Abstract
Introduction
The COVID-19 pandemic exacerbated healthcare needs and caused excess mortality, especially among lower socioeconomic groups. This study describes the emergence of socioeconomic differences along the COVID-19 pathway of testing, healthcare use and mortality in the Netherlands.
Methodology
This retrospective observational Dutch population-based study combined individual-level registry data from June 2020 to December 2020 on personal socioeconomic characteristics, COVID-19 administered tests, test results, general practitioner (GP) consultations, hospital admissions, Intensive Care Unit (ICU) admissions and mortality. For each outcome measure, relative differences between income groups were estimated using log-link binomial regression models. Furthermore, regression models explained socioeconomic differences in COVID-19 mortality by differences in ICU/hospital admissions, test administration and test results.
Results
Among the Dutch population, the lowest income group had a lower test probability (RR = 0.61) and lower risk of testing positive (RR = 0.77) compared to the highest income group. However, among individuals with at least one administered COVID-19 test, the lowest income group had a higher risk of testing positive (RR = 1.40). The likelihood of hospital admissions and ICU admissions were higher for low income groups (RR = 2.11 and RR = 2.46, respectively). The lowest income group had an almost four times higher risk of dying from COVID-19 (RR = 3.85), which could partly be explained by a higher risk of hospitalization and ICU admission, rather than differences in test administration or result.
Discussion
Our findings indicated that socioeconomic differences became more pronounced at each step of the care pathway, culminating to a large gap in mortality. This underlines the need for enhancing social security and well-being policies and incorporation of health equity in pandemic preparedness plans.
Similar content being viewed by others
Introduction
The COVID-19 pandemic impacted many aspects of the health system, pressuring hospital capacity and causing high excess mortality. In 2020, the Netherlands registered more than 20,000 deaths due to COVID-19 [1] and an overall excess mortality of more than 15,000 deaths [2]. Furthermore, over 30,000 individuals were admitted to Dutch hospitals with COVID-19 [3], of which approximately 6500 were admitted to the ICU [4]. This has had a major impact on regular care provision, both in hospitals and primary care [5, 6]. Regular care was postponed, canceled, avoided or provided digitally and waiting times increased [7,8,9]. GPs function as gatekeepers in the Dutch healthcare system. During the COVID-19 pandemic, GPs had to transform and adapt service provision due to a large influx of patients and imposed contact restrictions. Being the first point of contact for patients, GPs experienced a large influx of patients with COVID-19 related complaints and patients whose treatment was postponed in secondary care. Furthermore, impose contact restrictions forced GPs to mainly provide digital care. These changes in primary care increased workload and put pressure on the accessibility and quality of care during the COVID-19 pandemic [10,11,12]. To prevent spread and potential care use related to COVID-19, Municipal Health Services offered free testing in case of COVID-19 related symptoms from June 1st 2020 onwards [13]. Although free of charge, individuals could have experienced barriers for barriers for testing, which included capacity constraints and long waiting times, accessibility of the test location, digital barriers in making appointments and recognizing health symptoms [14]. On the other hand, being free of charge could have induced risky behavior (i.e., moral hazard) and overconsumption of testing.
Socioeconomic Status (SES) disparities in health status, health care utilization and mortality were prominent before the pandemic. Although various definitions and interpretations exists, SES in health research is a multidimensional construct that encompasses individual’s or group’s access to basic resources required to achieve and maintain good health [15]. Among an adult population, SES is often determined by factors such as income, assets or equity, education, occupation and employment, each covering various aspects of SES [16]. Additionally, SES indicators may comprise other sociocultural differences, such as lifestyle, behavioral, cultural, and contextual factors. Regardless of level of healthcare coverage in countries, individuals with lower SES reported poorer health and used on average more care [17, 18]. This association was more ambiguous for previous pandemics and infectious diseases, as it varied by (respiratory) infectious disease whether it affected socioeconomic groups differently [19,20,21,22]. International evidence on socioeconomic differences in COVID-19 infections, utilization and mortality is emerging rapidly [23, 24]. In the Netherlands, preliminary figures show that low education is negatively correlated to test rates for COVID-19 via the Municipal Health Services [25]. Furthermore, low-income individuals had higher risk of dying from COVID-19 [26, 27]. Findings from other European countries with universal healthcare systems consistently showed that lower socioeconomic groups had a higher risk for COVID-19 related hospital admission, ICU admission and mortality than higher socioeconomic groups among the general population, as well as among the population with at least one administered test and confirmed COVID-19 cases [28,29,30,31]. Findings were, however, mixed for positive COVID-19 tests. In the general population, both no differences as well as a lower risk of testing positive for COVID-19 for individuals with lower SES compared with higher SES were found [28,29,30]. For England, Thygesen, Tomlinson, Hollings et al. [32] constructed a COVID-19 care pathway analysis, where care pathways of each individual were followed, including stages of no COVID-19 infection, positive COVID-19 test, primary care COVID-19 diagnosis, hospitalization for COVID-19, ICU admission for COVID-19 and death due to COVID-19. They stratified their analysis, among others, by area index of multiple deprivation (IMD), which is a combined measure of area income, employment, education, health, crime, barriers to housing and services, and living environment [33]. Comparing the lowest and highest area IMD scores, individuals with the lowest IMD score had higher transition rates between most stages, but there were no major differences in elapsed time between stages between lowest and highest area IMD score. When focusing on a hospitalized population, a US and English study showed that lower SES, in terms of median household income or area deprivation index respectively, was associated with higher in-hospital mortality with COVID-19 [34, 35]. The study periods comprised 2020 for the US study and March 1 to May 31, 2020 for the English study. Contrarily, a Scottish study found no differences between Scottish area IMD in mortality among hospitalized patients with COVID-19 during the first wave in 2020 [36].
To date, a comprehensive overview of socioeconomic differences along the COVID-19 care pathway, from testing to mortality, is scarce. The majority of research studies concentrated on a restricted set of outcome measures. We included six consecutive steps in the pathway: administered COVID-19 tests, positive COVID-19 tests, contact with GP for COVID-19, hospital admission for COVID-19, ICU admission for COVID-19 and COVID-19 mortality (Fig. 1). Consequently, the addition of this study to existing literature resides in its comprehensive analysis of the entire care pathway and specifically the inclusion of GP consultations for COVID-19 related health symptoms. Furthermore, most studies employed geographically aggregated data as a proxy for socioeconomic status, as individual level data pertaining to for example income, education and wealth may either be lacking of insufficiently widespread. This study addresses this research gap by utilizing nationwide individual level data encompassing both socioeconomic status and COVID-19 outcome measures. To contribute to the current knowledge base, we aim to answer the following questions:
-
1.
To what extent did COVID-19 related testing, healthcare utilization and mortality differ by socioeconomic groups?
-
2.
To what extent could socioeconomic differences in COVID-19 related mortality be explained by differences in COVID-19 related testing and healthcare utilization?
To answer the first research question, we used binomial regression models with log-link and adjusted step-by-step for age, sex, health status, degree of urbanization of the living environment, household size and country of origin. The second research question will be answered using binomial regression models with log-link and adjusted step-by-step for COVID-19 administered tests, positive tests, hospital admission and ICU admission.
Methodology
Study population and period
The study population included all Dutch residents on January 1, 2020 living in a non-institutionalized household and aged 25–79 years. The study period covered June to December 2020, because all outcomes measures were collectively available during this period. The study therefore covered a period of relatively low infection rates and relaxation of COVID-19 lockdown and other measures (June to October) and the ‘second wave’ of infections with increasing restrictions to a complete lockdown (October to December) [13]. The primary variant of SARS-COV-2 was dominant during this times [37]. In the Netherlands, COVID-19 vaccinations became available from January 2021, therefore the effect of vaccination was not taken into account in this study.
Study design and data sources
This cross-sectional study used pseudonymized routinely collected registry data at the individual level. Individual characteristics, i.e., age, sex, income, education, country of origin, urbanity and household size, from Statistic Netherlands and hospital visits from Vektis (a healthcare business intelligence center who combines and provides declared healthcare data) were linked at individual level to six different types of COVID-19-related outcome measures: administered COVID-19 tests and positive tests from the municipal health services, GP registration data from the Extramural Leiden University Medical Center Academic Network (ELAN), hospital and ICU admissions from Dutch Hospital Data (DHD) and mortality registrations from Statistics Netherlands. Statistics Netherlands functioned as a trusted third party, enabling the linkage between datasets, while ensuring the privacy of the involved individuals, according to Dutch law (Statistics Netherlands Act 2003). An overview of the variables, data sources and population is provided in Table 1.
COVID-19 tests
The number of administered tests for COVID-19 in all Municipal Health Services test locations were available from June 2020 to December 2020. Administered COVID-19 tests and positive test results were binary coded, indicating at least one administered or positive test at the Municipal Health Services, respectively, between June and December 2020.
COVID-19-related GP-consultations
Data from the ELAN network were used to identify COVID-19-related GP consultations [38]. This network includes registrations of about 100 general practitioners in The Hague greater area (5% of the Dutch population), enrolling approximately 300,000 Dutch citizens. Following Sijbom, Büchner, Saadah et al. [39], COVID-19-related GP consultations were identified as consultations with ICPC code R74 or an ICPC code associated with COVID-19-related symptoms together with an indication of COVID-19 in the description (Appendix 1). COVID-19-related GP consultations were coded binary, with score one indicating at least one COVID-19-related GP consultation between June and December 2020.
COVID-19-related hospitalization
DHD provided data on COVID-19-related hospitalizations in nursing wards and ICUs. Hospitalizations related to COVID-19 were identified as hospitalization with ICD-10 codes U07.1 (confirmed COVID-19) or U07.2 (suspected COVID-19) [40]. Due to the structure of the data, it was not possible to distinguish whether a patient had been admitted to the hospital due to health complaints caused by a COVID-19 infection or had been admitted for other health complaints while having COVID-19. COVID-19-related hospital and ICU admissions and were coded binary, indicating at least one admission to the hospital or ICU with COVID-19 respectively between June-December 2020.
COVID-19 mortality
Mortality with COVID-19 (ICD-10 code U07.1) or suspected COVID-19 (ICD-10 code U07.2) was based on the official mortality registry of Statistics Netherlands [41]. This registry uses the primary cause of death as identified by the physician.
Socioeconomic status: income, educational level and financial wealth
We used disposable household income, standardized for household composition [42], as the main indicator for socioeconomic status since household income is most frequently used and arguably the best single indicator of material living standards [16]. To facilitate interpretability, we categorized income level. Income was categorized through a data-driven approach, employing scatterplots to determine the most appropriate cut-off points, thereby resulting into decile categorization. The income deciles were age-standardized, implying that the income decile is based on the income distribution of peers from the same age category (5-year categories for the population aged 25 to 79). This implies that a different income threshold value applied in different age groups to belong, for example, to the lowest income group.
We additionally used educational level [43], lagged income, and financial wealth, derived from tax filings from the Dutch Tax Administration [44], to check for robustness across SES-indicators. These findings are presented in Appendix 3. For educational level, following Statistics Netherlands, the highest level of completed level of education is used and categorized as low (lower vocational educational level, lower secondary educational level or less), middle (intermediate vocational educational level or higher secondary educational level) or high (higher vocational educational level or university). Educational level was missing for a substantial part of the population (38.6%) and missing values were strongly correlated with age. Therefore, a random forest approach, based on data from the representative Dutch Labor Force Survey, was used to impute missing information on educational level. Financial wealth was defined as the difference between households assets and household debts and standardized for household composition. Financial wealth was, using the same approach as for income, categorized in deciles relative to peers in the same 5-year age group.
Covariates
Age, sex, elixhauser comorbidity index, urbanity of living environment, household size and country of origin were included as covariates. These covariates were included because they are known to be associated with income and one or more of the outcome variables [45,46,47,48,49,50,51]. The covariates were maintained across models for consistency. Age was measured on January 1, 2020, and classified into categories to improve interpretability. Applying a data-driven approach to determine the optimal cut-off points, age was categorized into two age categories (25–64 and 65–79) for models with mortality as outcome measure, and three age categories (25–44, 45–64 and 65–79) for models with other outcome measures. The elixhauser comorbidity index is used as a proxy for health status. The elixhauser comorbidity index is operationalized based on prior healthcare use and indicated whether one had one or more hospital visits (both inpatient or outpatient) between 2016 and 2019 for one of the comorbidity listed in the Elixhauser index. This index identifies 30 comorbidities that are associated with substantial increases in length of stay, hospital charges, and mortality [52] and that are closely related to underlying health conditions marked by the Dutch Institute for Public Health and the Environment (RIVM) as risk groups for severe illness from COVID-19 [53]. Primary diagnoses of individual hospital visits from 2016 to 2019 were identified from claims data [54] using algorithms developed during cost-of-illness studies [55] and classified based on the list of Elixhauser ICD-10 codes (Appendix 2). For urbanity six categories were distinguished based on neighborhood address density (0–500 (least urban), 500–1000, 1000–1500, 1500–2500, 2500–5000 or more than 5000 (most urban) addresses per squared kilometer). Household size was defined as a single household, two-person household, three- or four-person household or more than four-person household. Country of origin was defined as Dutch origin, first or second generation of European country origin (excluding the Netherlands) or first or second generation from a non-European country.
Statistical analyses
Descriptive statistics are provided for the study sample of the Dutch population and The Hague greater area population aged 25–79. Socioeconomic differences were estimated per outcome measure for the Dutch population using binomial regression models with log-link to obtain relative risks (RR) of each income decile compared to the highest income decile. For the analysis on GP consultations, the sample was limited to citizens enrolled at one of the participating GP practices. Additionally, the ratio of positive COVID-19 tests was assessed on the Dutch population with at least one administered test and the ratio of COVID-19-related mortality was assessed on the Dutch hospitalized population. All models were fitted using stepwise inclusion of covariates. We decided to use the same covariates for each outcome measure to increase comparability.
-
Model 1: SES (income/education/financial wealth) + age + sex
-
Model 2: Model 1 + Elixhauser comorbidity index
-
Model 3: Model 2 + urbanity + household size + country of origin
Finally, we used multiple logistic regression models to explore to which extent socioeconomic differences in COVID-19 mortality could be explained by differences in hospital admissions, testing behavior and testing results. Here, model 2 was used with COVID-19 mortality as an outcome measure, followed by a stepwise inclusion following the care pathway (administered COVID-19 tests, positive COVID-19 tests, hospital admission for COVID-19 and ICU admission for COVID-19 respectively). GP consultations were not included because they were not available for the entire Dutch population. The fitted models were:
-
Model 4: Model 2 + administered COVID-19 tests
-
Model 5: Model 4 + positive COVID-19 tests
-
Model 6: Model 5 + hospital admissions for COVID-19
-
Model 7: Model 6 + ICU admissions for COVID-19
To test for robustness across SES-indicators, we repeated the analyses using educational attainment, lagged income, and financial wealth instead of income. Confidence intervals (CIs) were set at 95%. Analyses were conducted in R version 4.1.2, using the logbin package [56].
Results
Study population
Data on sex, age, standardized disposable household income, household financial wealth, urbanity and household size were available for 11,447,803 individuals aged 25–79 in the Dutch population (3.9% of individuals excluded due to missing data). 226,959 of these individuals were enrolled at one of the participating GP practices (2.0% of the Dutch population). Table 2 shows the characteristics of both study populations. Approximately half of the Dutch population was female (50.3%) and the mean age was 50.8 (SD 15.0). Three-quarters of the population had a Dutch country of origin, 8% had another European background and 16% had a non-European country of origin. Most individuals lived in a two-person household and in an area with 1500–2500 addresses per km2. Almost half of the population was identified with one or more Elixhauser comorbidities (44.4%).
2% of the full Dutch study population was enrolled at one of the participating GP practices in The Hague greater area. Compared to the full Dutch population, individuals in The Hague greater area that enrolled at participating GP practices had similar age, sex, income, education, financial wealth and Elixhauser comorbidity distribution. Individuals in The Hague greater area did have a non-European country of origin more often, lived in more urban areas, and lived in larger households (Table 2).
aStandardized for household composition relative to peers in the same 5-year age group. Percentages per decile deviate from 10% in The Hague greater area because a subsample of the Dutch population was taken
Descriptive statistics of the outcome measures
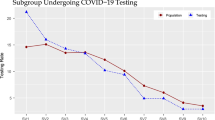
Table 3 shows descriptive information on the six outcome measures among the Dutch population and The Hague greater area. In the Dutch population, 27.7% of the individuals between 25 and 79 years old took at least one COVID-19 test at the Municipality Health Services during the period June 1st to December 31st 2020. This percentage ranged between 17.5% for the lowest income decile and 30.4% for the highest income decile. Furthermore, 3.8% of the Dutch population tested positive for COVID-19. Among the subpopulation living in the Hague greater area, 4.68% consulted the GP for COVID-19-related symptoms. In total, 0.13% in the Dutch population had been admitted to the hospital with COVID-19 or suspicion of COVID-19, of which 18% had been admitted to the ICU. Mortality rates ranged from 0.013% among the highest income decile to 0.059% in the lowest income decile, with an average of 0.026%.
GP consultations among the Hague greater area (n = 226,959). June to December 2020. Frequency in between brackets
Socioeconomic differences in COVID-19-related healthcare use and mortality
Figure 2 shows for each outcome measure the differences between income groups compared to the highest income group (see Appendix 3 for tables with all regression coefficients). Results reported below refer to the relative risk of the lowest income group compared to the highest income group from the fully adjusted model (model 3), unless stated otherwise. Individuals in the lowest income group had a 39% lower risk of at least one administered COVID-19 test (RR = 0.61, 95%CI 0.60–0.61) and in general a 23% lower risk of testing positive for COVID-19 (RR = 0.77, 95%CI 0.76–0.78) compared to individuals in the highest income group. However, among those who took at least one COVID-19 test, individuals in the lowest income group had a 32% higher relative risk of testing positive (RR = 1.32, 95%CI 1.30–1.34). In other words, individuals with lower income were at a population level less likely to test positive for COVID-19 most likely because they tested less often. Middle incomes went to the GP slightly more often with COVID-19-related complaints compared to the highest income group (income decile 6 vs. income decile 10; RR = 1.27, 95%CI 1.17–1.39), however, there was no statistically significant risk difference between the lowest and highest income groups (RR = 1.08, 95%CI 0.98–1.18). Individuals in the lowest income group had a 111% higher risk to be admitted to the hospital ward (RR = 2.11, 95%CI 1.95–2.27), 146% higher risk to be admitted to the ICU (RR = 2.46, 95%CI 2.05–2.95) and 285% higher risk to die with COVID-19 (RR = 3.85, 95%CI 3.21–4.62) compared to individuals in the highest income group. Among hospitalized patients, individuals in the lowest income group had a 81% higher risk to die with COVID-19 (RR = 1.81, 95%CI 1.45–2.25). These relative risk should be interpreted in the context of the small absolute numbers of hospitalization, ICU admission and mortality, as described in Table 3.The addition of covariates (elixhauser comorbidity index, urbanity, household size and country of origin) only marginally explained the association between income groups and differences (models 3 compared to models 1 and 2).
Socioeconomic differences in COVID-19-related testing, healthcare use and mortality. Reference category is income decile 10 (highest income group). Model 1: SES (income) + age + sex; Model 2: Model 1 + elixhauser index; Model 3: Model 2 + urbanity + household size + country of origin (fully adjusted). Analyses with outcomes administered tests, positive tests, hospital admissions, ICU admissions and mortality are analyzed on the Dutch population (N = 11,477,803). GP consultations were analyzed among the Hague greater area (N = 226,959), positive tests among testers was analyzed on the Dutch population with at least one administered test (n = 3,180,218) and mortality among hospitalized was analyzed among the Dutch hospitalized population (n = 15,241). Please note the different x-axis scales
Explaining income differences in COVID-19-related mortality
Figure 3 shows to what extent the higher risk of dying from COVID-19 among lower income groups can be explained by differences in testing and hospital admission (see Appendix 3 for tables with all regression coefficients). Here, model 2 (see also Fig. 2) with COVID-19-related mortality as outcome measure was extended step-by-step with administered COVID-19 tests, positive COVID-19 tests, hospital admission for COVID-19 and ICU admission for COVID-19. The higher risk of dying from COVID-19 among lower income individuals could only partly be explained by differences in hospital admission and ICU admission. After controlling for differences in testing and hospital/ICU admission, individuals in the lowest income group had a 83% higher risk of dying with COVID-19 (RR = 1.83, 95%CI 1.55–2.16, model 7) compared to individuals in the highest income group. Thus, the higher risk of COVID-19 mortality for lower-income individuals could partly be explained by a higher risk of COVID-19 hospitalization or ICU admission and partly by a higher risk of death when being hospitalized. However, income differences in COVID-19 mortality did not change when controlling for testing positive for COVID-19 or having at least one administered COVID-19 test (models 4 and 5). This indicates that differences in testing behavior and test results did not contribute to the observed socioeconomic differences in COVID-19-related mortality.
Education, lagged income, and financial wealth as SES-indicator
Appendix 3 shows the results for financial wealth, lagged income, education and imputed education as a measure of SES. Results are in general consistent with the analysis using income as SES-indicator. The association of financial wealth with hospital admissions, ICU admissions and mortality seems to be slightly stronger compared to income.
Discussion
In this retrospective cross-sectional observational study in the Netherlands, we evaluated socioeconomic differences in each step of the COVID-19 care pathway using individual level registration data. We found that lower income groups had a lower risk of having at least one administered COVID-19 test and testing positive for COVID-19. However, when assessing the risk of testing positive among individuals with at least one administered test, individuals of lower income groups had a higher risk of testing positive. Furthermore, lower income groups had a higher risk of subsequent healthcare use following a (suspicion of) COVID-19 infection, in terms of hospital and ICU admission. We did not observe any differences in COVID-19-related GP consultations between low and high income groups. Lastly, we found that individuals of lower income groups were at higher risk of dying with COVID-19, which could partly be explained by a higher risk of COVID-19 hospitalization or ICU admission and partly by a higher risk of death when being hospitalized. Overall, our findings seems to suggest that socioeconomic disparities became more pronounced at each step of the care pathway.
The contradicting direction of the association between SES and positive COVID-19 tests among the full Dutch population and individuals with at least one administered test may imply that COVID-19 diagnosis may have been under reported among lower income groups. Testing behavior may have concealed differences in infection rates between socioeconomic groups. Hence, the number of positive tests in this study cannot directly be translated to infection rates. Lower testing rates may not been necessarily due to reluctance to test [57], but possibly because of perceived barriers such as accessibility of the test location, digital barriers in making appointments and recognizing health symptoms [14, 58, 59]. On the other hand, it could also be that individuals belonging to higher income groups tested more often than necessary given their symptoms because testing was offered free of charge in the Netherlands during the study period. Because we had no data available on COVID-19-related symptoms during the study period, we cannot conclude whether the differences in testing behavior are due to differences in the occurrence of symptoms, relative underconsumption by individuals belonging to lower income groups, relative overconsumption of individuals belonging to higher income groups, applied testing policies or a combination of these.
Our findings among approximately 200,000 patients from general practitioners in The Hague greater area indicated that individuals belonging to middle income groups were more likely to consult the GP for COVID-19-related complaints than individuals belonging to higher income groups. The risk of consulting a GP for COVID-19-related complaints did not statistically significantly differ between the lowest and highest income groups. To our knowledge, no research has evaluated socioeconomic differences in GP- visits for COVID-19 or COVID-19-related symptoms. In the primary care setting, literature focused mainly on disrupted care, e.g., for chronic diseases or cancer diagnosis [7], and the emergence and uptake of teleconsulting [8]. In addition, the pattern of middle incomes being more likely to visit a GP, but higher incomes not differing from lower incomes, is inconsistent with previous findings of pre-pandemic GP visits in the Netherlands [17]. Due to the inherent limitations of the study design and use of registration data, we could not determine whether these outcomes stemmed from a different consumption pattern in Covid than for other conditions, underconsumption by low income groups during the COVID-19 pandemic, or overconsumption by higher income groups. Alternatively, income differences in COVID-19 incidence and severity may be partly driven by having a non-Dutch country of origin [60]. The lowest income groups in the Hague greater area may have a greater share of individuals with a non-Dutch country of origin, which may affect comparability between findings in the Dutch population and the Hague greater area.
Furthermore, among the full Dutch population, we found that individuals belonging to lower income groups were at higher risk for being admitted to the hospital and ICU compared to individuals belonging to higher income groups in the general population. It could be reasoned that a more severe disease course among lower socioeconomic groups could be driven by poorer pre-pandemic health status and more comorbidities, which is widely shown for non-COVID-19 healthcare use and mortality [17, 18]. Our results indicated, however, that the elixhauser comorbidity index could not explain income differences in COVID-19 hospital and ICU admission. Possibly, the elixhauser comorbidity index, based on prior hospital visits, inadequately proxies health status or inadequately captures income differences in health status. The finding that individuals belonging to lower income groups were at greater risk of serious COVID-19 illness, even after controlling for a poorer pre-pandemic health status, is consistent with findings from Spain [61] and Switzerland [28]. However, other studies showed that the association between income and COVID-19 hospitalization may be dependent on study period and included confounders. In Sweden, income was not associated with COVID-19 hospitalization in the first six months of the pandemic [30] but in another Swedish study negatively associated in the period March 2020 to March 2022 [62]. In Finland and England, lower income groups had a higher risk of hospitalization for COVID-19, but this difference did attenuate when controlling for risk factors, among others comorbidities [60, 63]. In addition, other unidentified factors might have contributed to the higher risk of hospital and ICU admission among lower income groups. For example, differences in lifestyle factors by SES, such as BMI, smoking and physical activity [64, 65] may have played a significant role in the disease course [66], which was not captured adequately by pre-pandemic healthcare use or any other covariate used.
Lastly, we found that individuals belonging to lower income groups were at higher risk for dying with COVID-19, which is consisted with findings from other European countries, such as Sweden [67] and Switzerland [28]. They are also comparable to findings from the first wave (March–June, 2020) in the Netherlands, as Stoeldraijer et al. [26] indicated that the lowest income quintile had a three times higher risk of COVID-19 mortality compared to the highest income quintile. Wouterse et al. [27] showed that income differences in all-cause mortality was larger than predicted during the pandemic in the Netherland. Although income differences in non-COVID mortality were smaller than predicted, the income differences COVID-19 mortality drove the larger differences in all-cause mortality. Therefore, they argue that the COVID-19 pandemic has enlarged already existing income differences in mortality in the Netherlands. Similar to hospital and ICU admission, higher mortality rates may result from a higher infection rate and/or a more severe disease course. However, no support was found for these mechanisms, possibly due to the study’s limitations. The question then still remains: what could explain the higher COVID-19 mortality rates among lower socio-economic groups? In our study, we found that income difference in COVID-19-related mortality risk decreased when taking into account differences in hospital and ICU admissions for COVID-19, indicating that the differences in hospitalization could partly, but not entirely, explain why individuals belonging to lower income groups were more likely to die with COVID-19. Among hospitalized patients, individuals belonging to lower income groups retained a higher COVID-19 mortality risk. Differences in testing behavior and test results did not contributed to the observed higher risk of dying with COVID-19 among lower income groups.
Strengths and limitations
The strength of this study lies in the assessment of the entire care pathway, from testing to mortality, while other studies only looked at testing, hospitalization and mortality as single outcome measures. We were thus able to provide a comprehensive overview of the emergence of socioeconomic differences along the care pathway. This study is, to our knowledge, the first to gain insights into socioeconomic differences in COVID-19-related GP consultations. In addition, this study was based on population-wide individual level registration data, which eliminated any selection or recall biases.
Our research was also subjected to some limitations. The sample from The Hague greater area, used to analyze the GP consultations, covered approximately 2% of the Dutch population. While the subsample was representative on outcome measures and SES indicators, a higher degree of urbanity could skew the results towards higher SES differences in GP consultations. To reduce bias, we correct for degree of urbanity, household size, and country of origin in all regression analyses. Because of the small probability of ICU admission and mortality, the sample was too small to perform advanced analyses and incorporate GP consultations into the model explaining socioeconomic differences in COVID-19 mortality. Another limiting factor is that the COVID-19 test dataset did not contain administered and positive tests at commercial test centers and tests performed by employers and healthcare facilities. Some employers organized test facilities for their employees, which was for example common for healthcare workers. Commercial test centers emerged due to capacity constraints at the test centers from the municipal health services, and charged costs for administering a COVID-19 test. There is no insight into the total number of tests conducted by parties other than the Municipal Health Services. Journalism research claimed that at peak about one-third of the tests were conducted by commercial parties [68]. Due to the costs of testing at commercial test centers, it is to be expected that higher income individuals were more likely to test at commercial test centers, which would underestimate differences in COVID-19 testing based on SES. Furthermore, due to the use of registration data, it was not possible to identify whether COVID-19 was the primary cause for hospitalization or mortality, or whether it was a comorbidity to other health complaints. In the case of pre-existing life-threatening illnesses or old age combined with a COVID-19 infection, the registered cause of death depends on the physician's assessment [69]. Multi-cause mortality may cause errors in registration of actual COVID-19 mortality, but this bias is likely equally distributed among SES-groups. Lastly, inclusion of outcome indicators reflecting the entire healthcare pathway limited us in longitudinal data availability, with total overlap in data availability only covering eight months. This period includes the low-infectivity period in summer 2020 and ends at the height of the winter resurgence in 2021. While that provides a realistic representation of the pandemic, additional longitudinal data are needed to assess potential changes in SES-mediated outcome differences over the course of the pandemic.
Conclusions, policy implications and further research
The COVID-19 pandemic had major consequences for the entire Dutch population, but individuals with lower pre-pandemic socioeconomic status experienced significantly higher risks of COVID-19 hospitalization and mortality. The socioeconomic differences became more pronounced at each step of the care pathway, culminating to a large gap in mortality rates. These findings indicated that existing socioeconomic differences were reflected in an unequal distribution of the burden of a new communicable disease. As SES-differences in testing behavior and test results did not contribute to SES-differences in mortality, it may be especially important to improve the starting position of lower SES-groups. Policy aimed at social security and well-being may, therefore, also contribute to reduced vulnerability of lower SES-groups in a crisis situation such as the COVID-19 pandemic, the utilization of health potential and prevention or worsening of illness. Furthermore, infection prevention may be particularly valuable in lower SES-groups as they were at higher risk to experience a more severe disease course.
The descriptive analyses in this research did not explain why individuals belonging to lower income groups had a higher risk of COVID-19 hospitalization and mortality. Even though previous studies have often shown that individuals belonging to lower income groups generally used more healthcare and had a higher mortality risk because they were in poorer health, socioeconomic differences in COVID-19 hospitalization and mortality did not decrease in our study when accounting for a proxy of pre-pandemic health status. Therefore, more research is needed specifically on the contribution of health status to SES-differences in COVID-19 hospitalization and mortality and to what extent health promotion can contribute to reducing these differences. Future research into other causal mechanisms underlying these trends, such as lifestyle, behavioral, cultural, and contextual factors could inform policy makers on the extent that socioeconomic differences could have been prevented in each step of the care pathway. The dynamics in individual care pathways, e.g., using individual regression lines, could also provide additional insight. This way important lessons can be retrieved about mechanism driving the unequal distribution of the burden of a new communicable disease among socioeconomic groups. These insights will be beneficial to take equity into account in pandemic preparedness plans currently being developed.
Data availability
Results are based on non-public microdata from Statistics Netherlands. Under certain conditions, these microdata are accessible for statistical and scientific research.
References
StatLine C. Overledenen; doodsoorzaak (uitgebreide lijst), leeftijd, geslacht. In: StatLine C (eds.) (2022).
Centraal Bureau voor de Statistiek. Bijna 169 duizend mensen overleden in 2020, 10 procent meer dan verwacht 2021. https://www.cbs.nl/nl-nl/nieuws/2021/04/bijna-169-duizend-mensen-overleden-in-2020-10-procent-meer-dan-verwacht.
Centraal Bureau voor de Statistiek. In 2020 bijna 230 duizend minder mensen opgenomen in het ziekenhuis 2022. https://www.cbs.nl/nl-nl/nieuws/2022/24/in-2020-bijna-230-duizend-minder-mensen-opgenomen-in-het-ziekenhuis.
Dutch National Institute for Public Health and the Environment. Covid-19 Intensive care-opnames (IC) in Nederland per ic-opnamedatum en meldingsdatum (volgens NICE registratie). In: Dutch National Institute for Public Health and the Environment (eds.) (2022).
de Wit, G., Oosterhoff, M., Kouwenberg, L., et al.: De gezondheidsgevolgen van uitgestelde operaties tijdens de corona-pandemie. Schattingen voor 2020 en 2021. The health consequences of surgical procedures postponed during the coronavirus pandemic Estimates for 2020 and 2021: Rijksinstituut voor Volksgezondheid en Milieu. (2022).
Jansen, T., Gouwens, S., Meijerink, L., et al.: Disruption of hospital care during the first year of the COVID-19 pandemic impacted socioeconomic groups differently: population based study using routine registration data [Manuscript submitted for publication]. (2023).
Lambooij, M., Heins, M., Meijer, M., et al.: Het mijden van huisartsenzorg tijdens de coronapandemie. Inzicht in verminderde huisartsenzorg tijdens de coronapandemie. Avoiding GP care during the coronavirus pandemic insight in reduction of GP care during the coronavirus pandemic: Rijksinstituut voor Volksgezondheid en Milieu RIVM. (2022).
Ndayishimiye, C., Lopes, H., Middleton, J.: A systematic scoping review of digital health technologies during COVID-19: a new normal in primary health care delivery. Health Technol. 13, 273–284 (2023)
van Giessen, A., de Wit, A., van den Brink, C., et al.: Impact van de eerste COVID-19 golf op de reguliere zorg en gezondheid : Inventarisatie van de omvang van het probleem en eerste schatting van gezondheidseffecten. Impact of the first wave of COVID-19 on regular healthcare and health: Assessment of the extent of the problem and first estimation of the health effects: Rijksinstituut voor Volksgezondheid en Milieu RIVM. (2020).
Rotteveel, A., van Vliet, E., Keuper, J., et al.: De impact van de coronapandemie op de huisartsenzorg – ervaringen van en geleerde lessen door huisartsen. Impact of the coronavirus pandemic on the provision of GP care: experiences and lessons learned in general practice: Rijksinstituut voor Volksgezondheid en Milieu RIVM. (2023).
Wanat, M., Hoste, M., Gobat, N., et al.: Transformation of primary care during the COVID-19 pandemic: experiences of healthcare professionals in eight European countries. Br. J. Gen. Pract. 71(709), e634–e642 (2021)
Groenewegen, P., van den Muijsenbergh, M., Batenburg, R., et al.: Snelle aanpassing praktijkorganisatie tijdens de coronapandemie. Huisarts en wetenschap. 65(5), 16–20 (2022)
Rijksoverheid. Ontwikkelingen coronavirus in 2020 (2023). https://www.rijksoverheid.nl/onderwerpen/coronavirus-tijdlijn/2020.
Zomer, C., Plantinga, L., Kroese, F.: Testen op corona tijdens de pandemie door mensen met een lager inkomen. RIVM, (2023).
Shavers, V.L.: Measurement of socioeconomic status in health disparities research. J. Natl. Med. Assoc. 99(9), 1013–1023 (2007)
Galobardes, B., Shaw, M., Lawlor, D.A., et al.: Indicators of socioeconomic position (part 1). J. Epidemiol. Community Health 60(1), 7 (2006)
Loef, B., Meulman, I., Herber, G.-C.M., et al.: Socioeconomic differences in healthcare expenditure and utilization in The Netherlands. BMC Health Serv. Res. 21(1), 643 (2021)
Mackenbach, J.P., Stirbu, I., Roskam, A.-J.R., et al.: Socioeconomic inequalities in health in 22 European countries. N. Engl. J. Med. 358(23), 2468–2481 (2008)
Pini, A., Stenbeck, M., Galanis, I., et al.: Socioeconomic disparities associated with 29 common infectious diseases in Sweden, 2005–14: an individually matched case-control study. Lancet Infect. Dis.Infect. Dis 19(2), 165–176 (2019)
Baker, M.G., Barnard, L.T., Kvalsvig, A., et al.: Increasing incidence of serious infectious diseases and inequalities in New Zealand: a national epidemiological study. The Lancet. 379(9821), 1112–1119 (2012)
Bengtsson, T., Dribe, M., Eriksson, B.: Social Class and Excess Mortality in Sweden During the 1918 Influenza Pandemic. Am. J. Epidemiol. 187(12), 2568–2576 (2018)
de Gier, B., Houben-van Herten, M., Uiters, E., et al.: Educational differences in acute infectious diseases in the Netherlands: results from a nationwide health survey. Eur. J. Public Health 30(2), 270–275 (2020)
Wachtler, B., Michalski, N., Nowossadeck, E., et al.: Socioeconomic inequalities and COVID-19—a review of the current international literature. J. Health Monit. 5(S7), 3–17 (2020)
Khanijahani, A., Iezadi, S., Gholipour, K., et al.: A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. Int. J. Equity Health. 20(1), 248 (2021)
Centraal Bureau voor de Statistiek. GGD-testdata: 6,7 miljoen mensen deden minstens één coronatest (2021) https://www.cbs.nl/nl-nl/nieuws/2021/25/ggd-testdata-6-7-miljoen-mensen-deden-minstens-een-coronatest.
Stoeldraijer, L., Kunst, A. E., Chilunga, F., et al.: Sociaal-demografische verschillen in COVID-19-sterfte in het eerste jaar van de coronapandemie. Centraal Bureau voor de Statistiek, (2022).
Wouterse, B., Geisler, J., Bär, M., et al.: Has COVID-19 increased inequality in mortality by income in the Netherlands? J. Epidemiol. Community Health (2023). https://doi.org/10.1136/jech-2022-219845
Riou, J., Panczak, R., Althaus, C.L., et al.: Socioeconomic position and the COVID-19 care cascade from testing to mortality in Switzerland: a population-based analysis. Lancet Public Health. 6(9), e683–e691 (2021)
Fernández-Martínez, N.F., Ruiz-Montero, R., Gómez-Barroso, D., et al.: Socioeconomic differences in COVID-19 infection, hospitalisation and mortality in urban areas in a region in the South of Europe. BMC Public Health 22(1), 2316 (2022)
Bergman, J., Ballin, M., Nordström, A., et al.: Risk factors for COVID-19 diagnosis, hospitalization, and subsequent all-cause mortality in Sweden: a nationwide study. Eur. J. Epidemiol. 36(3), 287–298 (2021)
Gustafsson, P.E., San Sebastian, M., Fonseca-Rodriguez, O., et al.: Inequitable impact of infection: social gradients in severe COVID-19 outcomes among all confirmed SARS-CoV-2 cases during the first pandemic wave in Sweden. J. Epidemiol. Community Health 76(3), 261 (2022)
Thygesen, J.H., Tomlinson, C., Hollings, S., et al.: COVID-19 trajectories among 57 million adults in England: a cohort study using electronic health records. Lancet Digit Health. 4(7), e542–e557 (2022)
UK Government. English indices of deprivation 2019 (2019) https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019.
Isath, A., Malik, A.H., Goel, A., et al.: Nationwide analysis of the outcomes and mortality of hospitalized COVID-19 patients. Curr. Probl. Cardiol.Probl. Cardiol. 48(2), 101440 (2023)
Navaratnam, A.V., Gray, W.K., Day, J., et al.: Patient factors and temporal trends associated with COVID-19 in-hospital mortality in England: an observational study using administrative data. Lancet Respir. Med. 9(4), 397–406 (2021)
Khan, K.S., Torpiano, G., McLellan, M., et al.: The impact of socioeconomic status on 30-day mortality in hospitalized patients with COVID-19 infection. J. Med. Virol. 93(2), 995–1001 (2021)
Rijksinstituut voor Volksgezondheid en Milieu. Varianten van het coronavirus SARS-CoV-2 (2023) https://www.rivm.nl/coronavirus-covid-19/virus/varianten.
Ardesch, F.H., Meulendijk, M.C., Kist, J.M., et al.: A data-driven population health management approach: The Extramural LUMC Academic Network data infrastructure. Health Policy 132, 104769 (2023)
Sijbom, M., Büchner, F.L., Saadah, N.H., et al.: Comparing antibiotic prescriptions in primary care between SARS-CoV-2 and influenza: a retrospective observational study. BJGP Open. 6(4), BJGPO.2022.0049 (2022)
World Health Organisation. ICD-10 Version:2019 (2019) https://icd.who.int/browse10/2019/en.
Centraal Bureau voor de Statistiek. Documentatie Doodsoorzaken van personen die bij overlijden inwoners waren van Nederland (DOODOORZTAB). (2022).
Centraal Bureau voor de Statistiek. Documentatie Inkomen van huishoudens (INHATAB) (2021).
Centraal Bureau voor de Statistiek. Documentatie Hoogst behaald en hoogst gevolgd opleidingsniveau en opleidingsrichting van de bevolking in Nederland (HOOGSTEOPLTAB). (2022).
Centraal Bureau voor de Statistiek. Documentatie Vermogens van huishoudens (VEHTAB). (2022).
Coyer, L., Boyd, A., Schinkel, J., et al.: Differences in SARS-CoV-2 infections during the first and second wave of SARS-CoV-2 between six ethnic groups in Amsterdam, the Netherlands: a population-based longitudinal serological study. Lancet Reg. Health Eur. 13, 100284 (2022)
Ahrenfeldt, L.J., Otavova, M., Christensen, K., et al.: Sex and age differences in COVID-19 mortality in Europe. Wien. Klin. Wochenschr.Klin. Wochenschr. 133(7), 393–398 (2021)
Li, X., Zhong, X., Wang, Y., et al.: Clinical determinants of the severity of COVID-19: a systematic review and meta-analysis. PLoS ONE 16(5), e0250602 (2021)
Martin, C.A., Jenkins, D.R., Minhas, J.S., et al.: Socio-demographic heterogeneity in the prevalence of COVID-19 during lockdown is associated with ethnicity and household size: Results from an observational cohort study. EClinicalMedicine. 25, 100466 (2020)
Boterman, W.: Population density and SARS-CoV-2 pandemic: comparing the geography of different waves in the Netherlands. Urban Stud. 60(8), 1377–1402 (2022)
StatLine C. Inkomen van personen; persoonskenmerken, regio (indeling 2021) (2021) https://opendata.cbs.nl/#/CBS/nl/dataset/85065NED/table?dl=5CC3F.
VZinfo.nl. Gezondheidsverschillen in ziekten en aandoeningen (2023) https://www.vzinfo.nl/gezondheidsverschillen/ziekten-aandoeningen.
Elixhauser, A., Steiner, C., Harris, D.R., et al.: Comorbidity measures for use with administrative data. Med. Care 36(1), 8–27 (1998)
Dutch National Institute for Public Health and the Environment. Risk groups and COVID-19 (2022) https://www.rivm.nl/en/coronavirus-covid-19/risk-groups.
Centraal Bureau voor de Statistiek. Documentatie Geopende Diagnose Behandeling Combinatie prestaties in de Medisch Specialistische Zorg (MSZPrestatiesVEKTTAB). (2022).
Rijksinstituut voor Volksgezondheid en Milieu. Kosten van ziekten 2022 (Accessed 11 Aug 2022) https://www.vzinfo.nl/kosten-van-ziekten.
Donoghoe, M.W., Marschner, I.C.: logbin: an R package for relative risk regression using the log-binomial model. J. Stat. Softw. 86(9), 1–22 (2018)
Thunström, L., Ashworth, M., Shogren, J.F., et al.: Testing for COVID-19: willful ignorance or selfless behavior? Behav. Public Policy. 5(2), 135–152 (2021)
Perry, B.L., Aronson, B., Railey, A.F., et al.: If you build it, will they come? Social, economic, and psychological determinants of COVID-19 testing decisions. PLoS ONE 16(7), e0252658 (2021)
Bevan, I., Stage Baxter, M., Stagg, H.R., et al.: Knowledge, attitudes, and behavior related to COVID-19 testing: a rapid scoping review. Diagnostics. 11(9), 1685 (2021)
Saarinen, S., Moustgaard, H., Remes, H., et al.: Income differences in COVID-19 incidence and severity in Finland among people with foreign and native background: a population-based cohort study of individuals nested within households. PLoS Med. 19(8), e1004038 (2022)
Castilla, J., Guevara, M., Miqueleiz, A., et al.: Risk factors of infection, hospitalization and death from SARS-CoV-2: a population-based cohort study. J. Clin. Med. 10(12), 2608 (2021)
Bell, M., Hergens, M.-P., Fors, S., et al.: Individual and neighborhood risk factors of hospital admission and death during the COVID-19 pandemic: a population-based cohort study. BMC Med. 21(1), 1 (2023)
Patel, A.P., Paranjpe, M.D., Kathiresan, N.P., et al.: Race, socioeconomic deprivation, and hospitalization for COVID-19 in English participants of a national biobank. Int. J. Equity Health. 19(1), 114 (2020)
Nagelhout, G.E., de Korte-de Boer, D., Kunst, A.E., et al.: Trends in socioeconomic inequalities in smoking prevalence, consumption, initiation, and cessation between 2001 and 2008 in the Netherlands. Findings from a national population survey. BMC Public Health 12(1), 303 (2012)
Proper, K.I., Cerin, E., Brown, W.J., et al.: Sitting time and socio-economic differences in overweight and obesity. Int. J. Obes. 31(1), 169–176 (2007)
Méjean, C., Droomers, M., van der Schouw, Y.T., et al.: The contribution of diet and lifestyle to socioeconomic inequalities in cardiovascular morbidity and mortality. Int. J. Cardiol. 168(6), 5190–5195 (2013)
Drefahl, S., Wallace, M., Mussino, E., et al.: A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden. Nat. Commun. 11(1), 5097 (2020)
van der Heyden, W., Schram, P.: Ruim een derde van alle coronatests niet door GGD, maar particulier: 'We verliezen het zicht op het virus'. EenVandaag. (2020).
Centraal Bureau voor de Statistiek. Bijna 3,2 duizend mensen overleden aan COVID-19 in november 2020 (2021) https://www.cbs.nl/nl-nl/nieuws/2021/10/bijna-3-2-duizend-mensen-overleden-aan-covid-19-in-november-2020.
Acknowledgements
We acknowledge Marie Buijs, Lotta Meijerink and Sigur Gouwens for their contribution to data processing. This study was funded by the Strategic Program project “Societal” of the Dutch National Institute for Public Health and the Environment (RIVM). The funding source had no involvement in the study design; in the collection, analysis and interpretation of data; in the writing of the articles; and in the decision to submit it for publication.
Author information
Authors and Affiliations
Contributions
IM: conceptualization, formal analysis, writing—original draft. EU, NS: conceptualization, supervision, writing—review and editing. MC, JS, JP: writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Meulman, I., Uiters, E., Cloin, M. et al. From test to rest: evaluating socioeconomic differences along the COVID-19 care pathway in the Netherlands. Eur J Health Econ (2024). https://doi.org/10.1007/s10198-024-01680-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10198-024-01680-4