Abstract
Background
Serum lactate dehydrogenase to albumin ratio (LAR) is associated with poor outcomes in malignancy and pneumonia. However, there are few studies suggesting that LAR is associated with the occurrence of acute kidney injury (AKI) in patients with sepsis, which was investigated in this study.
Methods
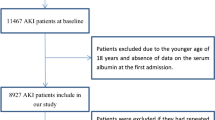
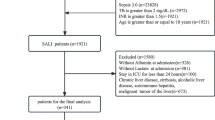
We conducted a retrospective cohort study based on the Medical Information Mart for Intensive Care (MIMIC)-IV database. The primary outcome was the occurrence of AKI within 2 days and 7 days. Multivariable logistic regression models were used to calculate odds ratios to validate the association between LAR and AKI, in-hospital mortality, RRT use, and recovery of renal function, respectively.
Results
A total of 4010 participants were included in this study. The median age of the participants was 63.5 years and the median LAR was 10.5. After adjusting for confounding variables, patients in the highest LAR quartile had a higher risk of AKI than those in the lowest LAR quartile within 2 days and 7 days, with odds ratios of 1.37 (95% confidence interval [CI]: 1.23–1.52) and 1.95 (95% CI: 1.72–2.22), respectively. The adjusted odds of AKI within 2 and 7 days were 1.16 (95% CI: 1.12–1.20) and 1.29 (95% CI: 1.24–1.35) for each 1 unit increase in LAR(log2), respectively.
Conclusion
This study demonstrated that elevated LAR was associated with poor prognosis in patients with sepsis. The risk of AKI and in-hospital mortality increased, the need for RRT increased, and the chance of recovery of renal function decreased with the increase of LAR.




Similar content being viewed by others
References
Basile DP, Anderson MD, Sutton TA. Pathophysiology of acute kidney injury. Compr Physiol. 2012;2(2):1303–53. https://doi.org/10.1002/cphy.c110041.
Harrois A, Grillot N, Figueiredo S, Duranteau J. Acute kidney injury is associated with a decrease in cortical renal perfusion during septic shock. Crit Care. 2018;22(1):161. https://doi.org/10.1186/s13054-018-2067-0.
Mehta RL, Bouchard J, Soroko SB, Ikizler TA, Paganini EP, Chertow GM, et al. Sepsis as a cause and consequence of acute kidney injury: program to improve care in acute renal disease. Intensive Care Med. 2011;37(2):241–8. https://doi.org/10.1007/s00134-010-2089-9.
Rabb H, Griffin MD, McKay DB, Swaminathan S, Pickkers P, Rosner MH, et al. Inflammation in AKI: current understanding, key questions, and knowledge gaps. J Am Soc Nephrol. 2016;27(2):371–9. https://doi.org/10.1681/ASN.2015030261.
Fiaccadori E, Cremaschi E. Nutritional assessment and support in acute kidney injury. Curr Opin Crit Care. 2009;15(6):474–80. https://doi.org/10.1097/MCC.0b013e328332f6b2.
Lu J, Wei Z, Jiang H, Cheng L, Chen Q, Chen M, et al. Lactate dehydrogenase is associated with 28-day mortality in patients with sepsis: a retrospective observational study. J Surg Res. 2018;228:314–21. https://doi.org/10.1016/j.jss.2018.03.035.
Aday U, Boyuk A, Akkoc H. The prognostic significance of serum lactate dehydrogenase-to-albumin ratio in colorectal cancer. Ann Surg Treat Res. 2020;99(3):161–70. https://doi.org/10.4174/astr.2020.99.3.161.
Lee BK, Ryu S, Oh SK, Ahn HJ, Jeon SY, Jeong WJ, et al. Lactate dehydrogenase to albumin ratio as a prognostic factor in lower respiratory tract infection patients. Am J Emerg Med. 2022;52:54–8. https://doi.org/10.1016/j.ajem.2021.11.028.
Green H, Tobar A, Gafter-Gvili A, Leibovici L, Klein T, Rahamimov R, et al. Serum lactate dehydrogenase is elevated in ischemic acute tubular necrosis but not in acute rejection in kidney transplant patients. Prog Transplant. 2017;27(1):53–7. https://doi.org/10.1177/1526924816664089.
Bennett MR, Nehus E, Haffner C, Ma Q, Devarajan P. Pediatric reference ranges for acute kidney injury biomarkers. Pediatr Nephrol. 2015;30(4):677–85. https://doi.org/10.1007/s00467-014-2989-y.
Zhang D, Shi L. Serum lactate dehydrogenase level is associated with in-hospital mortality in critically Ill patients with acute kidney injury. Int Urol Nephrol. 2021;53(11):2341–8. https://doi.org/10.1007/s11255-021-02792-z.
Yu MY, Lee SW, Baek SH, Na KY, Chae DW, Chin HJ, et al. Hypoalbuminemia at admission predicts the development of acute kidney injury in hospitalized patients: a retrospective cohort study. PLoS ONE. 2017;12(7):e0180750. https://doi.org/10.1371/journal.pone.0180750.
Lee EH, Baek SH, Chin JH, Choi DK, Son HJ, Kim WJ, et al. Preoperative hypoalbuminemia is a major risk factor for acute kidney injury following off-pump coronary artery bypass surgery. Intensive Care Med. 2012;38(9):1478–86. https://doi.org/10.1007/s00134-012-2599-8.
Jeon SY, Ryu S, Oh SK, Park JS, You YH, Jeong WJ, et al. Lactate dehydrogenase to albumin ratio as a prognostic factor for patients with severe infection requiring intensive care. Medicine (Baltimore). 2021;100(41):e27538. https://doi.org/10.1097/MD.0000000000027538.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. https://doi.org/10.1016/j.ijsu.2014.07.013.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10. https://doi.org/10.1001/jama.2016.0287.
Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function–measured and estimated glomerular filtration rate. N Engl J Med. 2006;354(23):2473–83. https://doi.org/10.1056/NEJMra054415.
Ricci Z, Romagnoli S. Acute kidney injury: diagnosis and classification in adults and children. Contrib Nephrol. 2018;193:1–12. https://doi.org/10.1159/000484956.
Zhao GJ, Xu C, Ying JC, Lu WB, Hong GL, Li MF, et al. Association between furosemide administration and outcomes in critically ill patients with acute kidney injury. Crit Care. 2020;24(1):75. https://doi.org/10.1186/s13054-020-2798-6.
Panitchote A, Mehkri O, Hastings A, Hanane T, Demirjian S, Torbic H, et al. Clinical predictors of renal non-recovery in acute respiratory distress syndrome. BMC Nephrol. 2019;20(1):255. https://doi.org/10.1186/s12882-019-1439-2.
Kellum JA, Sileanu FE, Murugan R, Lucko N, Shaw AD, Clermont G. Classifying AKI by urine output versus serum creatinine level. J Am Soc Nephrol. 2015;26(9):2231–8. https://doi.org/10.1681/ASN.2014070724.
Siew ED, Peterson JF, Eden SK, Moons KG, Ikizler TA, Matheny ME. Use of multiple imputation method to improve estimation of missing baseline serum creatinine in acute kidney injury research. Clin J Am Soc Nephrol. 2013;8(1):10–8. https://doi.org/10.2215/CJN.00200112.
Chen Y, Feng F, Li M, Yuan JJ, Chang XN, Wei BH, et al. Relationship between platelet/lymphocyte ratio and prognosis of patients with septic acute kidney injury: a pilot study. J Chin Med Assoc. 2020;83(11):1004–7. https://doi.org/10.1097/JCMA.0000000000000404.
Chen JJ, Kuo G, Fan PC, Lee TH, Yen CL, Lee CC, et al. Neutrophil-to-lymphocyte ratio is a marker for acute kidney injury progression and mortality in critically ill populations: a population-based, multi-institutional study. J Nephrol. 2022;35(3):911–20. https://doi.org/10.1007/s40620-021-01162-3.
Xiao W, Lu Z, Liu Y, Hua T, Zhang J, Hu J, et al. Influence of the initial neutrophils to lymphocytes and platelets ratio on the incidence and severity of sepsis-associated acute kidney injury: a double robust estimation based on a large public database. Front Immunol. 2022;13:925494. https://doi.org/10.3389/fimmu.2022.925494.
Feng JF, Wang L, Yang X, Jiang YH. Prognostic value of lactate dehydrogenase to albumin ratio (LAR) in patients with resectable esophageal squamous cell carcinoma. Cancer Manag Res. 2019;11:7243–51. https://doi.org/10.2147/CMAR.S208320.
Xie Z, Zhou H, Wang L, Wu Y. The Significance of the preoperative lactate dehydrogenase/albumin ratio in the prognosis of colon cancer: a retrospective study. PeerJ. 2022;10:e13091. https://doi.org/10.7717/peerj.13091.
Liang M, Ren X, Huang D, Ruan Z, Chen X, Qiu Z. The association between lactate dehydrogenase to serum albumin ratio and the 28 day mortality in patients with sepsis-associated acute kidney injury in intensive care: a retrospective cohort study. Ren Fail. 2023;45(1):2212080. https://doi.org/10.1080/0886022X.2023.2212080.
Deng Y, Li X, Lai Q, Wang F, Zhang C, Yang Y, et al. Prognostic implication of lactic dehydrogenase-to-albumin ratio in critically ill patients with acute kidney injury. Clin Exp Nephrol. 2023;27(4):349–57. https://doi.org/10.1007/s10157-023-02321-5.
Prowle JR, Liu YL, Licari E, Bagshaw SM, Egi M, Haase M, et al. Oliguria as predictive biomarker of acute kidney injury in critically ill patients. Crit Care. 2011;15(4):R172. https://doi.org/10.1186/cc10318.
Priyanka P, Zarbock A, Izawa J, Gleason TG, Renfurm RW, Kellum JA. The impact of acute kidney injury by serum creatinine or urine output criteria on major adverse kidney events in cardiac surgery patients. J Thorac Cardiovasc Surg. 2021;162(1):143-51 e7. https://doi.org/10.1016/j.jtcvs.2019.11.137.
Bianchi NA, Stavart LL, Altarelli M, Kelevina T, Faouzi M, Schneider AG. Association of oliguria with acute kidney injury diagnosis, severity assessment, and mortality among patients with critical illness. JAMA Netw Open. 2021;4(11):e2133094. https://doi.org/10.1001/jamanetworkopen.2021.33094.
Zavada J, Hoste E, Cartin-Ceba R, Calzavacca P, Gajic O, Clermont G, et al. A comparison of three methods to estimate baseline creatinine for RIFLE classification. Nephrol Dial Transplant. 2010;25(12):3911–8. https://doi.org/10.1093/ndt/gfp766.
Siew ED, Matheny ME, Ikizler TA, Lewis JB, Miller RA, Waitman LR, et al. Commonly used surrogates for baseline renal function affect the classification and prognosis of acute kidney injury. Kidney Int. 2010;77(6):536–42. https://doi.org/10.1038/ki.2009.479.
Zeng X, McMahon GM, Brunelli SM, Bates DW, Waikar SS. Incidence, outcomes, and comparisons across definitions of AKI in hospitalized individuals. Clin J Am Soc Nephrol. 2014;9(1):12–20. https://doi.org/10.2215/CJN.02730313.
Fani F, Regolisti G, Delsante M, Cantaluppi V, Castellano G, Gesualdo L, et al. Recent advances in the pathogenetic mechanisms of sepsis-associated acute kidney injury. J Nephrol. 2018;31(3):351–9. https://doi.org/10.1007/s40620-017-0452-4.
Mandavia CH, Aroor AR, Demarco VG, Sowers JR. Molecular and metabolic mechanisms of cardiac dysfunction in diabetes. Life Sci. 2013;92(11):601–8. https://doi.org/10.1016/j.lfs.2012.10.028.
Akchurin OM, Kaskel F. Update on inflammation in chronic kidney disease. Blood Purif. 2015;39(1–3):84–92. https://doi.org/10.1159/000368940.
Lasry A, Zinger A, Ben-Neriah Y. Inflammatory networks underlying colorectal cancer. Nat Immunol. 2016;17(3):230–40. https://doi.org/10.1038/ni.3384.
Berbudi A, Rahmadika N, Tjahjadi AI, Ruslami R. Type 2 diabetes and its impact on the immune system. Curr Diabetes Rev. 2020;16(5):442–9. https://doi.org/10.2174/1573399815666191024085838.
Shen X, Lv K, Hou B, Ao Q, Zhao J, Yang G, et al. Impact of diabetes on the recurrence and prognosis of acute kidney injury in older male patients: a 10 year retrospective cohort study. Diabetes Ther. 2022;13(11–12):1907–20. https://doi.org/10.1007/s13300-022-01309-w.
Ratliff BB, Abdulmahdi W, Pawar R, Wolin MS. Oxidant mechanisms in renal injury and disease. Antioxid Redox Signal. 2016;25(3):119–46. https://doi.org/10.1089/ars.2016.6665.
Patil NK, Parajuli N, MacMillan-Crow LA, Mayeux PR. Inactivation of renal mitochondrial respiratory complexes and manganese superoxide dismutase during sepsis: mitochondria-targeted antioxidant mitigates injury. Am J Physiol Renal Physiol. 2014;306(7):F734–43. https://doi.org/10.1152/ajprenal.00643.2013.
Miao P, Sheng S, Sun X, Liu J, Huang G. Lactate dehydrogenase a in cancer: a promising target for diagnosis and therapy. IUBMB Life. 2013;65(11):904–10. https://doi.org/10.1002/iub.1216.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
WX and JJ designed this study. JX, QH and TZ conducted the collection and analysis of data. WX drafted the manuscript. JH, GC and JM analyzed and interpreted the results. All authors have reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors have declared no competing interest.
Ethical approval
The Institutional Review Boards of the Massachusetts Institute of Technology exempted the MIMIC IV database from ethics review, given that patient information was hidden to protect privacy.
Informed consent
Not applicable
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Xu, W., Huo, J., Hu, Q. et al. Association between lactate dehydrogenase to albumin ratio and acute kidney injury in patients with sepsis: a retrospective cohort study. Clin Exp Nephrol (2024). https://doi.org/10.1007/s10157-024-02500-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10157-024-02500-y