Abstract
Objectives
Stroke is a leading cause for disability and morbidity associated with increased economic burden due to treatment and post-stroke care (PSC). The aim of our study is to provide information on resource consumption for PSC, to identify relevant cost drivers, and to discuss potential information gaps.
Methods
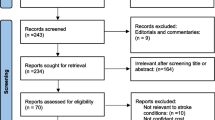
A systematic literature review on economic studies reporting PSC-associated data was performed in PubMed/MEDLINE, Scopus/Elsevier and Cochrane databases, Google Scholar and gray literature ranging from January 2000 to August 2016. Results for post-stroke interventions (treatment and care) were systematically extracted and summarized in evidence tables reporting study characteristics and economic outcomes. Economic results were converted to 2015 US Dollars, and the total cost of PSC per patient month (PM) was calculated.
Results
We included 42 studies. Overall PSC costs (inpatient/outpatient) were highest in the USA ($4850/PM) and lowest in Australia ($752/PM). Studies assessing only outpatient care reported the highest cost in the United Kingdom ($883/PM), and the lowest in Malaysia ($192/PM). Fifteen different segments of specific services utilization were described, in which rehabilitation and nursing care were identified as the major contributors.
Conclusion
The highest PSC costs were observed in the USA, with rehabilitation services being the main cost driver. Due to diversity in reporting, it was not possible to conduct a detailed cost analysis addressing different segments of services. Further approaches should benefit from the advantages of administrative and claims data, focusing on inpatient/outpatient PSC cost and its predictors, assuring appropriate resource allocation.




Similar content being viewed by others
Abbreviations
- TIA:
-
Transient ischemic attacks
- WHO:
-
World Health Organization
- PPP:
-
Purchasing power parity
- CPI:
-
Consumer Price Index
- CHEERS:
-
Consolidated Health Economic Evaluation Reporting Standards
- SRF:
-
Skilled nursing facilities
- IRF:
-
Inpatient rehabilitation facilities
- ESUS:
-
Extended stroke unit services
- OSUS:
-
Ordinary stroke unit services
- PSC:
-
Post-stroke care
- PM:
-
Patient month
- GDP:
-
Gross domestic product
- AUD:
-
Australian Dollar
- CAD:
-
Canadian Dollar
- DM:
-
Deutsche Mark
- SEK:
-
Swedish Krona
- CHF:
-
Swiss Franc
- £:
-
UK Pound
- $, USD:
-
US Dollar
References
Land Tirol. (2018). Projekt Integrierter Patientenpfad/Behandlungspfad Schlaganfall Tirol. https://www.schlaganfall-tirol.info https://www.tirol.gv.at/gesundheit-vorsorge/krankenanstalten/schlaganfall/projekt/. Accessed 4 Mar 2017
World Health Organization: Global Health Estimates: Deaths by Cause, Age, Sex and Country, 2000–2012. Geneva, WHO (2014)
Mozaffarian, D., Benjamin, E.J., Go, A.S., Arnett, D.K., Blaha, M.J., Cushman, M., de Ferranti, S., Despres, J.P., Fullerton, H.J., Howard, V.J., Huffman, M.D., Judd, S.E., Kissela, B.M., Lackland, D.T., Lichtman, J.H., Lisabeth, L.D., Liu, S., Mackey, R.H., Matchar, D.B., McGuire, D.K., Mohler, E.R. III, Moy, C.S., Muntner, P., Mussolino, M.E., Nasir, K., Neumar, R.W., Nichol, G., Palaniappan, L., Pandey, D.K., Reeves, M.J., Rodriguez, C.J., Sorlie, P.D., Stein, J., Towfighi, A., Turan, T.N., Virani, S.S., Willey, J.Z., Woo, D., Yeh, R.W., Turner, M.B.: Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation 131(4), e29–e322 (2015). https://doi.org/10.1161/cir.0000000000000152
Truelsen, T., Piechowski-Jozwiak, B., Bonita, R., Mathers, C., Bogousslavsky, J., Boysen, G.: Stroke incidence and prevalence in Europe: a review of available data. Eur. J. Neurol. 13(6), 581–598 (2006). https://doi.org/10.1111/j.1468-1331.2006.01138.x
Di Carlo, A.: Human and economic burden of stroke. Age Ageing. 38(1), 4–5 (2009). https://doi.org/10.1093/ageing/afn282
Ovbiagele, B., Goldstein, L.B., Higashida, R.T., Howard, V.J., Johnston, S.C., Khavjou, O.A., Lackland, D.T., Lichtman, J.H., Mohl, S., Sacco, R.L., Saver, J.L., Trogdon, J.G.: Forecasting the future of stroke in the United States: a policy statement from the American Heart Association and American Stroke Association. Stroke J. Cereb. Circ. 44(8), 2361–2375 (2013). https://doi.org/10.1161/STR.0b013e31829734f2
Stroke.org. (2018). Rehabilitation Therapy after a Stroke. http://www.stroke.org/we-can-help/stroke-survivors/just-experienced-stroke/rehab. Accessed 8 Feb 2018
Brady, B.K., McGahan, L., Skidmore, B.: Systematic review of economic evidence on stroke rehabilitation services. Int. J. Technol. Assess. Health Care 21(1), 15–21 (2005)
Anderson, C., Ni Mhurchu, C., Brown, P.M., Carter, K.: Stroke rehabilitation services to accelerate hospital discharge and provide home-based care: an overview and cost analysis. Pharmacoeconomics 20(8), 537–552 (2002)
Larsen, T., Olsen, T.S., Sorensen, J.: Early home-supported discharge of stroke patients: a health technology assessment. Int. J. Technol. Assess. Health Care 22(3), 313–320 (2006)
Tummers, J.F., Schrijvers, A.J., Visser-Meily, J.M.: Economic evidence on integrated care for stroke patients; a systematic review. Int. J. Integr. Care 12, e193 (2012)
Polder, J.J.: Cost of illness in the Netherlands: description, comparison and projection. Thesis, Erasmus University Rotterdam (2001)
Harrington, R., Taylor, G., Hollinghurst, S., Reed, M., Kay, H., Wood, V.A.: A community-based exercise and education scheme for stroke survivors: a randomized controlled trial and economic evaluation. Clin. Rehabilit. 24(1), 3–15 (2010). https://doi.org/10.1177/0269215509347437
Humphreys, I., Thomas, S., Phillips, C., Lincoln, N.: Cost analysis of the communication and low mood (CALM) randomised trial of behavioural therapy for stroke patients with aphasia. Clin. Rehabilit. 29(1), 30–41 (2015). https://doi.org/10.1177/0269215514537656
Patel, A., Knapp, M., Evans, A., Perez, I., Kalra, L.: Training care givers of stroke patients: economic evaluation. BMJ. 328(7448), 1102 (2004). https://doi.org/10.1136/bmj.328.7448.1102
Drummond, M.F., Sculpher, M.J., Torrance, G.W., O’Brien, B., Stoddart, G.L.,: Methods for the Economic Evaluation of Health Care Programmes, 3rd edn. Oxford University Press, Oxford (2005)
Wang, G., Zhang, Z., Ayala, C., Dunet, D.O., Fang, J., George, M.G.: Costs of hospitalization for stroke patients aged 18–64 years in the United States. J. Stroke Cerebrovasc. Dis. 23(5), 861–868 (2014). https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.07.017
U.S. Department of Labor, Bureau of Labor Statistics, Consumer Price Index. All Urban Consumers (CPI-U). http://www.bls.gov/cpi/ (2015). Accessed 18 Dec 2015
World Bank. Data: GDP per capita. http://data.worldbank.org/indicator/NY.GDP.PCAP.CD (2016). Accessed 8 Aug 2016
OECD (2018) Hospital beds (indicator). https://doi.org/10.1787/0191328e-en
Drummond, M.F., Jefferson, T.O.: Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ economic evaluation working party. BMJ 313(7052), 275–283 (1996)
Husereau, D., Drummond, M., Petrou, S., Carswell, C., Moher, D., Greenberg, D., Augustovski, F., Briggs, A.H., Mauskopf, J., Loder, E.: Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMC Med. 11(1), 1–6 (2013). https://doi.org/10.1186/1741-7015-11-80
Moher, D., Liberati, A., Tetzlaff, J., Altman, D.G.: Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6(7), e1000097 (2009). https://doi.org/10.1371/journal.pmed.1000097
Akhavan Hejazi, S.M., Mazlan, M., Abdullah, S.J., Engkasan, J.P.: Cost of post-stroke outpatient care in Malaysia. Singap. Med. J. 56(2), 116–119 (2015)
Gold M.R., Siegel J.E., Russell L.B., Weinstein M.C.: Estimating costs in cost-effectiveness analysis. In: Cost-effectiveness in health and medicine, pp. 176–213. Oxford University Press, New York (1996)
Beeuwkes-Buntin, M.B., Colla, C.H., Deb, P., Sood, N., Escarce, J.J.: Medicare spending and outcomes after postacute care for stroke and hip fracture. Med. Care 48(9), 776–784 (2010). https://doi.org/10.1097/MLR.0b013e3181e359df
Bjorkdahl, A., Sunnerhagen, K.S.: Process skill rather than motor skill seems to be a predictor of costs for rehabilitation after a stroke in working age; a longitudinal study with a 1 year follow up post discharge. BMC Health Serv. Res. 7, 209 (2007). https://doi.org/10.1186/1472-6963-7-209
Hayes, J., Vogel, B., Reker, D.M.: Factors associated with VHA costs of care for first 12 months after first stroke. J. Rehabilit. Res. Dev. 45(9), 1375–1384 (2008)
Kalra, L., Evans, A., Perez, I., Knapp, M., Swift, C., Donaldson, N.: A randomised controlled comparison of alternative strategies in stroke care. Health Technol. Assess. (Winchester, England) 9(18), iii–iv (2005) (1–79)
Tay-Teo, K., Moodie, M., Bernhardt, J., Thrift, A.G., Collier, J., Donnan, G., Dewey, H.: Economic evaluation alongside a phase II, multi-centre, randomised controlled trial of very early rehabilitation after stroke (AVERT). Cerebrovasc. Dis. (Basel, Switzerland). 26(5), 475–481 (2008). https://doi.org/10.1159/000155984
Forster, A., Young, J., Green, J., Patterson, C., Wanklyn, P., Smith, J., Murray, J., Wild, H., Bogle, S., Lowson, K.: Structured re-assessment system at 6 months after a disabling stroke: a randomised controlled trial with resource use and cost study. Age Ageing 38(5), 576–583 (2009). https://doi.org/10.1093/ageing/afp095
Simpson, A.N., Bonilha, H.S., Kazley, A.S., Zoller, J.S., Simpson, K.N., Ellis, C.: Impact of outpatient rehabilitation medicare reimbursement caps on utilization and cost of rehabilitation care after ischemic stroke: do caps contain costs? Arch. Phys. Med. Rehabilit. (2015). https://doi.org/10.1016/j.apmr.2015.07.008
Van Exel, J., Koopmanschap, M.A., Van Wijngaarden, J.D., Scholte Op Reimer, W.J.: Costs of stroke and stroke services: determinants of patient costs and a comparison of costs of regular care and care organised in stroke services. Cost Effect. Resour. Alloc. C/E 1(1), 2 (2003)
Godwin, K.M., Wasserman, J., Ostwald, S.K.: Cost associated with stroke: outpatient rehabilitative services and medication. Top. Stroke Rehabilit. 18 Suppl 1, 676–684 (2011). https://doi.org/10.1310/tsr18s01-676
Mahler, M.P., Zuger, K., Kaspar, K., Haefeli, A., Jenni, W., Leniger, T., Beer, J.H.: A cost analysis of the first year after stroke - early triage and inpatient rehabilitation may reduce long term costs. Swiss Med. Wkly. 138(31–32), 459–465 (2008)
Liberati, A., Altman, D.G., Tetzlaff, J., Mulrow, C., Gøtzsche, P.C., Ioannidis, J.P.A., Clarke, M., Devereaux, P.J., Kleijnen, J., Moher, D.: The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann. Intern. Med. 151(4), W-65 (2009). https://doi.org/10.7326/0003-4819-151-4-200908180-00136
Demaerschalk, B.M., Hwang, H.M., Leung, G.: US cost burden of ischemic stroke: a systematic literature review. Am. J. Manag. Care 16(7), 525–533 (2010)
Ekman, M.: Economic evidence in stroke: a review. Eur. J. Health Econ. HEPAC Health Econ. Prev. Care 5(Suppl 1), 74–83 (2004). https://doi.org/10.1007/s10198-005-0292-3
Grieve, R., Hutton, J., Bhalla, A., Rastenyte, D., Ryglewicz, D., Sarti, C., Lamassa, M., Giroud, M., Dundas, R., Wolfe, C.D.: A comparison of the costs and survival of hospital-admitted stroke patients across Europe. Stroke J. Cereb. Circ. 32(7), 1684–1691 (2001)
Everink, I.H.J., van Haastregt, J.C.M., van Hoof, S.J.M., Schols, J.M.G.A., Kempen, G.I.J.M.: Factors influencing home discharge after inpatient rehabilitation of older patients: a systematic review. BMC Geriatr. 16(1), 1–14 (2016). https://doi.org/10.1186/s12877-016-0187-4
Meijer, R., Ihnenfeldt, D.S., van Limbeek, J., Vermeulen, M., de Haan, R.J.: Prognostic factors in the subacute phase after stroke for the future residence after six months to one year. A systematic review of the literature. Clin. Rehabilit. 17(5), 512–520 (2003)
Brinjikji, W., Rabinstein, A.A., Cloft, H.J.: Hospitalization costs for acute ischemic stroke patients treated with intravenous thrombolysis in the United States are substantially higher than medicare payments. Stroke J. Cereb. Circ. 43(4), 1131–1133 (2012). https://doi.org/10.1161/strokeaha.111.636142
Claesson, L., Gosman-Hedstrom, G., Johannesson, M., Fagerberg, B., Blomstrand, C.: Resource utilization and costs of stroke unit care integrated in a care continuum: a 1-year controlled, prospective, randomized study in elderly patients: the Goteborg 70 + stroke study. Stroke J. Cereb. Circ. 31(11), 2569–2577 (2000)
Jain, M., Jain, A., Jahromi, B.S.: Strategies to improve cost-efficiency of stroke care: Stroke units and telestroke. In: Robinson, J.S., Walid, M.S., Barth, A.C.M. (eds.) Toward Healthcare Resource Stewardship. Hauppauge, New York: Nova Publishers (2012)
Saka, O., Serra, V., Samyshkin, Y., McGuire, A., Wolfe, C.C.: Cost-effectiveness of stroke unit care followed by early supported discharge. Stroke J. Cereb. Circ. 40(1), 24–29 (2009). https://doi.org/10.1161/strokeaha.108.518043
Te Ao, B.J., Brown, P.M., Feigin, V.L., Anderson, C.S.: Are stroke units cost effective? Evidence from a New Zealand stroke incidence and population-based study. Int. J. Stroke 7(8), 623–630 (2012). https://doi.org/10.1111/j.1747-4949.2011.00632.x
Miller, P., Gladman, J.R., Cunliffe, A.L., Husbands, S.L., Dewey, M.E., Harwood, R.H.: Economic analysis of an early discharge rehabilitation service for older people. Age and ageing (2005). https://doi.org/10.1093/ageing/afi058
Saka, R.O., McGuire, A., Wolfe, C.D.A.: Economic Burden of Stroke in England. University of London. https://www.nao.org.uk/wp-content/uploads/2005/11/0506452_economic_analysis.pdf (2003). Accessed 8 Aug 2016
Ghatnekar, O., Persson, U., Glader, E.L., Terent, A.: Cost of stroke in Sweden: an incidence estimate. Int. J. Technol. Assess. Health Care 20(3), 375–380 (2004)
Ghatnekar, O., Persson, U., Asplund, K., Glader, E.L.: Costs for stroke in Sweden 2009 and developments since 1997. Int. J. Technol. Assess. Health Care 30(2), 203–209 (2014). https://doi.org/10.1017/s0266462314000075
Kolominsky-Rabas, P.L., Heuschmann, P.U., Marschall, D., Emmert, M., Baltzer, N., Neundorfer, B., Schoffski, O., Krobot, K.J.: Lifetime cost of ischemic stroke in Germany: results and national projections from a population-based stroke registry: the Erlangen Stroke Project. Stroke J. Cereb. Circ. 37(5), 1179–1183 (2006). https://doi.org/10.1161/01.str.0000217450.21310.90
Gloede, T.D., Halbach, S.M., Thrift, A.G., Dewey, H.M., Pfaff, H., Cadilhac, D.A.: Long-term costs of stroke using 10-year longitudinal data from the North East Melbourne Stroke Incidence Study. Stroke J. Cereb. Circ. 45(11), 3389–3394 (2014). https://doi.org/10.1161/strokeaha.114.006200
Spieler, J.F., De Pouvourville, G., Amarenco, P.: Cost of a recurrent vs. cost of first-ever stroke over an 18-month period. Eur. J. Neurol. 10(6), 621–624 (2003)
Christensen, M.C., Morris, S.: Association between disability measures and short-term health care costs following intracerebral hemorrhage. Neurocrit. Care 9(3), 313–318 (2008). https://doi.org/10.1007/s12028-008-9124-5
Alonso-Freyre, J.L., Basanta, L., Vasquez-Roque, A., Vera-Miyar, C.R., Santos-Monzon, Y., Lopez-Hernandez, L.: Degree of independence and cost of ischaemic stroke. Revista de neurologia 32(9), 897–899 (2001)
Fearon, W.F., Shilane, D., Pijls, N.H., Boothroyd, D.B., Tonino, P.A., Barbato, E., Juni, P., De Bruyne, B., Hlatky, M.A.: Cost-effectiveness of percutaneous coronary intervention in patients with stable coronary artery disease and abnormal fractional flow reserve. Circulation. 128(12), 1335–1340 (2013). https://doi.org/10.1161/circulationaha.113.003059
Schreyer, P., Koechlin, F.: Purchasing Power Parities—Measurement and Uses. OECD Statistics Brief, No. 3, March. OECD, Paris (2002)
Swart, E.: Health care utilization research using secondary data. In: Janssen, C., Swart, E., von Lengerke, T. (eds.) Health Care Utilization in Germany: Theory, Methodology, and Results, pp. 63–86. Springer, New York (2014)
Swart, E., Ihle, P., Gothe, H., Matusiewicz, D.: Routinedaten im Gesundheitswesen. Handbuch Sekundärdatenanalyse: Grundlagen, Methoden und Perspektiven. 2. vollständig überarb. Aufl. Hans Huber, Bern (2014)
Siebert, U.: When should decision-analytic modeling be used in the economic evaluation of health care? Eur. J. Health Econ. 4(3), 143–150 (2003). https://doi.org/10.1007/s10198-003-0205-2
Siebert, U., Rochau, U., Claxton, K.: When is enough evidence enough? Using systematic decision analysis and value-of-information analysis to determine the need for further evidence. Zeitschrift fur Evidenz, Fortbildung und Qualitat im Gesundheitswesen. 107(9–10), 575–584 (2013). https://doi.org/10.1016/j.zefq.2013.10.020
Anderson, C., Rubenach, S., Mhurchu, C.N., Clark, M., Spencer, C., Winsor, A.: Home or hospital for stroke rehabilitation? Results of a randomized controlled trial: I: health outcomes at 6 months. Stroke J. Cereb. Circ. 31(5), 1024–1031 (2000)
Cadilhac, D.A., Carter, R., Thrift, A.G., Dewey, H.M.: Estimating the long-term costs of ischemic and hemorrhagic stroke for Australia: new evidence derived from the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke J. Cereb. Circ. 40(3), 915–921 (2009). https://doi.org/10.1161/strokeaha.108.526905
Dewey, H.M., Thrift, A.G., Mihalopoulos, C., Carter, R., Macdonell, R.A., McNeil, J.J., Donnan, G.A.: Cost of stroke in Australia from a societal perspective: results from the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke J. Cereb. Circ. 32(10), 2409–2416 (2001)
Dewey, H.M., Thrift, A.G., Mihalopoulos, C., Carter, R., Macdonell, R.A., McNeil, J.J., Donnan, G.A.: Lifetime cost of stroke subtypes in Australia: findings from the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke J. Cereb. Circ. 34(10), 2502–2507 (2003). https://doi.org/10.1161/01.str.0000091395.85357.09
Spieler, J.F., Lanoe, J.L., Amarenco, P.: Costs of stroke care according to handicap levels and stroke subtypes. Cerebrovasc. Dis. (Basel, Switzerland). 17(2–3), 134–142 (2004). https://doi.org/10.1159/000075782
Abbas, S., Ihle, P., Hein, R., Schubert, I.: Rehabilitation in geriatric patients after ischemic stroke—a comparison of 2 organisational systems in Germany using claims data of a statutory health insurance fund. Die Rehabil. 52(6), 375–382 (2013). https://doi.org/10.1055/s-0033-1334914
Weimar, C., Lüngen, M., Wagner, M., Kraywinkel, K., Evers, T., Busse, O., Haberl, R.L., Laaser, U., Lauterbach, K.W., Diener, H.C.: Cost of stroke care in Germany—an analysis of the stroke data bank of the German foundation stroke-aid. Aktuelle Neurol. 29(4), 181–190 (2002). https://doi.org/10.1055/s-2002-30690
Weimar, C., Weber, C., Wagner, M., Busse, O., Haberl, R.L., Lauterbach, K.W., Diener, H.C.: Management patterns and health care use after intracerebral hemorrhage. A cost-of-illness study from a societal perspective in Germany. Cerebrovasc. Dis. (Basel, Switzerland). 15(1–2), 29–36 (2003)
Fattore, G., Torbica, A., Susi, A., Giovanni, A., Benelli, G., Gozzo, M., Toso, V.: The social and economic burden of stroke survivors in Italy: a prospective, incidence-based, multi-centre cost of illness study. BMC Neurol. 12, 137 (2012). https://doi.org/10.1186/1471-2377-12-137
Gerzeli, S., Tarricone, R., Zolo, P., Colangelo, I., Busca, M.R., Gandolfo, C.: The economic burden of stroke in Italy. The EcLIPSE Study: Economic Longitudinal Incidence-based Project for Stroke Evaluation. Neurol. Sci. 26(2), 72–80 (2005). https://doi.org/10.1007/s10072-005-0439-0
Torbica, A., Calciolari, S., Fattore, G.: Does informal care impact utilization of healthcare services? Evidence from a longitudinal study of stroke patients. Soc. Sci. Med. 1982(124), 29–38 (2015). https://doi.org/10.1016/j.socscimed.2014.11.005
van Eeden, M., van Heugten, C., van Mastrigt, G.A., van Mierlo, M., Visser-Meily, J.M., Evers, S.M.: The burden of stroke in the Netherlands: estimating quality of life and costs for 1 year poststroke. BMJ Open. 5(11), e008220 (2015). https://doi.org/10.1136/bmjopen-2015-008220
Andersson, A., Levin, L.A., Oberg, B., Mansson, L.: Health care and social welfare costs in home-based and hospital-based rehabilitation after stroke. Scand. J. Caring Sci. 16(4), 386–392 (2002)
Claesson, L., Linden, T., Skoog, I., Blomstrand, C.: Cognitive impairment after stroke—impact on activities of daily living and costs of care for elderly people. The Goteborg 70+ Stroke Study. Cerebrovasc. Dis. (Basel, Switzerland). 19(2), 102–109 (2005). https://doi.org/10.1159/000082787
von Koch, L., de Pedro-Cuesta, J., Kostulas, V., Almazan, J., Widen Holmqvist, L.: Randomized controlled trial of rehabilitation at home after stroke: one-year follow-up of patient outcome, resource use and cost. Cerebrovasc. Dis. (Basel, Switzerland). 12(2), 131–138 (2001)
Roderick, P., Low, J., Day, R., Peasgood, T., Mullee, M.A., Turnbull, J.C., Villar, T., Raftery, J.: Stroke rehabilitation after hospital discharge: a randomized trial comparing domiciliary and day-hospital care. Age Ageing. 30(4), 303–310 (2001)
Fjaertoft, H., Indredavik, B., Magnussen, J., Johnsen, R.: Early supported discharge for stroke patients improves clinical outcome. Does it also reduce use of health services and costs? One-year follow-up of a randomized controlled trial. Cerebrovasc. Dis. (Basel, Switzerland). 19(6), 376–383 (2005). https://doi.org/10.1159/000085543
Rasmussen, R.S., Ostergaard, A., Kjaer, P., Skerris, A., Skou, C., Christoffersen, J., Seest, L.S., Poulsen, M.B., Ronholt, F., Overgaard, K.: Stroke rehabilitation at home before and after discharge reduced disability and improved quality of life: A randomised controlled trial. Clin. Rehabil. (2015). https://doi.org/10.1177/0269215515575165
Teng, J., Mayo, N.E., Latimer, E., Hanley, J.: Wood-Dauphinee S, Cote R, Scott S. Costs and caregiver consequences of early supported discharge for stroke patients. Stroke J. Cereb. Circ. 34(2), 528–536 (2003)
Funding
This work was supported by the Erasmus-Western Balkans mobility programme (ERAWEB), a project funded by the European Commission. The funding source had no influence on study design, analysis and interpretation of data, in the writing of the manuscript and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Committee
This work was approved by the Research Committee for Scientific and Ethical Questions (RCSEQ), University for Health Sciences, Medical Informatics and Technology (UMIT), Hall in Tirol, Austria (Date: April 26, 2016; reference number: 1697).
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendices
Appendix 1: Evidence tables
Appendix 2
See Table 4.
Appendix 3
Rights and permissions
About this article
Cite this article
Rajsic, S., Gothe, H., Borba, H.H. et al. Economic burden of stroke: a systematic review on post-stroke care. Eur J Health Econ 20, 107–134 (2019). https://doi.org/10.1007/s10198-018-0984-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-018-0984-0