Abstract
Aim
The nutritional risk index for Japanese hemodialysis (NRI-JH) is a nutritional screening tool for predicting mortality in patients undergoing hemodialysis; however, its utility in patients undergoing hemodialysis during long-term hospitalization who have a high risk of protein-energy wasting, is unclear.
Methods
This retrospective study assessed hospitalized patients undergoing hemodialysis during long-term care at a single hospital. The NRI-JH was calculated using body mass index, serum albumin level, total cholesterol level, and serum creatinine level. The patients were categorized into three risk groups—low, medium, and high. Dietary energy and protein intake were evaluated by dietitians. The association of NRI-JH risk with nutritional intake and mortality were examined.
Results
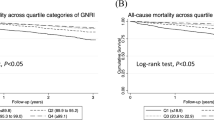
In total, 133 patients were analyzed. The NRI-JH risk was low in 24%, medium in 26%, and high in 50% of the patients. The patients in the high-risk group were older and had lower energy and protein intakes than those in the low- and medium-risk groups. High-risk patients showed shorter survival times than low- and medium-risk patients, and a high NRI-JH risk was associated with a high mortality rate (hazard ratio [HR], 2.12; 95% confidence interval [CI], 1.08–4.77; p < 0.05). The association weakened when protein intake and C-reactive protein level were added as covariates (HR, 2.01; 95% CI, 0.95–4.28, p = 0.07).
Conclusions
High NRI-JH risk was associated with low dietary nutritional intake and poor survival in patients undergoing hemodialysis during long-term hospitalization. Nutritional status evaluation and nutritional interventions may improve prognosis in this population.


Similar content being viewed by others
References
Kalantar-Zadeh JafarTH, Nitsch D, et al. Chronic kidney disease. Lancet. 2021;398:786–802.
Kurella TM, Desai M, Kapphahn KI, et al. Dialysis versus medical management at different ages and levels of kidney function in veterans with advanced CKD. J Am Soc Nephrol. 2018;29:2169–77.
Fouque D, Kalantar-Zadeh K, Kopple J, et al. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008;73:391–8.
Ikizler TA, Cano NJ, Franch H, et al. Prevention and treatment of protein energy wasting in chronic kidney disease patients: a consensus statement by the International Society of Renal Nutrition and Metabolism. Kidney Int. 2013;84:1096–107.
Carrero JJ, Stenvinkel P, Cuppari L, et al. Etiology of the protein-energy wasting syndrome in chronic kidney disease: a consensus statement from the International Society of Renal Nutrition and Metabolism (ISRNM). J Ren Nutr. 2013;23:77–90.
Riella MC. Nutritional evaluation of patients receiving dialysis for the management of protein-energy wasting: what is old and what is new? J Ren Nutr. 2013;23:195–8.
Lawson CS, Campbell KL, Dimakopoulos I, et al. Assessing the validity and reliability of the MUST and MST nutrition screening tools in renal inpatients. J Ren Nutr. 2012;22:499–506.
Xia YA, Healy A, Kruger R. Developing and validating a renal nutrition screening tool to effectively identify undernutrition risk among renal inpatients. J Ren Nutr. 2016;26:299–307.
Jackson HS, MacLaughlin HL, Vidal-Diez A, et al. A new renal inpatient nutrition screening tool (Renal iNUT): a multicenter validation study. Clin Nutr. 2019;38:2297–303.
Golestaneh L. Decreasing hospitalizations in patients on hemodialysis: time for a paradigm shift. Semin Dial. 2018;31:278–88.
Kanda E, Kato A, Masakane I, et al. A new nutritional risk index for predicting mortality in hemodialysis patients: nationwide cohort study. PLoS ONE. 2019. https://doi.org/10.1371/journal.pone.0214524.
Shimamoto S, Yamada S, Hiyamuta H, et al. Association of the nutritional risk index for Japanese hemodialysis patients with long-term mortality: the Q-Cohort study. Clin Exp Nephrol. 2022;26:59–67.
Standard tables of food composition in Japan-2021(8th revised edition). Tokyo, Japan: Ishiyaku Publishere Inc; 2021.
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Johansson L, Fouque D, Bellizzi V, et al. As we grow old: nutritional considerations for older patients on dialysis. Nephrol Dial Transplant. 2017;32:1127–36.
Cereda E, Pedrolli C, Klersy C, et al. Nutritional status in older persons according to healthcare setting: a systematic review and meta-analysis of prevalence data using MNA((R)). Clin Nutr. 2016;35:1282–90.
Fazio S, Stocking J, Kuhn B, et al. How much do hospitalized adults move? A systematic review and meta-analysis. Appl Nurs Res. 2020. https://doi.org/10.1016/j.apnr.2019.151189.
Beddhu S, Ramkumar N, Pappas LM. Normalization of protein intake by body weight and the associations of protein intake with nutritional status and survival. J Ren Nutr. 2005;15:387–97.
Kang SS, Chang JW, Park Y. Nutritional status predicts 10-Year mortality in patients with end-stage renal disease on hemodialysis. Nutrients. 2017. https://doi.org/10.3390/nu9040399.
Kovesdy CP, Shinaberger CS, Kalantar-Zadeh K. Epidemiology of dietary nutrient intake in ESRD. Semin Dial. 2010;23:353–8.
Cederholm T, Jensen GL, Correia M, et al. GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. Clin Nutr. 2019;38:1–9.
Tinti F, Lai S, Noce A, Rotondi S, Marrone G, Mazzaferro S et al. Chronic kidney disease as a systemic inflammatory syndrome: update on mechanisms involved and potential treatment. Life (Basel, Switzerland). 2021; doi:https://doi.org/10.3390/life11050419.
de Roij van Zuijdewijn CL, ter Wee PM, Chapdelaine I, et al. A comparison of 8 nutrition-related tests to predict mortality in hemodialysis patients. J Ren Nutr. 2015; 25:412–9.
Rodrigues J, Santin F, Brito F, Lindholm B, Stenvinkel P, Avesani CM. Nutritional status of older patients on hemodialysis: which nutritional markers can best predict clinical outcomes? Nutrition. 2019;65:113–9.
Santin FG, Bigogno FG, Dias Rodrigues JC, et al. Concurrent and predictive validity of composite methods to assess nutritional status in older adults on hemodialysis. J Ren Nutr. 2016;26:18–25.
Acknowledgements
None.
Author information
Authors and Affiliations
Contributions
KK and SY: Conceptualization, data curation, formal analysis, and investigation; KK and SY: Methodology, visualization, and writing—original draft preparation; IN: Supervision and writing—review and editing.
Corresponding author
Ethics declarations
Conflicts of interest
All authors have no competing interests to declare.
Ethical approval
All procedures performed in studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee at which the studies were conducted (institutional review board approval no. 2101, June 21, 2021) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
As this was a retrospective and non-interventional study, we adopted an opt-out method instead of written informed consent. We provided patients with the opportunity to opt-out by announcing the purpose of the study and the individual data required for the study on the website of Shinkohkai Murakami Kinen Hospital, Murakami, Niigata 958–0034, Japan.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kitabayashi, K., Yamamoto, S. & Narita, I. Association of the nutritional risk index for Japanese hemodialysis with mortality and dietary nutritional intake in patients undergoing hemodialysis during long-term hospitalization. Clin Exp Nephrol 26, 1200–1207 (2022). https://doi.org/10.1007/s10157-022-02259-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-022-02259-0