Abstract
Only few studies outside of the US have addressed the issue of out-of-pocket payments (OOP) at the end of life because of a lack of data. We use an exclusive dataset from a major French health insurance company (MGEN), including claim data, both mandatory and voluntary health insurance details, income and individual characteristics, for individuals aged 65 or older who died in 2017. We address three main issues: (1) What is the magnitude of OOP in France at the end of life? (2) How are OOP distributed, and do they present a financial risk to patients? (3) What are the determinants of OOP and what health system reforms could reduce them? Our results indicate that OOP expenses increase in the last year of life and accelerate in the last trimester. Despite some outliers, the French system is successful in protecting individuals from catastrophic OOP. Using generalised linear models, we confirm that improving the pathways of care could generate savings and partially reduce households’ financial burden. However, OOP are elastic to income and driven essentially by personal convenience demands. Using concentration curves and Gini coefficients, we show that providing additional insurance against end-of-life OOP would likely be regressive, i.e., socially non-desirable.

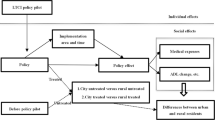
Source: Éracles, year 2017

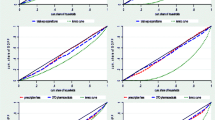
Source: Éracles, year 2017
Similar content being viewed by others

Notes
For instance, according to Kelley et al. [13], health expenses and OOP vary according to the cause of death, indicating a financial risk of inequality in the face of death. They find that for Medicare enrolees, the average OOP is highest for dementia (81% more than other patients) and lowest for patients who died of heart disease or cancer.
References
Kolodziejczyk, C.: The effect of time to death on health care expenditures: taking into account the endogeneity and right censoring of time to death. Eur. J. Health Econ. 21, 945–962 (2020)
French, E.B., McCauley, J., Aragon, M., Bakx, P., Chalkley, M., Chen, S.H., et al.: End-of-life medical spending in last twelve months of life is lower than previously reported. Health Aff. 36(7), 1211–1217 (2017). https://doi.org/10.1377/hlthaff.2017.0174
Cooper, Z., Craig, S.V., Gaynor, M., Van Reen, J.: The price ain’t right? Hospital prices and health spending on the privately insured. Q. J. Econ. 134(1), 51–107 (2019). https://doi.org/10.1093/qje/qjy020
Davis, M.A., Nallamothu, B.K., Banerjee, M., Bynum, J.P.: Identification of four unique spending patterns among older adults in the last year of life challenges standard assumptions. Health Aff. 35(7), 1316–1323 (2016). https://doi.org/10.1377/hlthaff.2015.1419
Emanuel, E.J., Emanuel, L.L.: The economics of dying–the illusion of cost savings at the end of life. N. Engl. J. Med. 330(8), 540–544 (1994)
Wagstaff, A., van Doorslaer, E.: Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993–1998. Health Econ. 12(11), 921–934 (2003). https://doi.org/10.1002/hec.776
Liu, Y., Rao, K., Hsiao, W. C.: Medical expenditure and rural impoverishment in China. J. Health Popul. Nutr. 216–222 (2003)
Pannarunothai, S., Mills, A.: The poor pay more: health-related inequality in Thailand. Soc. Sci. Med. 44(12), 1781–1790 (1997). https://doi.org/10.1016/S0277-9536(96)00287-0
McGarry, K., Schoeni, R.F.: Widow(er) poverty and out-of-pocket medical expenditures near the end of life. J. Gerontol. B Psychol. Sci. Soc. Sci. 60(3), S160–S168 (2005). https://doi.org/10.1093/geronb/60.3.S160
Riley, G.F., Lubitz, J.D.: Long-term trends in Medicare payments in the last year of life. Health Serv. Res. 45(2), 565–576 (2010). https://doi.org/10.1111/j.1475-6773.2010.01082.x
Paris, V., Hewlett, E., Auraaen, A., Alexa, J., Simon, L.: Health care coverage in OECD countries in 2012. (2016). https://doi.org/10.1787/5jlz3kbf7pzv-en
Kelley, A.S., McGarry, K., Fahle, S., Marshall, S.M., Du, Q., Skinner, J.S.: Out-of-pocket spending in the last five years of life. J. Gen. Intern. Med. 28, 304–309 (2013). https://doi.org/10.1007/s11606-012-2199-x
Kelly, A.S., McGarry, K., Gorges, R., Skinner, J.: The burden of healthcare costs for patients with dementia in the last five years of life. Ann. Intern. Med 163, 729–736 (2015). https://doi.org/10.7326/M15-0381
Narang, A.K., Nicholas, L.H.: Out-of-pocket spending and financial burden among medicare beneficiaries with cancer. JAMA Oncol. 3(6), 757–765 (2017). https://doi.org/10.1001/jamaoncol.2016.4865
Kominski, G.F., Nonzee, N.J., Sorensen, A.: The Affordable Care Act’s impacts on access to insurance and health care for low-income populations. Annu. Rev. Public Health 38, 489–505 (2017). https://doi.org/10.1146/annurev-publhealth-031816-044555
Orlovic, M., Marti, J., Mossialos, E.: Analysis of end-of-life care, out-of-pocket spending, and place of death in 16 European countries and Israel. Health Aff. 36(7), 1201–1210 (2017). https://doi.org/10.1377/hlthaff.2017.0166
Penders, Y.W., Rietjens, J., Albers, G., Croezen, S., Van den Block, L.: Differences in out-of-pocket costs of healthcare in the last year of life of older people in 13 European countries. Palliat. Med. 31(1), 42–52 (2017). https://doi.org/10.1177/0269216316647206
Dutton, P.V.: Differential diagnoses: A comparative history of health care problems and solutions in the United States and France. Cornell University Press (2012)
Lardellier, R., Legal, R., Raynaud, D., Vidal, G.: Un outil pour l’étude des dépenses de santé et des «restes à charge» des ménages: le modèle Omar. Économie et Statistique 450(1), 47–77 (2011)
Finkelstein, A., McKnight, R.: What did Medicare do? The initial impact of Medicare on mortality and out of pocket medical spending. J. Public Econ. 92(7), 1644–1668 (2008)
Finkelstein, A., Taubman, S., Wright, B., Bernstein, M., Gruber, J., Newhouse, J.P., Oregon Health Study Group: The Oregon health insurance experiment: evidence from the first year. Q. J. Econ. 127(3), 1057–1106 (2012). https://doi.org/10.1016/j.jpubeco.2007.10.005
Rodwin, V.G.: The health care system under French national health insurance: lessons for health reform in the United States. Am. J. Public Health 93(1), 31–37 (2003). https://doi.org/10.2105/AJPH.93.1.31
Buchmueller, T., Couffinhal, A.: Private Health Insurance in France. OCDE Health Working Papers, no 12, OCDE, Paris (2004). https://doi.org/10.1787/555485381821
Nay, O., Béjean, S., Benamouzig, D., Bergeron, H., Castel, P., Ventelou, B.: Achieving universal health coverage in France: policy reforms and the challenge of inequalities. Lancet 387(10034), 2236–2249 (2016). https://doi.org/10.1016/S0140-6736(16)00580-8
Fourcade, N., von Lennep, F., Grémy, I., Bourdillon, F., Luciano, L., Rey, S., et al.: M.: L’état de santé de la population en France-RAPPORT 2017 (2017)
Montaut, A.: La généralisation de la complémentaire santé d’entreprise a peu fait évoluer le marché en 2016. Etudes et résultats 1064, 1–6 (2018)
Murray Scott, A., Aziz, K.M.K.: Illness trajectories and palliative care. BMJ (Clinical Research Ed) 330, 1007–1011 (2005). https://doi.org/10.1136/bmj.330.7498.1007
Pennec, S., Gaymu, J., Monnier, A., Riou, F., Aubry, R., Pontone, S., Cases, C.: Le dernier mois de l’existence : les lieux de fin de vie et de décès en France. Population, 68(4), 585–615 (2013). https://doi.org/10.3917/popu.1304.0585
Pradhan, M., Prescott, N.: Social risk management options for medical care in Indonesia. Health Econ. 11(5), 431–446 (2002). https://doi.org/10.1002/hec.689
Ranson, M.K.: Reduction of catastrophic health care expenditures by a community-based health insurance scheme in Gujarat, India: current experiences and challenges. Bull. World Health Organ. 80, 613–621 (2002)
Buigut, S., Ettarh, R., Amendah, D.D.: Catastrophic health expenditure and its determinants in Kenya slum communities. Int. J. Equity Health 14(1), 46 (2015). https://doi.org/10.1186/s12939-015-0168-9
Jones, A.M.: Models for health care. University of York., Centre for Health Economics (2010)
Papon, S.: Les décès en 2017. Insee Résultats. 128 (2018)
Gerfin, M., Kaiser, B., Schmid, C.: Healthcare demand in the presence of discrete price changes. Health Econ. 24(9), 1164–1177 (2015). https://doi.org/10.1002/hec.3154
Zweifel, P., Felder, S., Meiers, M.: Ageing of population and health care expenditure: a red herring? Health Econ. 8(6), 485–496 (1999). https://doi.org/10.1002/(SICI)1099-1050(199909)8:6%3c485::AID-HEC461%3e3.0.CO;2-4
Reynaud, M., Butor, L., Foucaud, D., Bonnevide, P.: Haut conseil pour l’avenir de l’assurance maladie 2013. Rapport Annuel. 273 (2014)
Chowdhury, S., Gupta, I., Trivedi, M., Prinja, S.: Inequity and burden of out-of-pocket health spending: district level evidences from India. Indian J. Med. Res. 148(2), 180 (2018). https://doi.org/10.4103/ijmr.IJMR_90_17
del Pozo-Rubio, R., Jiménez-Rubio, D.: Catastrophic risk associated with out-of-pocket payments for long term care in Spain. Health Policy 123(6), 582–589 (2019). https://doi.org/10.1016/j.healthpol.2019.03.016
Dourgnon P., Evrard I., Guillaume S.: Towards an Information System on Health Care Costs, Public and Complementary Health Insurance Reimbursements, and Out-of-pocket Payments. QES 194, IRDES, Paris (2014)
Acknowledgements
We thank Carine Franc from the French National Institute for Health and Medical Research (INSERM), the participants of the 41st JESF and 68th AFSE annual meetings and two anonymous reviewers for their useful comments.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bell-Aldeghi, R., Sirven, N., Le Guern, M. et al. One last effort. Are high out-of-pocket payments at the end of life a fatality?. Eur J Health Econ 23, 879–891 (2022). https://doi.org/10.1007/s10198-021-01401-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-021-01401-1