Abstract
Background
There are no consensus criteria for diagnosing upper urinary tract infections (UTI). Therefore, we conducted a study to assess whether bacterial colony counts of ≥ 103 CFU/ml are optimal for diagnosing upper UTIs among infants.
Methods
This retrospective observational study included 673 patients (<4 months of age) with urine samples obtained by catheterization for bacterial cultures. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were obtained when cutoff values of 103, 104, and 105 CFU/ml were used for diagnosing upper UTIs. Upper UTI patients were divided based on cutoff values: Group A (103 CFU/ml), Group B (104 CFU/ml), and Group C (≥ 105 CFU/ml).
Results
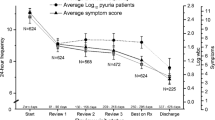
Of the 197 positive (≥ 103 CFU/ml) patients, 92 were diagnosed with an upper UTI. These patients were divided into Group A (n = 23), Group B (n = 16), and Group C (n = 53). No significant differences were detected in terms of clinical findings, including the incidence of vesicoureteral reflex. When cutoff values of 103, 104, and 105 CFU/ml were used for diagnosing upper UTIs, the sensitivity/specificity percentages were 100/81.3, 75.0/95.9, and 57.6/97.5, and the PPVs/NPVs were 46.7/100, 75.0/95.9, and 79.1/93.4.
Conclusion
Using ≥ 105 CFU/ml as a diagnostic threshold leads to approximately 40% of positive cases being missed. In contrast when ≥ 103 CFU/ml is used, all upper UTIs were identified. Therefore, bacterial colony counts of ≥ 103 CFU/ml should be considered the cutoff value for the diagnosis of upper UTIs in infants (< 4 months of age).

Similar content being viewed by others
References
Shaikh N, Morone NE, Bost JE, Farrell MH. Prevalence of urinary tract infection in childhood: a meta-analysis. Pediatr Infect Dis J. 2008;27(4):302–8. https://doi.org/10.1097/INF.0b013e31815e4122.
Bell LE, Mattoo TK. Update on childhood urinary tract infection and vesicoureteral reflux. Semin Nephrol. 2009;29(4):349–59. https://doi.org/10.1016/j.semnephrol.2009.03.011.
Stein R, Dogan HS, Hoebeke P, Kocvara R, Nijman RJ, Radmayr C, et al. Urinary tract infections in children: EAU/ESPU guidelines. Eur Urol. 2015;67(3):546–58. https://doi.org/10.1016/j.eururo.2014.11.007.
Saadeh SA, Mattoo TK. Managing urinary tract infections. Pediatr Nephrol. 2011;26(11):1967–76. https://doi.org/10.1007/s00467-011-1801-5.
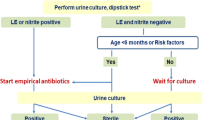
Subcommittee on Urinary Tract Infection SCoQI, Management, Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128(3):595–610. https://doi.org/10.1542/peds.2011-1330.
Smellie JM, Prescod NP, Shaw PJ, Risdon RA, Bryant TN. Childhood reflux and urinary infection: a follow-up of 10–41 years in 226 adults. Pediatr Nephrol. 1998;12(9):727–36.
Hannula A, Venhola M, Renko M, Pokka T, Huttunen NP, Uhari M. Vesicoureteral reflux in children with suspected and proven urinary tract infection. Pediatr Nephrol. 2010;25(8):1463–9. https://doi.org/10.1007/s00467-010-1542-x.
Conway PH, Cnaan A, Zaoutis T, Henry BV, Grundmeier RW, Keren R. Recurrent urinary tract infections in children: risk factors and association with prophylactic antimicrobials. JAMA. 2007;298(2):179–86. https://doi.org/10.1001/jama.298.2.179.
Hiraoka M, Hashimoto G, Tsuchida S, Tsukahara H, Ohshima Y, Mayumi M. Early treatment of urinary infection prevents renal damage on cortical scintigraphy. Pediatr Nephrol. 2003;18(2):115–8. https://doi.org/10.1007/s00467-002-1023-y.
Mori R, Lakhanpaul M, Verrier-Jones K. Diagnosis and management of urinary tract infection in children: summary of NICE guidance. BMJ. 2007;335(7616):395–7. https://doi.org/10.1136/bmj.39286.700891.AD.
Hoberman A, Wald ER, Reynolds EA, Penchansky L, Charron M. Pyuria and bacteriuria in urine specimens obtained by catheter from young children with fever. J Pediatr. 1994;124(4):513–9.
Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Mobius TE. International system of radiographic grading of vesicoureteric reflux International Reflux Study in Children. Pediatr Radiol. 1985;15(2):105–9.
Roberts KB, Downs SM, Finnell SME, Hellerstein S, Shortliffe LD, Wald ER, et al. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128(3):595–610. https://doi.org/10.1542/peds.2011-1330.
Robinson JL, Finlay JC, Lang ME, Bortolussi R, Canadian Paediatric Society ID, Immunization Committee CPC. Urinary tract infections in infants and children: Diagnosis and management. Paediatr Child Health. 2014;19(6):315–25.
Exellence NIfHaC. Urinary tract infection in children: diagnosis, treatment and long-term management. London: RCOG Press; 2007.
Garin EH, Olavarria F, Garcia Nieto V, Valenciano B, Campos A, Young L. Clinical significance of primary vesicoureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized, controlled study. Pediatrics. 2006;117(3):626–32. https://doi.org/10.1542/peds.2005-1362.
Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269–84. https://doi.org/10.1038/nrmicro3432.
Acknowledgements
We are indebted to Yoshitaka Nakamura, MD, Shin-ichiro Hori, MD, and Katsushi Kaji for collecting data. We thank Kate Fox, DPhil, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee at which the studies were conducted (Nakano Children’s Hospital License No. 36) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Akagawa, Y., Kimata, T., Akagawa, S. et al. Optimal bacterial colony counts for the diagnosis of upper urinary tract infections in infants. Clin Exp Nephrol 24, 253–258 (2020). https://doi.org/10.1007/s10157-019-01812-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-019-01812-8