Abstract
Background
The beneficial effects of oral supplements with alkalinizing agents in patients with chronic kidney disease (CKD) have been limited to the severe stages. We investigated whether two types of supplements, sodium bicarbonate (SB) and potassium citrate/sodium citrate (PCSC), could maintain renal function in patients with mild-stage CKD.
Methods
This was a single-center, open-labeled, randomized cohort trial. Study participants with CKD stages G2, G3a, and G3b were enrolled between March 2013 and January 2019 and randomly assigned by stratification according to age, sex, estimated glomerular filtration rate (eGFR), and diabetes. They were followed up for 6 months (short-term study) for the primary endpoints and extended to 2 years (long-term study) for the secondary endpoints. Supplementary doses were adjusted to achieve an early morning urinary pH of 6.8–7.2. We observed renal dysfunction or new-onset cerebrovascular disease and evaluated urinary surrogate markers for renal injury.
Results
Overall, 101 participants were registered and allocated to three groups: standard (n = 32), SB (n = 34), and PCSC (n = 35). Two patients in the standard group attained the primary endpoints (renal stones and overt proteinuria) but were not statistically significant. There was one patient in the standard reduced eGFR during the long-term study (p = 0.042 by ANOVA). SB increased proteinuria (p = 0.0139, baseline vs. 6 months), whereas PCSC significantly reduced proteinuria (p = 0.0061, baseline vs. 1 year, or p = 0.0186, vs. 2 years) and urinary excretion of 8-hydroxy-2′-deoxyguanosine (p = 0.0481, baseline vs. 6 months).
Conclusion
This study is the first to report supplementation of PCSC reduced intrarenal oxidative stress in patients with mild-stage CKD.
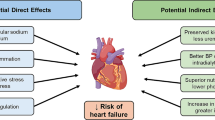
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aciduria is caused by the urinary excretion of acid waste and uremic toxins produced on a daily basis. Metabolic acidosis is a result of renal excretory dysfunction and accumulation of waste and uremic toxins in patients with chronic kidney disease (CKD). Metabolic acidosis is a risk factor for CKD progression and cardiovascular diseases (CVD) [1]. Alkali loads can neutralize metabolic acidosis; however, the reno-protective effects of supplements in patients with CKD are thought to be limited because exogenic alkali loads are excreted very quickly in the urine [2]. Additionally, whether exogenic alkali loads affect renal function remains controversial. Several randomized controlled trials (RCT) on patients with CKD and metabolic acidosis indicated that the chronic administration of sodium bicarbonate (SB) neutralized metabolic acidosis and slowed the decline rate of kidney function [3,4,5,6,7]. One double-blinded RCT study suggested that SB slowed the estimated glomerular filtration rate (eGFR) decline in mild-CKD stages of hypertensive nephropathy [8]; however, other double-blinded RCT studies have not indicated the reno-protective effects in the mild-stages of CKD [9,10,11]. The effect of alkalinizing supplementation on mild-stage CKD remains controversial. One study reported that another alkalinizing supplement, sodium citrate (SC), has reno-protective effects against hypertensive nephropathy [12]. However, RCTs on the effects of oral citrate supplementation in CKD have not yet been conducted.
We hypothesized that chronic oral alkalinizing supplementation could preserve the renal function in mild-stage CKD by monitoring the urinary pH and evaluating surrogate markers, including the intrarenal reactive oxygen species (ROS), to predict the associated renal dysfunction.
Methods
Study design and patient registration
This single-center, open-label, randomized cohort trial was named Oral ALkalizers in patients with Chronic Kidney disease (CKOALA study). The detailed study protocol has been published previously [13]. Two oral alkalinizing supplements, SB and potassium citrate/sodium citrate (PCSC), were used. Metabolic acidosis is defined as a serum bicarbonate level < 22 mEq/L with normal respiratory function, which is usually recognized in the severe stages of CKD with hyperpotassemia [14]. Therefore, we enrolled patients with mild-stage CKD to avoid the severe adverse effects of hyperkalemia because the PCSC included potassium. Patients aged 20–80 years with CKD stages G2, G3a, and G3b were recruited at the Tohoku University Hospital. The registered patients were layered using four variables: age (≥ 65, < 65 years old), sex, presence of diabetes mellitus, and estimated creatinine glomerular filtration rate (eGFR), ≥ 46 or < 46 mL/min/1.73 m2). All patients were randomly allocated to three groups using a computer method: standard, SB, and PCSC. Sex was self-reported during the first visit. SB or PCSC was started at 1.5 g per day. These drugs have been approved for the treatment of acidosis and hyperuricemia in Japan. When the early morning urinary pH (mUpH) was < 6.5, the agent dose was increased to 3.0 g per day. When the early mUpH was > 7.2, the dose was decreased to that of mUpH < 6.5. mUpH was measured using a urinary pH meter (LAQUAtwin pH sensor S010, HORIBA Ltd., Kyoto, Japan). All the registered patients provided written informed consent. The patients were followed up at baseline, 6 weeks (6W), 12 weeks (12W), and 6 months (6 M) for the short-term study. Patients who completed the short-term study were reconsented at 6 months to continue the long-term study for an additional 1 year (1Y) to 2 years (2Y). The exclusion criteria were as follows: eating and drinking abundant amounts of alkalinizing substances, taking tolvaptan, renal hypouricemia, hyperkalemia, diabetes insipidus, hypernatremia of unknown origin, untreated mUpH > 6.8, serious urinary tract infection, and serious complications of heart and liver disease.
Data collection and sample assay
The performance status, venous blood tests, spot urine tests, venous blood gas tests, serum creatinine (sCr), eGFR of rate (eGFR-Cr) of creatinine, proteinuria (UP), urinary excretion of albumin (UAE), and N-acetyl-beta-d-glucosaminidase (UNAG) were performed at the central laboratory of Tohoku University Hospital. For other urinary surrogate biomarkers, alfa1-microglobulin (UaMG, mg/L) and type IV collagen (U4Col) were measured at the SRL Laboratory (SRL, Inc., Tokyo, Japan). L-type fatty acid binding protein (ULFABP), neutrophil gelatinase-associated lipocalin (UNGAL), kidney injury molecule-1 (UKIM-1), transforming growth factor-beta (UTGFb), endothelin-1 (UET-1), angiotensinogen (UANG), monocyte chemotactic protein-1 (UMCP-1), interleukin-6 (UIL-6), aldosterone (UAldo) and lactate (ULac) were measured at Safety Research Institute for Chemical Compounds Co., Ltd. (Sapporo, Japan). For intrarenal ROS assays, 8-isoprostane (U8IsoP) and 8-hydroxy-2′-deoxyguanosine (U8OHdG) were measured at NIKKEN SEIL Co., Ltd. (Shizuoka, Japan). The Health Related Quality of Life Short Form 8TM Health Survey © (SF8) was licensed to the Institute for Health Outcomes and Process Evaluation research (iHope International, Kyoto, Japan) for the evaluation of individual performances. The renal function of eGFR was calculated using the following equation: eGFR-Cr = 194 × Cr−1.094 × age−0.287 for men, or 194 × Cr−1.094 × age−0.287 × 0.739 for women [15]. All samples at every visit were stored at –80 °C for subsequent analysis of urinary surrogate biomarkers.
Endpoints
The primary endpoints were the development of significant renal dysfunction as follows; (1) sCr level ≥ 1.5 × higher than that of baseline, (2) eGFR decrease ≥ 20 mL/min/1.73 m2 from baseline, (3) UP ≥ 3.5 g/gCr (overt), and (4) new development of urinary stones or the occurrence of CVD during the short-term study. The secondary endpoints were the same items as the primary endpoints at 1 and 2 years and the exploratory research of surrogate biomarkers associated with the reno-protective effects of the interventions.
Statistical analysis
The ideal estimated sample size of 50 participants in each group was to achieve the level of significance (i.e. type-1 error rate) of 5% (α = 0.05) and the statistical power of 80% (β = 0.2) with the equally allocated three groups referring to previous studies [3] as described previously [16]. However, two earlier separate studies of patients suggested the need for 33–36 patients in each of the three groups to achieve sufficient power to detect the eGFR benefit of the interventions by SB, SC, or fruits and vegetables (FV) among the groups compared with the control group [7, 12]. Therefore, we changed the registration period to 5 years, and the target number was approximately 35 for each group; the modified protocol was also approved by the Ethics Committee.
For the intention-to-treat analysis, the collection and management of the data was conducted by an individual data management team at the Clinical Research Data Center of Tohoku University Hospital. First, the appearance rates of primary endpoints at 6W, 12W, and 6 M during each treatment were compared with the standard (Student’s t-test). Second, changes in the renal function (sCr, eGFR-Cr, and UP) were compared using a paired t-test between each visit value and baseline for each group, or the Wilcoxon test among the three groups at each visit. An analysis of variance (ANOVA) was used for the secondary endpoints. Changes in other urinary surrogate markers and quality of life with SF-8 were analyzed using a paired t-test or Wilcoxon test using the same method. The significance of comparison among the three groups was p < 0.0167 for adapting Bonferroni correction, and the other was p < 0.05.
Efficacy was analyzed for the intention-to-treat population, that is the group of randomized subjects who received at least one dose of the study drug and underwent at least one post-drug efficacy assessment. Safety was analyzed in all patients who received at least one dose of the study drug. All statistical analyses were performed using Windows SAS software (version 9.4; SAS Institute, Cary, NC, USA).
Ethical matters
The trial was conducted in accordance with the Good Clinical Practice guidelines of the International Council for Harmonization and the ethical principles of the Declaration of Helsinki. Written informed consent was obtained from all patients. The Ethics Committee of Tohoku University Hospital approved this trial protocol (IRB2012-2–100-1 and CRB2200003). All registered data were monitored by independent central reviewers throughout the study.
Trial registration
The trial was registered on February 26, 2013 (UMIN-CTR 000010059), and March 26, 2019 (jRCTs 021180043).
Results
Patients and basal characteristics
A total of 101 patients [age (mean ± SD) 61.6 ± 11.5 years] with CKD stages G2, G3a, and G3b were registered between April 2013 and March 2018. As shown in Figure, the patients were allocated into three groups: standard (n = 31), SB (n = 32), and PCSC (n = 32). Six registered patients withdrew consent due to research anxieties or surgeries for worsened comorbidities before starting administration (Standard 1, SB 2, and PCSC 3). Four patients dropped out during the short-term study period (SB 1 and PCSC 3). In a long-term study, only 29 patients reconsented at 6 M (standard 4, SB 12, and PCSC, 13). The most common reason for this disagreement is the desire to consume alkalinizing supplements. Four patients dropped out after 2Y (standard 1, SB 2, and PCSC 1). No severe intervention-related adverse events were observed.
No differences in age, sex, medications, medical history, or malignancies that developed within 5 years were observed among the three groups (Table 1). The baseline physiological findings and blood and urine examinations were not significantly different among the three groups (Table 2).
Primary endpoints
There was no significant difference in the sCr and eGFR-Cr among the three groups at 6 months [sCr (g/dL, mean ± SE); Standard 1.13 ± 0.06, SB 0.98 ± 0.04, PCSC 1.08 ± 0.05: eGFR-Cr (mL/min/1.73 m2); Standard 52.0 ± 2.84, SB 58.1 ± 2.35, PCSC 52.8 ± 2.10]. None of the groups showed a significant increase in renal function from the baseline (Table 3).
One patient experienced overt UP after 6 weeks compared with that at baseline (from 3.17 g/gCr to 4.02), and one patient developed newly onset renal stones at 6 months in the standard group; however, renal dysfunction was not significantly different among the three groups (Tables 3 and 4). No new CVD complications occurred.
Secondary endpoints
Only 29 patients were included in the long-term study: Standard (n = 4), SB (n = 12), and PCSC (n = 13). Twelve patients in the SB and PCSC groups dropped out because they moved to nearby medical clinics (Fig. 1).
The renal function and urinary surrogate marker results are shown in Table 4. Longitudinal comparisons of sCr and eGFR-Cr showed significant differences among the three groups (p = 0.0166 for sCr and p = 0.042 for eGFR-Cr by ANOVA). UP significantly increased at 6 M compared with baseline in SB (p = 0.0139), but significantly decreased at 1Y and 2Y in PCSC (p = 0.0061 and p = 0.0186, respectively). The U4Col levels were significantly different among the three groups in the longitudinal comparison (p = 0.046). A significant increase in the mUpH was observed at 6 M and 2Y compared with baseline in PCSC (p = 0.0102 and p = 0.0385, respectively), and there were significant differences at 6 M among the three groups (p = 0.0078). Both alkalinizing supplements increased the mUpH. UAE significantly increased at 12W compared to baseline in SB (p = 0.0325). 8OHdG significantly increased at 6W in the SB group (p = 0.0393) compared to baseline and deceased at 6 M in PCSC (p = 0.0481). UET1 at 6 M was significantly different among the three groups (p = 0.00469), and both alkalinizing supplements increased the UET1. ULac at 6 M significantly decreased compared to baseline in standard (p = 0.0221) and increased in PCSC (p = 0.0016). Other urinary surrogate markers were not significantly different among the three groups, and longitudinal comparisons were performed within each group. The SF-8 values after the alkalization of the supplements were not significantly different from those in the standard group (Table 3).
The number of reconsulted patients after the short-term study was small; however, PSCS might suppress urinary excretion of 8OHdG at 1Y and 2Y compared with baseline (p = 0.0020 and p = 0.0137; Table 4). The most common reason was that taking PCSC made one feel better; however, there were no differences in performance status (Table 3).
Discussion
We investigated the chronic effects of preserving renal function in mild-stage CKD by neutralizing metabolic acidosis and aciduria (UMIN-CTR 000010059, jRCTs 021180043). We found that a citrate compound of PCSC suppressed the intrarenal ROS. It is also unique that the doses of the alkali loads were adjusted by monitoring the mUpH.
In this study, the progression of renal stones and overt proteinuria occurred in the standard group, but not in the alkalinizing group. PCSC had some reno-protective effects on eGFR-Cr and UP at the secondary endpoints; however, unexpectedly, SB was rather negative. We previously demonstrated that orally administered SB is quickly excreted in the urine and prevents renal injury by suppressing the intrarenal ROS stimulated by both albuminuria and aciduria in vivo [16]. Notably, SB was not effective on the surrogate biomarker for ROS (U8IsoP, 8OHdG, U4Col, UTGFb, and UANG); however, PCSC had protective effects on 8OHdG and U4Col. The relevant suppression of renal ROS by PCSC could be considered as the mechanism of the reno-protective effect. Coincidentally, the results of 8OHdG in the PCSC group tended to be higher than those in the standard and SB groups. The matching factors at registration were age, sex, eGFR, and diabetes status. The urinary biomarkers at baseline could not be matched, and could not be analyzed among the groups. Nevertheless, the reno-protective effects of SB are still controversial. The oral administration of SB or the base produced from FV increased the serum bicarbonate levels and slowed renal dysfunction in patients with CKD with definite metabolic acidosis [14]. Systemic reviews report that SB slowed the decline rate of eGFR [17, 18]. In a series of RCT studies resulting in SB-protected renal functions, the recruited patients had severe stages of CKD with metabolic acidosis [3,4,5]. In these studies, the inclusion criteria were sufficiently low bicarbonate concentrations (< 21–22 mEq/L), and the participants achieved a target serum bicarbonate concentration of up to 24–28 mmol/L after SB administration. Furthermore, SB improved chronic heart failure and mortality [3] cardiovascular risk [17], and preserved muscle mass [5]. In our study, 8OHdG was significantly increased at 6W and 12W but returned to the basal level at 6 M in the SB group. The intratubular load of high sodium increased the renal oxidative stress from tubular cells by increasing the intracellular transportation of sodium [19, 20] and neutralizing acid conditions of tubules suppressed renal oxidative stress [16]. The effects of SB might be biphasic, sodium loading effects were acutely seen at 6W and 12W, and acid-neutralizing effects by bicarbonate appeared chronically. Thus, SB may have partial reno-protective effects.
We found that the new phenomena that PCSC did not alter 8IsoP, despite a reduction in 8OHdG. A previous study reported that chronic oxidative stress caused by radiation nephropathy increases the urinary excretion of 8-OHdG, but not 8-isoprostane, because they are produced through different pathways, namely DNA oxidation and lipid peroxidation [21]. Another study showed that some citrate-rich fruit extracts stimulated the secretion of prostaglandin E2 in vitro[22]. It is possible that PCSC can suppress renal and/or systemic oxidative stress; however, it simultaneously increases the arachidonic acid levels by citrate. Further studies are needed to test this hypothesis.
To evaluate the effect of proteinuria in patients with CKD associated with urinary excretion of sodium and potassium and the ratio of urinary sodium and potassium excretion (Supplemental Table 1), proteinuria was significantly positively related to sodium and potassium loading only in the SB group, and the effects of urinary sodium or potassium against proteinuria were analyzed (Supplemental Table 2). The reason for this was considered to be that the loading of sodium in the tubules stimulates the production of superoxide anions through the activation of Na/K-ATPase [19]. However, in the PSCS group, the loading of both sodium and potassium was not related to proteinuria. Citrate and/or potassium could attenuate renal injuries caused by sodium but by unknown mechanisms. In future clinical studies, we plan to evaluate the candidate surrogate biomarkers identified in this study precisely.
Patients with severe chronic CKD were excluded. We utilized aciduria (pH < 6.5), including an incision criterion, and the alkali loads were adjusted according to the mUpH levels, but not the serum bicarbonate concentrations. We considered urinary pH as a better index to understand metabolic acidosis because excessive amounts of alkali loads are excreted in the urine [14, 15]. Notably, PCSC significantly increased the mUpH levels but not BS because it was considered that BS was excreted more immediately than PCSC and could not be reflected in the urine the following morning. Additionally, the baseline bicarbonate concentrations in this study were relatively higher (25.7 ± 2.75 mEq/L). Some RCT studies of SB had negative results because patients with low-grade metabolic acidosis (baseline SB of approximately 24 mEq/L) were enrolled [9,10,11]. This was thought to be the reason why alkali loads are easily buffered and excreted in mild-stage CKD. Nevertheless, PCSC prevented renal function deterioration. In another study, SC preserved the eGFR of cystatin C (CysC) more than eGFR-Cr [12]. A meta-analysis demonstrated that the serum Cr/CysC ratio was positively correlated with muscle mass and strength [23]. The intake of FV-containing citrate was observed to preserve renal function [6, 7, 14]. A notable crossover double-blind study on SC supplementation reported improved tennis performance and reduced fatigue [24]. A different citrate compound, potassium citrate, has been reported to increase serum bicarbonate levels and bone mineral density [25]. Citrate is a major substrate of the tricarboxylic acid cycle in mitochondria, and citrate compounds can metabolically exert organ-protective effects.
Limitations
This study has several limitations. This was a single-center study that only included Japanese patients, and the enrolled participants were limited to those with mild-CKD stages, including patients with pyuria. After identifying the available surrogate biomarker candidates, they must be precisely addressed and evaluated in future clinical studies. To reveal the reno-protective effects of alkalinizing supplements, we need a larger number of participants for further studies because alkali loads are easily influenced by daily foods and beverages.
Conclusion
This study is the first to report that the alkalinizing supplementation of PCSC-reduced intrarenal reactive oxygen species in patients with mild-stage CKD. To demonstrate that citrate supplementation prevents the progression of renal dysfunction in patients with CKD, we conducted a cohort study that additionally matched the renal oxidative stress before random stratification.
References
Adamczak M, Surma S. Metabolic acidosis in patients with CKD: epidemiology, pathogenesis, and treatment. Kidney Dis. 2021;7:452–67.
Hamm LL, Nakhoul N, Hering-Smith KS. Acid-b homeostasis. Clin J Am Soc Nephrol. 2015;10:2232–42.
de Brito-Ashurst I, Varagunam M, Raftery MJ, Yaqoob MM. Bicarbonate supplementation slows progression of CKD and improves nutritional status. J Am Soc Nephrol. 2009;20:2075–84.
Di Iorio BR, Bellasi A, Raphael KL, et al. Treatment of metabolic acidosis with sodium bicarbonate delays progression of chronic kidney disease: the UBI Study. J Nephrol. 2019;32:989–1001.
Dubey AK, Sahoo J, Vairappan B, et al. Correction of metabolic acidosis improves muscle mass and renal function in chronic kidney disease stages 3 and 4: a randomized controlled trial. Nephrol Dial Transplant. 2020;35:121–9.
Goraya N, Simoni J, Jo CH, Wesson DE. Treatment of metabolic acidosis in patients with stage 3 chronic kidney disease with fruits and vegetables or oral bicarbonate reduces urine angiotensinogen and preserves glomerular filtration rate. Kidney Int. 2014;86:1031–8.
Goraya N, Munoz-Maldonado Y, Simoni J, et al. Fruit and vegetable treatment of chronic kidney disease-related metabolic acidosis reduces cardiovascular risk better than sodium bicarbonate. Am J Nephrol. 2019;49:438–48.
Mahajan A, Simoni J, Sheather SJ, et al. Daily oral sodium bicarbonate preserves glomerular filtration rate by slowing its decline in early hypertensive nephropathy. Kidney Int. 2010;78:303–9.
BiCARB study group. Clinical and cost-effectiveness of oral sodium bicarbonate therapy for older patients with chronic kidney disease and low-grade acidosis (BiCARB): a pragmatic randomised, double-blind, placebo-controlled trial. BMC Med. 2020;18:91.
Raphael KL, Isakova T, Ix JH, et al. A randomized trial comparing the safety, adherence, and pharmacodynamics profiles of two doses of sodium bicarbonate in CKD: the BASE pilot trial. J Am Soc Nephrol. 2020;31:161–74.
Melamed ML, Horwitz EJ, Dobre MA, et al. Effects of sodium bicarbonate in CKD stages 3 and 4: a randomized, placebo-controlled, multicenter clinical trial. Am J Kidney Dis. 2020;75:225–34.
Phisitkul S, Khanna A, Simoni J, et al. Amelioration of metabolic acidosis in patients with low GFR reduced kidney endothelin production and kidney injury, and better preserved GFR. Kidney Int. 2010;77:617–23.
Abe M, Akaishi T, Shoji M, CKOALA study group, et al. Reno-protective effects of oral alkalizing agents in chronic kidney disease with aciduria: protocol for a randomized cohort study. BMC Nephrol. 2020;21:144.
Goraya N, Narayanan M, Wesson DE. Management of metabolic acidosis in chronic kidney disease: past, present, and future direction. Adv Chronic Kidney Dis. 2022;29:416–23.
Matsuo S, Imai E, Horio M, Collaborators developing the Japanese equation for estimated GFR, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Souma T, Abe M, Moriguchi T, et al. Luminal alkalinization attenuates proteinuria-induced oxidative damage in proximal tubular cells. J Am Soc Nephrol. 2011;22:635–48.
Kim HJ. Metabolic acidosis in chronic kidney disease: pathogenesis, clinical consequences, and treatment. Electrolyte Blood Press. 2021;19:29–37.
Cheng F, Li Q, Wang J, et al. The effects of oral sodium bicarbonate on renal function and cardiovascular risk in patients with chronic kidney disease: a systematic review and meta-analysis. Ther Clin Risk Manag. 2021;17:1321–31.
Abe M, Kaldunski M, Liang M, et al. Effect of sodium delivery on superoxide and nitric oxide in the medullary thick ascending limb. Am J Physiol Renal Physiol. 2006;291:F350–7.
Cowley AW Jr, Abe M, Mori T, et al. Reactive oxygen species as important determinants of medullary flow, sodium excretion and hypertension. Am J Physiol Renal Physiol. 2015;308:F179–97.
Lenarczyk M, Cohen EP, Fish BL, et al. Chronic oxidative stress as a mechanism for radiation nephropathy. Radiat Res. 2009;171:164–72.
Na JR, Kim E, Na CS, Kim S. Citric acid-enriched extract of ripe Prunus mume (Siebold) Siebold & Zucc induces laxative effects by regulating the expression of aquaporin 3 and prostaglandin E(2) in rats with loperamide-induced constipation. J Med Food. 2022;25:12–23.
Zheng WH, Zhu YB, Yao Y, Huang HB. Serum creatinine/cystatin C ratio as a muscle mass evaluating tool and prognostic indicator for hospitalized patients: a meta-analysis. Front Med (Lausanne). 2023;9:1058464.
Cunha VCR, Aoki MS, Zourdos MC, et al. Sodium citrate supplementation enhances tennis skill performance: a crossover, placebo-controlled, double-blind study. J Int Soc Sports Nutr. 2019;16:32.
Domrongkitchaiporn S, Pongskul C, Sirikulchayanonta V, et al. Bone histology and bone mineral density after correction of acidosis in distal renal tubular acidosis. Kidney Int. 2002;62:2160–6.
Acknowledgements
We thank all the members of the CKOALA study group: Tomokazu Souma, Keisuke Nakayama, Masataka Kudo, Rei Morimoto, Takashi Nakamichi, Susumu Ogawa, Takehiro Numata, Tetsuya Sakurai, Takanori Mizuno, Reiko Kokubun, Mutsumi Shoji, Miyuki Endo, Kotoha Sasaki, Toshiko Osada, Maki Kamada, Dan Sato, Daisuke Saigusa, Junichi Tanaka, Fumitoshi Satoh, and former professors Hideyasu Kiyomoto, Hiroshi Sato, and Sadayoshi Ito. We would like to thank Mr. Dennis Nishimura and Editage (www.editage.jp) for English language proofreading.
Funding
JSPS KAKENHI, grant numbers (C) 16K08487 and (C) 22K11849. A collaborative research fund was obtained from Nippon Chemiphar Co., Ltd.
Author information
Authors and Affiliations
Consortia
Contributions
MA designed the protocol and was responsible for the study. ST, AM, RA, KI, MM, TAb, and TT provided the clinical registrations. TY and UM contributed to the data analysis and advice. SK, TN, KN, SY, KK, TK, and TAk technically assisted with the research procedure and assayed the samples. TI advised and supported this. All authors vouched for the accuracy and completeness of the data and the fidelity of the trial to the protocol.
Corresponding author
Ethics declarations
Conflicts of interest
Nippon Chemiphar Co., Ltd.
Ethics approval and consent to participate
All the study procedures were approved by the Institutional Review Board of Tohoku University Hospital (IRB2012-2–100-1, CRB2200003) and were performed in compliance with the Declaration of Helsinki of 1964 and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Abe, M., Yamaguchi, T., Koshiba, S. et al. Oral alkalinizing supplementation suppressed intrarenal reactive oxidative stress in mild-stage chronic kidney disease: a randomized cohort study. Clin Exp Nephrol (2024). https://doi.org/10.1007/s10157-024-02517-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10157-024-02517-3