Abstract
The German health care system is among the most patient-oriented systems in Europe. Nevertheless, distinct utilisation patterns, access barriers due to socio-economic profiles, and potentials of misallocation of medical resources lead to disparities in the provision of health care services. We analyse how a possible over- and undersupply of services and the utilisation of and the access to the health care system relate to regional variations in the population’s well-being. For this purpose, we employ a recent Bayesian stochastic frontier approach that allows for spatial dependence structures. Our results indicate that patient migration plays an important role in contributing to regional differences in the utilisation of the medical infrastructure. As a consequence, policy should take spatial patterns of health care utilisation into account to improve the allocation of medical resources.




Similar content being viewed by others
Notes
The software is freely available from https://www.uni-goettingen.de/en/550513.html.
For a detailed description of the variables, see Herwartz and Schley [34].
As mortality can be seen as an undesirable output in a health production context, we invert the SMR to represent a desirable output.
The number of dialysis devices is measured at federal state level.
Specifically, we determine the standard deviation within each district across count statistics for five medical specialists groups (internists, ophthalmologists, orthopaedists, psychotherapists per 100,000 inhabitants, and pediatricians per 100,000 children).
The dependent variable is the log inverted SMR and the explanatory variables are gp, spec, beds, dialysis and speciality diversity in natural logarithms joint with time and district fixed effects.
We construct instruments for the endogenous regressors from their respective lagged first differences. If the error terms are free of serial correlation, these lags will be highly correlated with the endogenous regressors, but uncorrelated with the composite residual process. The lagged instruments range from t − 1 to t − 8. If the assumptions of the Hausman test are met, the IV estimator is consistent, however, OLS is efficient under the null hypothesis of no systematic difference between the estimators [33].
In both IV approaches, the time and district-specific fixed effects are considered as exogenous.
We additionally tested for instrument validity by means of a Sargan Test [63]. The test returned p values of 0.147 (IV1) and 0.159 (IV2). Therefore, we conclude that the instruments fulfill the exogeneity condition.
All estimation results are obtained via full Bayesian MCMC simulations based on 120,000 iterations, a burn-in period of 20,000 iterations and a thinning parameter of 100, resulting in 1000 samples from the posterior. Convergence of the Markov chains are ensured by eyeball inspection. Accordingly, we did not find any evidence for remaining autocorrelation in the sampling paths.
Both model selection criteria can be determined from the MCMC output. Unlike the DIC, the WAIC evaluates the entire posterior distribution, and, hence, might preferred if the posterior distribution lacks normality.
For instance, for the care of back pain, Andersohn and Walker [3] show that the number of conducted operations varies significantly across regions with an increased number of surgical interventions in areas with medical centres specialised on back problems in Germany.
We further included the dummy variable east to account for differences between Eastern and Western Germany. However, the effect of this variable lacks statistical significance.
It is worth recalling that Germany comprises 402 districts for which we allow spatial dependence patterns. However, we excluded nineteen districts due to data inconsistencies and missing values. By means of the Markov random field (structured spatial effect), we obtain an effect for all 402 districts in Germany while the unstructured (random) spatial contributions are only estimated for regions with at least one observation. In consequence, the estimated spatial effects should be viewed with caution for the districts with no observation.
We evaluate efficiency scores for each district \(i\) in time \(t\) by the mean of the posterior distribution of technical efficiencies as \({\mathbb{E}}\left[ {{ \exp }\left( { - u_{it} |e_{it} } \right)} \right]\), where \(e_{it}\) is the composite error term \(e_{it} = y_{it} + u_{it}\) in (1) [38]. We refer to Klein et al. [40] for the derivation of \(p\left( {u_{it} |e_{it} } \right)\) in the Bayesian framework.
To control for spatial spillover effects, we run a weighted least squares regression of the predicted efficiency scores on an intercept and a rural-urban dummy variable, and account for spatially correlated observations by using an adjacency matrix \(\varvec{A}\) as variance-weighting matrix (see Appendix 1). We evaluate differences in the predicted efficiency scores between urban and rural districts by means of a significance test for the aforementioned dummy variable.
The marginal effects of the regional characteristics on inefficiency directly translate into effects on health as \(\partial \left( {{\mathbb{E}}\left[ {logy_{it} } \right]} \right)/\partial z^{d} = - \partial \left( {{\mathbb{E}}\left[ {u_{it} } \right]} \right)/\partial z^{d}\), where \(z^{d}\) is the \(d\)-th variable in \(z_{it}\) in (4) [68].
A usual form to regularise is \(\lambda \varvec{\zeta 'K\zeta }\) [21].
Nevertheless, Fahrmeir and Lang [22] showed, that one can only achieve a clear separation of the structured and unstructured part of the spatial effect if one effect dominates the other.
References
Afonso, A. and M. St. Aubyn (2006). Relative efficiency of health provision: A DEA approach with non-discretionary Inputs. ISEG-UTL Economics Working Paper 33/2006
Albrecht, M., Etgeton, S., Ochmann, R.: Faktencheck Gesundheit: Regionale Verteilung von Arztsitzen (Ärztedichte). Bertelsmann Stiftung, Gütersloh (2014)
Andersohn, F., Walker, J.: Faktencheck Ru¨cken: Ausmaß und regionale Variationen von Behandlungsf¨allen und bildgebender Diagnostik. Bertelsmann Stiftung, Gütersloh (2016)
Augurzky, B., Beivers, A.: Das GKV-Versorgungsstrukturgesetz: Richtung richtig. Umsetzung unklar. RWI Positionen 48, 1–22 (2012)
Augurzky, B., Kopetsch, T., Schmitz, H.: What accounts for the regional differences in the utilisation of hospitals in Germany? Eur. J. Health Econ. 14(4), 615–627 (2013)
Belitz, C., A. Brezger, T. Kneib, S. Lang, and N. B. Umlauf (2015). BayesX: Software for Bayesian inference in structured additive regression models. Version 2.1. http://www.bayesx.org.
Brezger, A., Kneib, T., Lang, S.: BayesX: Analysing Bayesian structured additive regression models. Discussion Paper, Ludwig-Maximilians-Universität München (2003)
Burwell, S.M.: Setting value-based payment goals – HHS efforts to improve US health care. N. Engl. J. Med. 372(10), 897–899 (2015)
Carrillo, M., Jorge, J.M.: DEA-like efficiency ranking of regional health systems in Spain. Soc. Indic. Res. 133(3), 1–17 (2016)
Chakrabarti, A., Rao, D.N.: Efficiency in production of health: a stochastic frontier analysis for Indian states. In: Tavidze, A. (ed.) Global Economics, pp. 105–128. Nova Science Publishers, New York (2007)
Cordero, J.M., Alonso-Moran, E., Nuno-Solinis, R., Orueta, J.F., Arce, R.S.: Efficiency assessment of primary care providers: a conditional nonparametric approach. Eur. J. Oper. Res. 240(1), 235–244 (2015)
Correia, I., Veiga, P.: Geographic distribution of physicians in Portugal. Eur. J. Health Econ. 11(4), 383–393 (2010)
Cullen, M.R., Cummins, C., Fuchs, V.R.: Geographic and racial variation in premature mortality in the US: analyzing the disparities. PLoS ONE 7(4), e32930 (2012)
Derose, K.P., Bahney, B.W., Lurie, N., Escarce, J.J.: Immigrants and health care access, quality, and cost. Med. Care Res. Rev. 66(4), 355–408 (2009)
Derose, K.P., Escarce, J.J., Lurie, N.: Immigrants and health care: sources of vulnerability. Health Aff. 26(5), 1258–1268 (2007)
Dieleman, J.L., Sadat, N., Chang, A.Y., Fullman, N., Abbafati, C., Acharya, P., Adou, A.K., Kiadaliri, A.A., Alam, K., Alizadeh-Navaei, R., et al.: Trends in future health financing and coverage: future health spending and universal health coverage in 188 countries, 2016–40. The Lancet 391(10132), 1783–1798 (2018)
Dubay, L., Kenney, G.M.: Health care access and use among low-income children: who fares best? Health Aff. 20(1), 112–121 (2001)
Dunn, P.K., Smyth, G.K.: Randomized quantile residuals. J. Comput. Graph. Stat. 5(3), 236–244 (1996)
Eibich, P., Ziebarth, N.R.: Examining the structure of spatial health effects in Germany using hierarchical Bayes models. Regional Sci. Urban Econ. 49, 305–320 (2014)
Eilers, P.H., Marx, B.D.: Flexible smoothing with B-splines and penalties. Stat. Sci. 11(2), 89–102 (1996)
Fahrmeir, L., Kneib, T., Lang, S., Marx, B.: Regression: Models, Methods and Applications. Springer Science & Business Media, Berlin (2013)
Fahrmeir, L., Lang, S.: Bayesian inference for generalized additive mixed models based on Markov random field priors. J. R. Stat. Soc. 50(2), 201–220 (2001)
Fassio, O., Rollero, C., Piccoli, N.D.: Health, quality of life and population density: a preliminary study on ‘contextualized’ quality of life. Soc. Indic. Res. 110(2), 479–488 (2013)
Felder, S., Tauchmann, H.: Federal state differentials in the efficiency of health production in Germany: an artifact of spatial dependence? Eur. J. Health Econ. 14(1), 21–39 (2013)
Finkelstein, A., Gentzkow, M., Williams, H.: Sources of geographic variation in health care: evidence from patient migration. Q. J. Econ. 131(4), 1681–1726 (2016)
Gearhart, R.: The robustness of cross-country healthcare rankings among homogeneous OECD countries. J. Appl. Econ. 19(1), 113–143 (2016)
Gelman, A., Hwang, J., Vehtari, A.: Understanding predictive information criteria for Bayesian models. Statist. Comput. 24(6), 997–1016 (2014)
Gelman, A., Pardoe, I.: Bayesian measures of explained variance and pooling in multilevel (hierarchical) models. Technometrics 48(2), 241–251 (2006)
Greene, W.: Distinguishing between heterogeneity and inefficiency: stochastic frontier analysis of the World Health Organization’s panel data on national health care systems. Health Econ. 13(10), 959–980 (2004)
Hadad, S., Hadad, Y., Simon-Tuval, T.: Determinants of healthcare system’s efficiency in OECD countries. Eur. J. Health Econ. 14(2), 253–265 (2013)
Han, P.K., Klein, W.M., Arora, N.K.: Varieties of uncertainty in health care: a conceptual taxonomy. Med. Decis. Mak. 31(6), 828–838 (2011)
Hasenfuß, G., Märker-Hermann, E., Hallek, M., Fölsch, U.R.: Initiative „Klug entschieden“: gegen Unter- und Überversorgung. International 113(13), A600 (2016)
Hausman, J.A.: Specification tests in econometrics. Econometrica 46(6), 1251–1271 (1978)
Herwartz, H., Schley, K.: Improving health care service provision by adapting to regional diversity: an efficiency analysis for the case of Germany. Health Policy 122(3), 293–300 (2018)
Herwartz, H., Strumann, C.: Hospital efficiency under prospective reimbursement schemes: an empirical assessment for the case of Germany. Eur. J. Health Econ. 15(2), 175–186 (2014)
Hossain, M.K., Kamil, A.A., Baten, M.A., Mustafa, A.: Stochastic frontier approach and Data Envelopment Analysis to total factor productivity and efficiency measurement of Bangladeshi rice. PLoS ONE 7(10), e46081 (2012)
Jacobs, R., Smith, P.C., Street, A.: Measuring Efficiency in Health Care: Analytic Techniques and Health Policy. Cambridge University Press, Cambridge (2006)
Jondrow, J., Lovell, C.K., Materov, I.S., Schmidt, P.: On the estimation of technical inefficiency in the stochastic frontier production function model. J. Econ. 19(2–3), 233–238 (1982)
Keselman, H.J., Rogan, J.C.: A comparison of the modified-Tukey and Scheffe methods of multiple comparisons for pairwise contrasts. J. Am. Stat. Assoc. 73(361), 47–52 (1978)
Klein, N., Herwartz, H., Kneib, T.: Modelling regional patterns of efficiency: A Bayesian approach to geoadditive panel stochastic frontier analysis with an application to cereal production in England and Wales. J. Econ. (2019) (forthcoming)
Klein, N., Kneib, T., Lang, S., Sohn, A., et al.: Bayesian structured additive distributional regression with an application to regional income inequality in Germany. Ann. Appl. Stat. 9(2), 1024–1052 (2015)
Kopetsch, T., Schmitz, H.: Regional variation in the utilisation of ambulatory services in Germany. Health Econ. 23(12), 1481–1492 (2014)
Ku, L., Matani, S.: Left out: immigrants’ access to health care and insurance. Health Aff. 20(1), 247–256 (2001)
Kumbhakar, S.C., Lovell, C.K.: Stochastic Frontier Analysis. Cambridge University Press, Cambridge (2003)
Kwietniewski, L., Schreyögg, J.: Efficiency of physician specialist groups. Health Care Manag. Sci. 21(3), 409–425 (2018)
Lang, S., Brezger, A.: Bayesian P-splines. J. Comput. Graph. Stat. 13(1), 183–212 (2004)
Latzitis, N., Sundmacher, L., Busse, R.: Regionale Unterschiede der Lebenserwartung in Deutschland auf Ebene der Kreise und kreisfreien St¨adte und deren m¨oglichen Determinanten. Das Gesundheitswesen 73(04), 217–228 (2011)
Levinson, W., Kallewaard, M., Bhatia, R.S., Wolfson, D., Shortt, S., Kerr, E.A.: ‘Choosing Wisely’: a growing international campaign. BMJ Qual. Saf. 24(2), 167–174 (2015)
Lewbel, A.: Using heteroscedasticity to identify and estimate mismeasured and endogenous regressor models. J. Bus. Econ. Stat. 30(1), 67–80 (2012)
Lipitz-Snyderman, A., Bach, P.B.: Overuse of health care services: when less is more…more or less. JAMA Intern. Med. 173(14), 1277–1278 (2013)
Luasa, S.N., Dineen, D., Zieba, M.: Technical and scale efficiency in public and private Irish nursing homes—a bootstrap DEA approach. Health Care Manag. Sci. 23, 1–22 (2016)
McDade, T.W., Adair, L.S.: Defining the ‘urban’ in urbanization and health: a factor analysis approach. Soc. Sci. Med. 53(1), 55–70 (2001)
McNeil, B.J.: Hidden barriers to improvement in the quality of care. N. Engl. J. Med. 345(22), 1612–1620 (2001)
Mutter, R.L., Greene, W.H., Spector, W., Rosko, M.D., Mukamel, D.B.: Investigating the impact of endogeneity on inefficiency estimates in the application of stochastic frontier analysis to nursing homes. J. Prod. Anal. 39(2), 101–110 (2013)
Ozegowski, S., Sundmacher, L.: Understanding the gap between need and utilization in outpatient care—the effect of supply-side determinants on regional inequities. Health Policy 114(1), 54–63 (2014)
Parhizkar, T., Balali, S., Mosleh, A.: An entropy based bayesian network framework for system health monitoring. Entropy 20(6), 416 (2018)
Porter, M.E.: A strategy for health care reform—toward a value-based system. N. Engl. J. Med. 361(2), 109–112 (2009)
Pross, C., Strumann, C., Geissler, A., Herwartz, H., Klein, N.: Quality and resource efficiency in hospital service provision: a geoadditive stochastic frontier analysis of stroke quality of care in Germany. PLoS ONE 13(9), e0203017 (2018)
Rettenmaier, A.J., Wang, Z.: Regional variations in medical spending and utilization: a longitudinal analysis of US Medicare population. Health Econ. 21(2), 67–82 (2012)
Ricketts, T.C., Holmes, G.M.: Mortality and physician supply: does region hold the key to the paradox? Health Serv. Res. 42(6p1), 2233–2251 (2007)
Rollnick, S., Miller, W.R., Butler, C.C., Aloia, M.S.: Motivational interviewing in health care: helping patients change behavior. J. Chronic Obstruct. Pulm. Dis. 5(3), 203 (2008)
Salm, M., Wübker, A.: Causes of regional variation in healthcare utilization in Germany. Number 675. Ruhr Economic Papers. (2017)
Sargan, J.D.: Contributions to Econometrics, vol. 1. CUP Archive, Cambridge (1988)
Spiegelhalter, D.J., Best, N.G., Carlin, B.P., Linde, A.: The deviance information criterion: 12 years on. J. R. Stat. Soc. 76(3), 485–493 (2014)
Sundmacher, L.: Trends and levels of avoidable mortality among districts: ‘Healthy’ benchmarking in Germany. Health Policy 109(3), 281–289 (2013)
The Darthmouth Atlas of Health Care.: Supply-sensitive care. http://www.dartmouthatlas.org/keyissues/issue.aspx?con=2937 (2018). Accessed 15 May 2018
Varabyova, Y., Schreyögg, J.: International comparisons of the technical efficiency of the hospital sector: panel data analysis of OECD countries using parametric and nonparametric approaches. Health Policy 112(1–2), 70–79 (2013)
Wang, H.-J.: Heteroscedasticity and non-monotonic efficiency effects of a stochastic frontier model. J. Prod. Anal. 18(3), 241–253 (2002)
Watanabe, S.: A widely applicable bayesian information criterion. J. Mach. Learn. Res. 14, 867–897 (2013)
Wendt, C.: Mapping european healthcare systems: a comparative analysis of financing, service provision and access to healthcare. J. Eur. Social Policy 19(5), 432–445 (2009)
Acknowledgements
Financial support by the German Research Association (DFG) Research Training Group 1644 ‘Scaling problems in Statistics’, Grant no. 152112243, is gratefully acknowledged. Helpful comments from two anonymous referees are also gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix
The following appendices provide further details on the Bayesian estimation procedure and the derivation of the marginal effects of the \(z\) variables.
The Bayesian stochastic frontier model
Prior specification
In a fully Bayesian approach, the general form of a normal regularisation-type prior with penalisation term and smoothing variance for a vector of unknown regression coefficients \({\varvec{\upzeta}}\) is given by:
In (6), \(\varvec{K}\) is a known penalty matrix which is chosen a priori and the smoothing variance is \(\tau^{2} = 1/\lambda\) where \(\lambda \ge 0\) is an unknown smoothing component that determines the strength of the regularisation to avoid overfitting.Footnote 19 To obtain a data-driven degree of smoothness, we assign an inverse gamma hyperprior to \(\tau^{2}\), i.e., \(\tau^{2} \sim IG\left( {a,b} \right)\) with \(a = b = 0.001\), which is the common choice in Bayesian estimation [21]. In summary, the general form of (6) offers a practical and flexible way to deal with any unknown regression coefficients by an adequate choice of \(\varvec{K}\).
Linear and nonlinear effects
In (1) and (4) the coefficient \(\varvec{\beta}\) and \(\varvec{\delta}\) describe the linear influences of the covariate vectors \(x_{it}\) and \(z_{it}\), respectively. For estimation purpose, we replace the variance components of \(u_{it}^{*}\) and \(v_{it}\) by \(\sigma_{u}^{2} = { \exp }\left\{ {c_{u} } \right\}\) and \(\sigma_{v}^{2} = { \exp }\left\{ {c_{v} } \right\}\), respectively, where \(c_{u}\)and \(c_{v}\) are coefficients to be estimated. We restrict (6) with \(\varvec{K} = 0\) to obtain completely non-informative priors. Therefore, the joint prior distributions for \(\beta\), \(\delta\), \(c_{u}\), \(c_{v}\) and \(\mu\) are flat, i.e. \(p\left( \beta \right)\), \(p\left( \delta \right)\), \(p\left( {c_{u} } \right)\), \(p\left( {c_{v} } \right)\), \(p\left( \mu \right) \propto const\).
We model the nonlinear effect of a covariate \(\tilde{x}_{it}\) by means of a smooth function \(f\left( {\tilde{x}_{it} } \right)\). We apply P-splines as introduced by Eilers and Marx [20], and approximate the unknown function by a polynomial spline of degree 3 with 20 equidistantly spaced knots over the domain of \(\tilde{x}_{it}\): \(f\left( {\tilde{x}_{it} } \right) = \varvec{W\tilde{\beta }}\), where \(\varvec{W}\) is the design matrix comprising the basis functions at the observed covariate values and \(\tilde{\varvec{\beta }}\) is a vector of regression coefficients to be estimated. Following Eilers and Marx [20] and Belitz et al. [6], for \(\varvec{\zeta}= \tilde{\varvec{\beta }}\) in (6) the matrix \(\varvec{K}\) comprises a second-order random walk penalty term to obtain a regularised function \(f\left( {\tilde{x}_{it} } \right)\).Footnote 20
Spatial components
To model spatial dependencies, we consider structured spatial effects in the production function (\(\gamma_{i}\)) and in the scaling function (\(\theta_{i}\)). We assign a Markov random field prior to the joint distribution of \(\varvec{\gamma}\) and \(\varvec{\theta}\) [22]. To obtain the representation in (6) for \(\varvec{\zeta}=\varvec{\gamma}\) and \(\varvec{\zeta}=\varvec{\theta}\), respectively, we define a first-order neighbourhood structure on the set of German districts. Thus, the we set \(\varvec{K}\) equal to an adjacency matrix \(\varvec{A}\), which takes the form of an indicator matrix, where the off-diagonal elements are equal to unity if two districts share a common border, and zero otherwise.
As the district-specific effects \(\alpha_{i}\) are independent of the neighbourhood structure in \(\varvec{A}\), one can interpret them as structured spatial effects. In that way, the joint prior distribution of \(\varvec{\alpha}\) corresponds to a Markov random field without neighbourhood structure. We specify the distribution in (6) for \(\varvec{\zeta}=\varvec{\alpha}\) by setting \(\varvec{K}\) equal to an identity matrix \(\varvec{I}\). In summary, the decomposition into structured and unstructured spatial components allows for additional flexibility in the model to recover more general spatial dependencies.Footnote 21
Estimation
The MCMC estimation algorithm is implemented in a developer version of the freely available software BayesX [6, 40] provide a detailed description of thse sampling algorithms which we adopt. Bayesian inference is based on the posterior density functions of the model given by \(p\left( {\zeta |y} \right) \propto p\left( {y|\zeta } \right)p\left( \zeta \right)\), which are obtained from the sampling paths to easily draw inferential results. For simplicity, \(\zeta\) denotes the collection of all unknown model parameters, and \(p\left( \zeta \right)\) are the respective prior distributions which are all of the type of (6), but differ from each other due to the different specifications of \(\varvec{K}\).
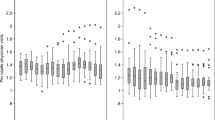
Quantile residuals
See Fig. 5,
Since SFA’s fit into the class of distributional regression models, quantile residuals are commonly used to check if the model has been correctly specified [41]. Quantile residuals are defined as \(\hat{r}_{i} = {\varvec{\Phi}}^{ - 1} ( {F( {y_{i} \left| {\hat{\varvec{\vartheta }}_{i} } \right.} )} )\), with the inverse cumulative distribution function (c.d.f.) of a standard normal distribution \(\varPhi^{ - 1}\) and \(F\left( {. |\hat{\varvec{\vartheta }}} \right)\) denoting the c.d.f. with model specific parameters, i.e., \(\hat{\varvec{\vartheta }}_{0} = \left( {\varvec{\alpha}, \varvec{\beta}, \tilde{\varvec{\beta }}_{1} , \ldots , \tilde{\varvec{\beta }}_{\varvec{J}} ,\varvec{\delta}, \sigma_{v}^{2} , \sigma_{{u^{*} }}^{2} , \mu } \right)^{\prime }\), \(\hat{\vartheta }_{I} = \left( {\varvec{\alpha}, \varvec{\beta}, \tilde{\varvec{\beta }}_{1} , \ldots ,\tilde{\varvec{\beta }}_{\varvec{J}} ,\varvec{ \delta },\varvec{\gamma}, \sigma_{v}^{2} , \sigma_{{u^{*} }}^{2} , \mu } \right)^{\prime } , \hat{\vartheta }_{II} = \left( {\varvec{\alpha}, \varvec{\beta}, \tilde{\varvec{\beta }}_{1} , \ldots ,\tilde{\varvec{\beta }}_{\varvec{J}} ,\varvec{ \delta },\varvec{\theta},\sigma_{v}^{2} , \sigma_{{u^{*} }}^{2} , \mu } \right)^{\prime } , \hat{\vartheta }_{II} = \left( {\varvec{\alpha}, \varvec{\beta}, \tilde{\varvec{\beta }}_{1} , \ldots , \tilde{\varvec{\beta }}_{\varvec{J}} ,\varvec{ \delta },\varvec{\theta},\sigma_{v}^{2} , \sigma_{{u^{*} }}^{2} , \mu } \right)^{\prime } ,\) where the indices are used to distinguish the model specifications ‘0′ to ‘III’ as outlined in Sect. 3.2.1. Based on the SFA specification, \(F\left( {. |\hat{\vartheta }} \right)\) is a mixed normal-half normal distribution [44]. According to Dunn and Smyth [18], the quantile residuals should at least approximately be standard normally distributed if the correct model has been specified. In practice, the residuals can be subjected to eyeball inspection in terms of QQ-plots.
Bayesian R2
In Bayesian inference one obtains a set of posterior simulation draws \(l = 1, \ldots , L\). For each draw, one obtains the vector of predicted values \(\hat{\varvec{y}}^{\left( l \right)}\) and residuals \(\varvec{e}^{\left( l \right)} = \varvec{y} - \hat{\varvec{y}}^{\left( l \right)}\) over all cross-sectional \(i = 1, \ldots , N\) and time instances \(t = 1, \ldots , T\). For each posterior draw \(l\), we calculate the proportion of variance explained as:
Since an R2l obtains for each posterior draw l = 1,…, L, we summarise this sample information by its posterior mean. The Bayesian R2 can be interpreted as a data-based estimate of the proportion of variance explained by the model [27, 28].
Marginal effects
In (4), the scaling function \(h_{it} = { \exp }\left\{ {z_{it}^{'} \delta + \theta_{i} } \right\}\) translates the effects of \(z_{it}\), denoted by \(\delta\), to both the mean and the variance of \(u_{it}^{*}\). The parametrisation of \(u_{it} = h_{it} u_{it}^{*}\) with \(u_{it}^{*} \sim N^{ + } \left( {\mu ,\sigma^{2} } \right)\) is equivalent to \(u_{it} \sim N^{ + } (\mu_{it}^{*} ,\left( {\sigma_{it}^{2} )^{*} } \right)\) where \(\mu_{it}^{*} = \mu { \exp }\left\{ {z_{it}^{'} \delta + \theta_{i} } \right\}\) and \((\sigma_{it}^{2} )^{*} = \sigma^{2} { \exp }\left\{ {2z_{it}^{'} \delta + 2\theta_{i} } \right\}.\) According to Wang [68], the first two moments of \(u_{it}\)read as
where \(a = \frac{{\mu_{it}^{*} }}{{\sigma_{it}^{*} }}\) and \(\varphi ( \cdot )\) and \(\varPhi \left( \cdot \right)\) denote the probability density function and the cumulative
density function of the standard normal distribution, respectively. Then, the marginal effect of a change in the \(d\)-th variable in \(z_{it}\) on the respective moments of \(u_{it}\) is given by the partial first derivatives:
where \(\delta^{d}\) is the coefficient of the \(d\)-th variable in \(\delta\).
Rights and permissions
About this article
Cite this article
Haschka, R.E., Schley, K. & Herwartz, H. Provision of health care services and regional diversity in Germany: insights from a Bayesian health frontier analysis with spatial dependencies. Eur J Health Econ 21, 55–71 (2020). https://doi.org/10.1007/s10198-019-01111-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-019-01111-9
Keywords
- Health production
- Health efficiency
- Stochastic frontier analysis
- Oversupply of medical services
- Regional misallocation
- Bayesian estimation
- Regional and spatial modelling
- Markov-chain–Monte Carlo simulation