Adv Cancer Res. 2017;135:53–118. https://doi.org/10.1016/bs.acr.2017.06.006.
Condrat CE, Thompson DC, Barbu MG, et al. miRNAs as biomarkers in disease: latest findings regarding their role in diagnosis and prognosis. Cells. 2020;9:276.
Lopez-Pedrera C, Barbarroja N, Patiño-Trives AM, et al. Role of microRNAs in the development of cardiovascular disease in systemic autoimmune disorders. Int J Mol Sci. 2020;21:2012.
Hussein M, Magdy R. MicroRNAs in central nervous system disorders: current advances in pathogenesis and treatment. Egypt J Neurol Psychiatry Neurosurg. 2021;57:36. https://doi.org/10.1186/s41983-021-00289-1.
Lan H, Lu H, Wang X, Jin H. MicroRNAs as potential biomarkers in cancer: opportunities and challenges. BioMed Res Int. 2015;2015:125094. https://doi.org/10.1155/2015/125094.
Honarpisheh M, Köhler P, von Rauchhaupt E, Lech M. The involvement of MicroRNAs in modulation of innate and adaptive immunity in systemic lupus erythematosus and lupus nephritis. J Immunol Res. 2018;2018:4126106. https://doi.org/10.1155/2018/4126106.
Treiber T, Treiber N, Meister G. Regulation of microRNA biogenesis and its crosstalk with other cellular pathways. Nat Rev Mol Cell Biol. 2019;20:5–20. https://doi.org/10.1038/s41580-018-0059-1.
Schell SL, Rahman ZSM. miRNA-mediated control of B cell responses in immunity and SLE. Front Immunol. 2021;12: 683710. https://doi.org/10.3389/fimmu.2021.683710.
Chi SW, Zang JB, Mele A, Darnell RB. Argonaute HITS-CLIP decodes microRNA-mRNA interaction maps. Nature. 2009;460:479–86. https://doi.org/10.1038/nature08170.
Lewis BP, Burge CB, Bartel DP. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cel. 2005;120:15–20. https://doi.org/10.1016/j.cell.2004.12.035.
Lee I, Ajay SS, Yook JI, et al. New class of microRNA targets containing simultaneous 5′-UTR and 3′-UTR interaction sites. Genome Res. 2009;19:1175–83. https://doi.org/10.1101/gr.089367.108.
Denzler R, McGeary SE, Title AC, Agarwal V, Bartel DP, Stoffel M. Impact of MicroRNA levels, target-site complementarity, and cooperativity on competing endogenous RNA-regulated gene expression. Mol Cell. 2016;64:565–79.
Landgraf P, Rusu M, Sheridan R, et al. A mammalian microRNA expression atlas based on small RNA library sequencing. Cell. 2007;129:1401–14. https://doi.org/10.1016/j.cell.2007.04.040.
Hsin JP, Lu Y, Loeb GB, Leslie CS, Rudensky AY. The effect of cellular context on miR-155-mediated gene regulation in four major immune cell types. Nat Immunol. 2018;19:1137–45. https://doi.org/10.1038/s41590-018-0208-x.
Carlsen AL, Schetter AJ, Nielsen CT, et al. Circulating microRNA expression profiles associated with systemic lupus erythematosus. Arthritis Rheum. 2013;65:1324–34. https://doi.org/10.1002/art.37890.
Luo X, Tsai LM, Shen N, Yu D. Evidence for microRNA-mediated regulation in rheumatic diseases. Ann Rheum Dis. 2010;1:30–6. https://doi.org/10.1136/ard.2009.117218.
Dai Y, Sui W, Lan H, Yan Q, Huang H, Huang Y. Comprehensive analysis of microRNA expression patterns in renal biopsies of lupus nephritis patients. Rheumatol Int. 2009;29:749–54. https://doi.org/10.1007/s00296-008-0758-6.
Te JL, Dozmorov IM, Guthridge JM, et al. Identification of unique microRNA signature associated with lupus nephritis. PLoS ONE. 2010;5:10344. https://doi.org/10.1371/journal.pone.0010344.
Zhang X, Yao B, Hu Q, et al. Detection of biomarkers in body fluids using bioprobes based on aggregation-induced emission fluorogens. Mater Chem Front. 2010;4:2548–70. https://doi.org/10.1039/D0QM00376J.
Aristizábal B, González Á, et al. Innate immune system. In: Anaya JM, Shoenfeld Y, Rojas-Villarraga A, et al., editors. Autoimmunity: From Bench to Bedside. Bogota: El Rosario University Press; 2013.
Lamkanfi M, Dixit VM. Inflammasomes and their roles in health and disease. Annu Rev Cell Dev Biol. 2012;28:137–61. https://doi.org/10.1146/annurev-cellbio-101011-155745.
Medzhitov R, Janeway CA. Innate immunity: impact on the adaptive immune response. Curr Opin Immunol. 1997;9:4–9. https://doi.org/10.1016/s0952-7915(97)80152-5.
Banchereau J, Pascual V. Type I interferon in systemic lupus erythematosus and other autoimmune diseases. Immunity. 2006;25:383–92. https://doi.org/10.1016/j.immuni.2006.08.010.
Shrivastav M, Niewold TB. Nucleic acid sensors and type I interferon production in systemic lupus erythematosus. Front Immunol. 2013;4:319.
Tang Y, Luo X, Cui H, et al. MicroRNA-146A contributes to abnormal activation of the type I interferon pathway in human lupus by targeting the key signaling proteins. Arthritis Rheum. 2009;60:1065–75. https://doi.org/10.1002/art.24436.
Luo X, Yang W, Ye DQ, et al. A functional variant in MicroRNA-146a promoter modulates its expression and confers disease risk for systemic lupus erythematosus. PLoS Genet. 2011;7:1002128.
Hou J, Wang P, Lin L, et al. MicroRNA-146a feedback inhibits RIG-I-dependent Type I IFN production in macrophages by targeting TRAF6, IRAK1, and IRAK2. J Immunol. 2009;83:2150–8. https://doi.org/10.4049/jimmunol.0900707.
Hsieh YT, Chou YC, Kuo PY, et al. Down-regulated miR-146a expression with increased neutrophil extracellular traps and apoptosis formation in autoimmune-mediated diffuse alveolar hemorrhage. J Biomed Sci. 2022;29:62. https://doi.org/10.1186/s12929-022-00849-4.
Taganov KD, Boldin MP, Chang KJ, Baltimore D. NF-kappaB-dependent induction of microRNA miR-146, an inhibitor targeted to signaling proteins of innate immune responses. Proc Natl Acad Sci U S A. 2006;103:12481–6. https://doi.org/10.1073/pnas.0605298103.
Tang B, Xiao B, Liu Z, et al. Identification of MyD88 as a novel target of miR-155, involved in negative regulation of Helicobacter pylori-induced inflammation. FEBS Lett. 2010;584:1481–6. https://doi.org/10.1016/j.febslet.2010.02.063.
von Bernuth H, Picard C, Jin Z, et al. Pyogenic bacterial infections in humans with MyD88 deficiency. Science. 2008;321:691–6. https://doi.org/10.1126/science.1158298.
Zhou H, Huang X, Cui H, et al. miR-155 and its star-form partner miR-155* cooperatively regulate type I interferon production by human plasmacytoid dendritic cells. Blood. 2010;116:5885–94. https://doi.org/10.1182/blood-2010-04-280156.
Gilliet M, Cao W, Liu YJ. Plasmacytoid dendritic cells: sensing nucleic acids in viral infection and autoimmune diseases. Nat Rev Immunol. 2008;8:594–606. https://doi.org/10.1038/nri2358.
Aboelenein HR, Hamza MT, Marzouk H, et al. Reduction of CD19 autoimmunity marker on B cells of paediatric SLE patients through repressing PU.1/TNF-α/BAFF axis pathway by miR-155. Growth Fact. 2017;35:49–60. https://doi.org/10.1080/08977194.2017.1345900.
Mishra R, Bhattacharya S, Rawat BS, et al. MicroRNA-30e-5p has an integrated role in the regulation of the innate immune response during virus infection and systemic lupus erythematosus. iScience. 2020;23:101322.
Yang B, Huang X, Xu S, et al. Decreased miR-4512 levels in monocytes and macrophages of individuals with systemic lupus erythematosus contribute to innate immune activation and neutrophil NETosis by targeting TLR4 and CXCL2. Front Immunol. 2021;12:756825. https://doi.org/10.3389/fimmu.2021.756825.
Wang Y, Liu X, Xia P, et al. The regulatory role of MicroRNAs on phagocytes: a potential therapeutic target for chronic diseases. Front Immunol. 2022;13:901166. https://doi.org/10.3389/fimmu.2022.901166.
Yan L, Jiang L, Wang B, et al. Novel microRNA biomarkers of systemic lupus erythematosus in plasma: miR-124-3p and miR-377-3p. Clin Biochem. 2022;107:55–61. https://doi.org/10.1016/j.clinbiochem.2022.05.004.
Ahmed MM, Zaki A, Alhazmi A, et al. Identification and validation of pathogenic genes in sepsis and associated diseases by integrated bioinformatics approach. Genes. 2022;13:209. https://doi.org/10.3390/genes13020209.
Gupta S, Kaplan MJ. The role of neutrophils and NETosis in autoimmune and renal diseases. Nat Rev Nephrol. 2006;12:402–13. https://doi.org/10.1038/nrneph.2016.71.
Sadeghi M, Dehnavi S, Jamialahmadi T, Johnston TP, Sahebkar A. Neutrophil extracellular trap: a key player in the pathogenesis of autoimmune diseases. Int Immunopharmacol. 2023;116:109843. https://doi.org/10.1016/j.intimp.2023.109843.
Blanco LP, Wang X, Carlucci PM, et al. RNA externalized by neutrophil extracellular traps promotes inflammatory pathways in endothelial cells. Arthritis Rheumatol. 2021;73:2282–92. https://doi.org/10.1002/art.41796.
Deng Y, Zhao J, Sakurai D, et al. MicroRNA-3148 modulates allelic expression of toll-like receptor 7 variant associated with systemic lupus erythematosus. PLoS Genet. 2013;9:1003336. https://doi.org/10.1371/journal.pgen.1003336.
Chafin CB, Regna NL, Dai R, Caudell DL, Reilly CM. MicroRNA-let-7a expression is increased in the mesangial cells of NZB/W mice and increases IL-6 production in vitro. Autoimmunity. 2013;46:351–62. https://doi.org/10.3109/08916934.2013.773976.
Kim SJ, Gregersen PK, Diamond B. Regulation of dendritic cell activation by microRNA let-7c and BLIMP1. J Clin Invest. 2013;1232:823–33.
Smith S, Wu PW, Seo JJ, et al. IL-16/miR-125a axis controls neutrophil recruitment in pristane-induced lung inflammation. JCI Insight. 2018;3:120798. https://doi.org/10.1172/jci.insight.120798.
Bonilla FA, Oettgen HC. Adaptive immunity. J Allergy Clin Immunol. 2010;125:33–40. https://doi.org/10.1016/j.jaci.2009.09.017.
Hirschberger S, Hinske LC, Kreth S. MiRNAs: dynamic regulators of immune cell functions in inflammation and cancer. Cancer Lett. 2018;431:11–21. https://doi.org/10.1016/j.canlet.2018.05.020.
Kourti M, Sokratous M, Katsiari CG. Regulation of microRNA in systemic lupus erythematosus: the role of miR-21 and miR-210. Mediterr J Rheumatol. 2020;31:71–4.
Chi M, Ma K, Li Y, et al. Immunological involvement of MicroRNAs in the key events of systemic lupus erythematosus. Front Immunol. 2021;12:699684. https://doi.org/10.3389/fimmu.2021.699684.
Zan H, Tat C, Casali P. MicroRNAs in lupus. Autoimmunity. 2014;47:272–85. https://doi.org/10.3109/08916934.2014.915955.
Cobb BS, Hertweck A, Smith J, et al. A role for Dicer in immune regulation. J Exp Med. 2006;203:2519–27. https://doi.org/10.1084/jem.20061692.
Chen SH, Lv QL, Hu L, Peng MJ, Wang GH, Sun B. DNA methylation alterations in the pathogenesis of lupus. Clin Exp Immunol. 2017;187:185–92.
Pan W, Zhu S, Yuan M, et al. MicroRNA-21 and microRNA-148a contribute to DNA hypomethylation in lupus CD4+ T cells by directly and indirectly targeting DNA methyltransferase 1. J Immunol. 2010;1950(184):6773–81. https://doi.org/10.4049/jimmunol.0904060.
Qin H, Zhu X, Liang J, et al. MicroRNA-29b contributes to DNA hypomethylation of CD4+ T cells in systemic lupus erythematosus by indirectly targeting DNA methyltransferase 1. J Dermatol Sci. 2013;69:61–7. https://doi.org/10.1016/j.jdermsci.2012.10.011.
Zhao S, Wang Y, Liang Y, et al. MicroRNA-126 regulates DNA methylation in CD4+ T cells and contributes to systemic lupus erythematosus by targeting DNA methyltransferase 1. Arthritis Rheum. 2011;63:1376–86. https://doi.org/10.1002/art.30196.
Stagakis E, Bertsias G, Verginis P, et al. Identification of novel microRNA signatures linked to human lupus disease activity and pathogenesis: miR-21 regulates aberrant T cell responses through regulation of PDCD4 expression. Ann Rheum Dis. 2011;70:1496–506. https://doi.org/10.1136/ard.2010.139857.
Zhao X, Tang Y, Qu B, et al. MicroRNA-125a contributes to elevated inflammatory chemokine RANTES levels via targeting KLF13 in systemic lupus erythematosus. Arthritis Rheum. 2010;62:3425–35. https://doi.org/10.1002/art.27632.
Al-hasso IK, Al-Derzi AR, Abbas AA, Gorial FI, Alnuimi AS. The role of microRNAs (MiR-125a and MiR-146a), RANTES, and IFN-γin systemic lupus erythematosus. Ann Trop Med Public Health. 2020. https://doi.org/10.36295/asro.2020.231382.
Motawi TK, Mohsen DA, El-Maraghy SA, Kortam MA. MicroRNA-21, microRNA-181a and microRNA-196a as potential biomarkers in adult Egyptian patients with systemic lupus erythematosus. Chem Biol Interact. 2016;260:110–6. https://doi.org/10.1016/j.cbi.2016.11.001.
Abdul-Maksoud RS, Rashad NM, Elsayed WSH, Ali MA, Kamal NM, Zidan HE. Circulating miR-181a and miR-223 expression with the potential value of biomarkers for the diagnosis of systemic lupus erythematosus and predicting lupus nephritis. J Gene Med. 2021;23:3326. https://doi.org/10.1002/jgm.3326.
Li HS, Ning Y, Li SB, et al. Expression and clinical significance of miR-181a and miR-203 in systemic lupus erythematosus patients. Eur Rev Med Pharmacol Sci. 2017;21:4790–6.
Divekar AA, Dubey S, Gangalum PR, Singh RR. Dicer insufficiency and MicroRNA-155 overexpression in lupus regulatory T cells: an apparent paradox in the setting of an inflammatory milieu. J Immunol. 2011;186:924–30. https://doi.org/10.4049/jimmunol.1002218.
Wang H, Geng G, Zhang D, Han F, Ye S. Analysis of microRNA-199a-3p expression in CD4+ T cells of systemic lupus erythematosus. Clin Rheumatol. 2023;42:1683–94. https://doi.org/10.1007/s10067-023-06534-7.
Wang Z, Heid B, Lu R, et al. Deletion of microRNA-183-96-182 cluster in lymphocytes suppresses Anti-DsDNA autoantibody production and IgG deposition in the kidneys in C57BL/6-Faslpr/lpr Mice. Front Genet. 2022;13:840060. https://doi.org/10.3389/fgene.2022.840060.
Wang Z, Dai R, Ahmed SA. MicroRNA-183/96/182 cluster in immunity and autoimmunity. Front Immunol. 2023;14:1134634. https://doi.org/10.3389/fimmu.2023.1134634.
Brandl A, Daum P, Brenner S, et al. The microprocessor component, DGCR8, is essential for early B-cell development in mice. Eur J Immunol. 2016;46:2710–8. https://doi.org/10.1002/eji.201646348.
Gonzalez-Martin A, Adams BD, Lai M, et al. The microRNA miR-148a functions as a critical regulator of B cell tolerance and autoimmunity. Nat Immunol. 2016;17:433–40.
Humayun A, Fornace AJ. Gadd45 in stress signaling, cell cycle control, and apoptosis. Adv Exp Med Biol. 2022;1360:1–22. https://doi.org/10.1007/978-3-030-94804-7_1.
Ibrahim SA, Afify AY, Fawzy IO, El-Ekiaby N, Abdelaziz AI. The curious case of miR-155 in SLE. Expert Rev Mol Med. 2021;23:11. https://doi.org/10.1017/erm.2021.11.
Aiello FB, Guszczynski T, Li W, et al. IL-7-induced phosphorylation of the adaptor Crk-like and other targets. Cell Signal. 2018;47:131–41. https://doi.org/10.1016/j.cellsig.2018.03.008.
Shi X, Ye L, Xu S, et al. Downregulated miR-29a promotes B cell overactivation by upregulating Crk-like protein in systemic lupus erythematosus. Mol Med Rep. 2020;22:841–9.
Xia Y, Tao JH, Fang X, et al. MicroRNA-326 upregulates B cell activity and autoantibody production in lupus disease of MRL/lpr mice. Mol Ther Nucleic Acids. 2018;11:284–91.
Jin L, Fang X, Dai C, et al. The potential role of Ets-1 and miR-326 in CD19+B cells in the pathogenesis of patients with systemic lupus erythematosus. Clin Rheumatol. 2019;38:1031–8. https://doi.org/10.1007/s10067-018-4371-0.
Talaat RM, Mohamed SF, Bassyouni IH, Raouf AA. Th1/Th2/Th17/Treg cytokine imbalance in systemic lupus erythematosus (SLE) patients: correlation with disease activity. Cytokine. 2015;72:146–53. https://doi.org/10.1016/j.cyto.2014.12.027.
Arkatkar T, Du SW, Jacobs HM, et al. B cell–derived IL-6 initiates spontaneous germinal center formation during systemic autoimmunity. J Exp Med. 2017;214:3207–17.
Fava A, Petri M. Systemic lupus erythematosus: diagnosis and clinical management. J Autoimmun. 2019;96:1–13. https://doi.org/10.1016/J.JAUT.2018.11.001.
Kirou KA, Dall`Era M, Aranow C, Anders HJ. Belimumab or anifrolumab for systemic lupus erythematosus? A risk-benefit assessment. Front Immunol. 2022;13:980079. https://doi.org/10.3389/FIMMU.2022.980079/BIBTEX.
Mok CC, Tse SM, Chan KL, Ho LY. Effect of immunosuppressive therapies on survival of systemic lupus erythematosus: a propensity score analysis of a longitudinal cohort. Lupus. 2017;27(5):722–7. https://doi.org/10.1177/0961203317739129.
Cain DW, Cidlowski JA. Immune regulation by glucocorticoids. Nat Rev Immunol. 2017;17(4):233–47. https://doi.org/10.1038/nri.2017.1.
Skoglund O, Walhelm T, Thyberg I, Eriksson P, Sjöwall C. Fighting fatigue in systemic lupus erythematosus: experience of dehydroepiandrosterone on clinical parameters and patient-reported outcomes. J Clin Med. 2022;11(18):5300. https://doi.org/10.3390/JCM11185300.
Fanouriakis A, Tziolos N, Bertsias G, Boumpas DT. Update οn the diagnosis and management of systemic lupus erythematosus. Ann Rheum Dis. 2021;80(1):14–25. https://doi.org/10.1136/ANNRHEUMDIS-2020-218272.
Cobo-Ibáñez T, Loza-Santamaría E, Pego-Reigosa JM, et al. Efficacy and safety of rituximab in the treatment of non-renal systemic lupus erythematosus: a systematic review. Semin Arthritis Rheum. 2014;44(2):175–85. https://doi.org/10.1016/J.SEMARTHRIT.2014.04.002.
Van Vollenhoven RF, Petri MA, Cervera R, et al. Belimumab in the treatment of systemic lupus erythematosus: high disease activity predictors of response. Ann Rheum Dis. 2012;71(8):1343–9. https://doi.org/10.1136/ANNRHEUMDIS-2011-200937.
Zhang L, Wei W. Anti-inflammatory and immunoregulatory effects of paeoniflorin and total glucosides of paeony. Pharmacol Ther. 2020;207:107452. https://doi.org/10.1016/J.PHARMTHERA.2019.107452.
Durcan L, O’Dwyer T, Petri M. Management strategies and future directions for systemic lupus erythematosus in adults. The Lancet. 2019;393(10188):2332–43. https://doi.org/10.1016/S0140-6736(19)30237-5.
Parra Sánchez AR, Voskuyl AE, van Vollenhoven RF. Treat-to-target in systemic lupus erythematosus: advancing towards its implementation. Nat Rev Rheumatol. 2022;18(3):146–57. https://doi.org/10.1038/s41584-021-00739-3.
Tanaka Y. Systemic lupus erythematosus. Best Pract Res Clin Rheumatol. 2022;36(4):101814. https://doi.org/10.1016/J.BERH.2022.101814.
Chafin CB, Reilly CM. MicroRNAs implicated in the immunopathogenesis of lupus nephritis. Clin Dev Immunol. 2013;2013:430239.
Thai TH, Christiansen PA, Tsokos GC. Is there a link between dysregulated miRNA expression and disease? Discov Med. 2010;10:184–94.
Salvi V, Gianello V, Tiberio L, Sozzani S, Bosisio D. Cytokine targeting by miRNAs in autoimmune diseases. Front Immunol. 2019;10:15.
Christopher AF, Kaur RP, Kaur G, Kaur A, Gupta V, Bansal P. MicroRNA therapeutics: discovering novel targets and developing specific therapy. Perspect Clin Res. 2016;7:68–74. https://doi.org/10.4103/2229-3485.179431.
Tang Q, Yang Y, Zhao M, et al. Mycophenolic acid upregulates miR-142-3P/5P and miR-146a in lupus CD4+T cells. Lupus. 2015;24:935–42. https://doi.org/10.1177/0961203315570685.
Thai TH, Patterson HC, Pham DH, Kis-Toth K, Kaminski DA, Tsokos GC. Deletion of microRNA-155 reduces autoantibody responses and alleviates lupus-like disease in the Fas(lpr) mouse. Proc Natl Acad Sci U S A. 2013;110:20194–9. https://doi.org/10.1073/pnas.1317632110.
Zhou S, Wang Y, Meng Y, et al. In vivo therapeutic success of MicroRNA-155 Antagomir in a mouse model of lupus alveolar hemorrhage. Arthritis Rheumatol. 2016;68:953–64. https://doi.org/10.1002/art.39485.
Wang M, Chen H, Qiu J, et al. Antagonizing miR-7 suppresses B cell hyperresponsiveness and inhibits lupus development. J Autoimmun. 2020;109:102440. https://doi.org/10.1016/j.jaut.2020.102440.
Yildirim-Toruner C, Diamond B. Current and novel therapeutics in the treatment of systemic lupus erythematosus. J Allergy Clin Immunol. 2011;127:303–12. https://doi.org/10.1016/j.jaci.2010.12.1087.
Acknowledgements
The authors acknowledge Jaypee Institute of Information Technology, Noida, for all the support provided.
Funding
None.
Author information
Authors and Affiliations
Contributions
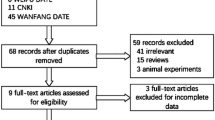
UN, PJ, AS, and PK wrote different aspects of the main manuscript text and prepared tables and figures; RG contributed to conceptualization and reviewing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest has been reported by the authors.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All authors have given consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Naithani, U., Jain, P., Sachan, A. et al. MicroRNA as a potential biomarker for systemic lupus erythematosus: pathogenesis and targeted therapy. Clin Exp Med 23, 4065–4077 (2023). https://doi.org/10.1007/s10238-023-01234-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-01234-7