Abstract
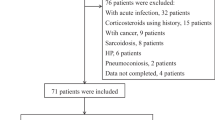
Few biomarkers distinguish connective tissue disease-associated interstitial lung disease (CTD-ILD) from idiopathic pulmonary fibrosis (IPF). Latent transforming growth factor-β binding protein-2 (LTBP2), a secreted extracellular matrix protein, is involved in pulmonary fibrosis. However, the role of LTBP2 in differentially diagnosing CTD-ILD and IPF is unclear. In this study, enzyme-linked immunosorbent assays quantified plasma LTBP2 concentrations in 200 individuals (35 healthy controls, 42 CTD patients without ILD, 89 CTD-ILD patients, and 34 IPF patients). CTD-ILD and IPF were further classified based on chest imaging pattern and pulmonary function test results. Plasma LTBP2 levels were significantly elevated in the IPF group compared with the CTD-ILD group. ROC analysis further suggested the possible value of LTBP2 in differentially diagnosing CTD-ILD and IPF. Additionally, CTD-ILD patients with progressive lung fibrosis had higher plasma LTBP2 concentrations than those who did not. Similarly, patients with IPF developing acute exacerbation showed higher plasma LTBP2 levels than those with stable IPF. This is the first study showing that LTBP2 was closely associated with the usual interstitial pneumonia (UIP) pattern in rheumatoid arthritis-associated ILD (RA-ILD). Moreover, the optimal cutoff values of LTBP2 for distinguishing IPF from CTD-UIP/RA-UIP were 33.75 and 38.33 ng/mL with an AUC of 0.682 and 0.681, respectively. Our findings suggest that plasma LTBP2 levels may differentially diagnose CTD-ILD and IPF, and assess their fibrotic activity. Additionally, clinical LTBP2 evaluation may be a great aid to identifying the presence of the UIP pattern in RA-ILD and to discriminating IPF from CTD-UIP, particularly RA-UIP.




Similar content being viewed by others
References
Travis WD, Costabel U, Hansell DM, et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188(6):733–48. https://doi.org/10.1164/rccm.201308-1483ST.
Wong AW, Ryerson CJ, Guler SA. Progression of fibrosing interstitial lung disease. Respir Res. 2020;21(1):32. https://doi.org/10.1186/s12931-020-1296-3.
Ryerson CJ, Collard HR. Update on the diagnosis and classification of ILD. Curr Opin Pulm Med. 2013;19(5):453–9. https://doi.org/10.1097/MCP.0b013e328363f48d.
Yoo H, Hino T, Hwang J, et al. Connective tissue disease-related interstitial lung disease (CTD-ILD) and interstitial lung abnormality (ILA): evolving concept of CT findings, pathology and management. Eur J Radiol Open. 2022;9: 100419. https://doi.org/10.1016/j.ejro.2022.100419.
Matson S, Lee J, Eickelberg O. Two sides of the same coin? A review of the similarities and differences between idiopathic pulmonary fibrosis and rheumatoid arthritis-associated interstitial lung disease. Eur Respir J. 2021;57(5):2002533. https://doi.org/10.1183/13993003.02533-2020.
Vij R, Strek ME. Diagnosis and treatment of connective tissue disease-associated interstitial lung disease. Chest. 2013;143(3):814–24. https://doi.org/10.1378/chest.12-0741.
Cottin V. Lung biopsy in interstitial lung disease: balancing the risk of surgery and diagnostic uncertainty. Eur Respir J. 2016;48(5):1274–7. https://doi.org/10.1183/13993003.01633-2016.
Martinez FJ, Collard HR, Pardo A, et al. Idiopathic pulmonary fibrosis. Nat Rev Dis Primers. 2017;3:17074. https://doi.org/10.1038/nrdp.2017.74.
Robertson IB, Horiguchi M, Zilberberg L, Dabovic B, Hadjiolova K, Rifkin DB. Latent TGF-β-binding proteins. Matrix Biol. 2015;47:44–53. https://doi.org/10.1016/j.matbio.2015.05.005.
Gibson MA, Hatzinikolas G, Davis EC, Baker E, Sutherland GR, Mecham RP. Bovine latent transforming growth factor beta 1-binding protein 2: molecular cloning, identification of tissue isoforms, and immunolocalization to elastin-associated microfibrils. Mol Cell Biol. 1995;15(12):6932–42. https://doi.org/10.1128/MCB.15.12.6932.
Enomoto Y, Matsushima S, Shibata K, et al. LTBP2 is secreted from lung myofibroblasts and is a potential biomarker for idiopathic pulmonary fibrosis. Clin Sci (Lond). 2018;132(14):1565–80. https://doi.org/10.1042/CS20180435.
Zou M, Zou J, Hu X, Zheng W, Zhang M, Cheng Z. Latent transforming growth factor-β binding protein-2 regulates lung fibroblast-to-myofibroblast differentiation in pulmonary fibrosis via NF-KB signaling. Front Pharmacol. 2021;12:788714. https://doi.org/10.3389/fphar.2021.788714.
Khanna D, Mittoo S, Aggarwal R, et al. Connective tissue disease-associated interstitial lung diseases (CTD-ILD)-report from OMERACT CTD-ILD working group. J Rheumatol. 2015;42(11):2168–71. https://doi.org/10.3899/jrheum.141182.
Raghu G, Remy-Jardin M, Richeldi L, et al. Idiopathic pulmonary fibrosis (an update) and progressive pulmonary fibrosis in adults: an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2022;205(9):e18–47. https://doi.org/10.1164/rccm.202202-0399ST.
Spagnolo P, Distler O, Ryerson CJ, et al. Mechanisms of progressive fibrosis in connective tissue disease (CTD)-associated interstitial lung diseases (ILDs). Ann Rheum Dis. 2021;80(2):143–50. https://doi.org/10.1136/annrheumdis-2020-217230.
Rajan SK, Cottin V, Dhar R, et al. Progressive pulmonary fibrosis: an expert group consensus statement. Eur Respir J. 2023;61(3):2103187. https://doi.org/10.1183/13993003.03187-2021.
Juge PA, Crestani B, Dieudé P. Recent advances in rheumatoid arthritis-associated interstitial lung disease. Curr Opin Pulm Med. 2020;26(5):477–86. https://doi.org/10.1097/MCP.0000000000000710.
Spagnolo P, Lee JS, Sverzellati N, Rossi G, Cottin V. The lung in rheumatoid arthritis: focus on interstitial lung disease. Arthr Rheumatol. 2018;70(10):1544–54. https://doi.org/10.1002/art.40574.
Mei Q, Liu Z, Zuo H, Yang Z, Qu J. Idiopathic pulmonary fibrosis: an update on pathogenesis. Front Pharmacol. 2021;12:797292. https://doi.org/10.3389/fphar.2021.797292.
Pang XF, Lin X, Du JJ, Zeng DY. LTBP2 knockdown by siRNA reverses myocardial oxidative stress injury, fibrosis and remodelling during dilated cardiomyopathy. Acta Physiol (Oxf). 2020;228(3):e13377. https://doi.org/10.1111/apha.13377.
Sideek MA, Teia A, Kopecki Z, Cowin AJ, Gibson MA. Co-localization of LTBP-2 with FGF-2 in fibrotic human keloid and hypertrophic scar. J Mol Histol. 2016;47(1):35–45. https://doi.org/10.1007/s10735-015-9645-0.
Raghu G, Anstrom KJ, King TE Jr, Lasky JA, Martinez FJ. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med. 2012;366(21):1968–77. https://doi.org/10.1056/NEJMoa1113354.
Fischer A, Du Bois R. Interstitial lung disease in connective tissue disorders. Lancet. 2012;380(9842):689–98. https://doi.org/10.1016/S0140-6736(12)61079-4.
Miyazono K, Olofsson A, Colosetti P, Heldin CH. A role of the latent TGF-beta 1-binding protein in the assembly and secretion of TGF-beta 1. EMBO J. 1991;10(5):1091–101. https://doi.org/10.1002/j.1460-2075.1991.tb08049.x.
Collard HR, Ryerson CJ, Corte TJ, et al. Acute exacerbation of idiopathic pulmonary fibrosis: an international working group report. Am J Respir Crit Care Med. 2016;194(3):265–75. https://doi.org/10.1164/rccm.201604-0801CI.
Pache JC, Christakos PG, Gannon DE, Mitchell JJ, Low RB, Leslie KO. Myofibroblasts in diffuse alveolar damage of the lung. Mod Pathol. 1998;11(11):1064–70.
Raghu G, Remy-Jardin M, Myers JL, et al. Diagnosis of idiopathic pulmonary fibrosis: an official ATS/ERS/JRSALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198:44–68. https://doi.org/10.1164/rccm.201807-1255ST.
Samara KD, Trachalaki A, Tsitoura E, et al. Upregulation of citrullination pathway: from autoimmune to idiopathic lung fibrosis. Respir Res. 2017;18(1):218. https://doi.org/10.1186/s12931-017-0692-9.
Acknowledgments
Not applicable.
Funding
This work was supported by funds from the National Natural Science Foundation of China (Grant No: 82070062) and the Climbing Project for Medical Talent of Zhongnan Hospital, Wuhan University (Grant No. PDJH202205).
Author information
Authors and Affiliations
Contributions
ZC, WZ and CW designed this study. MZ, XH, WS, HG, CW, WZ, and ZC collected data and human blood samples. MZ, XH, WS and WZ performed experiments and analyzed the data. MZ and WZ wrote the original manuscript. MZ, XH and WS contributed equally to this study and shared first authorship. ZC, WZ and CW contributed equally to this study.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Human blood samples were obtained under the auspices of the Medical Ethics Committee of Zhongnan Hospital of Wuhan University-approved protocol.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zou, M., Hu, X., Song, W. et al. Plasma LTBP2 as a potential biomarker in differential diagnosis of connective tissue disease-associated interstitial lung disease and idiopathic pulmonary fibrosis: a pilot study. Clin Exp Med 23, 4809–4816 (2023). https://doi.org/10.1007/s10238-023-01214-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-01214-x