Abstract
Background
Extremely low birth weight (ELBW) survivors may develop glomerulosclerosis due to low nephron number, whereas their tubular function remains unknown except for hypercalciuria and phosphaturia.
Methods
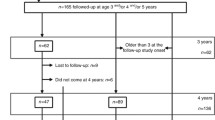
Fifty-three subjects (30 boys and 23 girls, aged 7 months-19 years, median 36 months) were studied retrospectively. The median gestational age and birth weight were 26 weeks (range 22–32) and 745 g (range 316–999), respectively. Urine calcium-to-creatinine ratio (Ca/Cr), N-acetyl-β-d-glucosaminidase-to-creatinine ratio (NAG/Cr), β2 microglobulin-to-creatinine ratio (β2m/Cr), uric acid-to-creatinine ratio (UA/Cr), glucose-to-creatinine ratio (glu/Cr), and microalbumin-to-creatinine ratio (malb/Cr) were examined. We also assessed the association between urine parameters and current age, gestational age, birth weight, and predictors of renal injury. Follow-up data were analyzed in 43 subjects 4–6 years later.
Results
Ninety percent of subjects had at least one tubular dysfunction. Frequency of elevated values was NAG/Cr 77.5%, UA/Cr 54.1%, β2m/Cr 38.2%, malb/Cr 30.4%, Ca/Cr 21.5%, and glu/Cr 20.5%. There were significant negative correlations between the current age and Ca/Cr, NAG/Cr, glu/Cr, and UA/Cr, suggesting tubular function maturation. Urine β2M/Cr and glu/Cr were negatively correlated with the gestational age. There were significant associations between elevated glu/Cr and asphyxia or neonatal acute kidney injury, and elevated NAG/Cr and indomethacin use, although these were not confirmed by multivariate analysis. At follow-up, the frequency of elevated NAG/Cr, glu/Cr, UA/Cr, and malb/Cr was reduced but that of elevated Ca/Cr, IgG/Cr, and β2m/Cr remained similar or increased.
Conclusion
Tubular dysfunction is common in ELBW survivors. Some abnormalities resolved with age while some remained persistent or even increased.
Similar content being viewed by others
Abbreviations
- ELBW:
-
Extremely low birth weight
- Ca:
-
Calcium
- Cr:
-
Creatinine
- NAG:
-
N-acetyl-β-d-glucosaminidase
- β2m:
-
β2 microglobulin
- UA:
-
Uric acid
- glu:
-
Glucose
- malb:
-
Microalbumin
- LBW:
-
Low birth weight
- IUGR:
-
Intrauterine growth restriction
- AKI:
-
Acute renal injury
- CLD:
-
Chronic lung disease
- MBD:
-
Mineral bone disorder
- SCr:
-
Serum creatinine
- eGFR:
-
Estimated glomerular filtration rate
References
Kwinta P, Klimek M, Drozdz D, et al. Assessment of long-term renal complications in extremely low birth weight children. Pediatr Nephrol. 2011;26:1095–103.
Bacchetta J, Harambat J, Dubourg L, et al. Both extrauterine and intrauterine growth restriction impair renal function in children born very preterm. Kidney Int. 2009;76:445–52.
Starzec K, Klimek M, Grudzien A, et al. Longitudinal assessment of renal size and function in extremely low birth weight children at 7 and 11 years of age. Pediatr Nephrol. 2016;31:2119–26.
Rodriguez-Soriano J, Aguirre M, Oliveros R, et al. Long-term renal follow-up of extremely low birth weight infants. Pediatr Nephrol. 2005;20:579–84.
Clark PM, Bryant TN, Hall MA, et al. Neonatal renal function assessment. Arch Dis Child. 1989;64:1264–9.
Tsukahara H, Yoshimoto M, Saito M, et al. Assessment of tubular function in neonates using urinary beta 2-microglobulin. Pediatr Nephrol. 1990;4:512–4.
Tsukahara H, Hori C, Tsuchida S, et al. Urinary N-acetyl-β-d-glucosaminidase excretion in term and preterm neonates. J Paediatr Child Health. 1994;30:536–8.
Wilkins BH. Renal function in sick very low birthweight infants: 4. Glucose excretion. Arch Dis Child. 1992;67:1162–5.
Keijzer-Veen MG, Schrevel M, Finken MJ, et al. Microalbuminuria and lower glomerular filtration rate at young adult age in subjects born very premature and after intrauterine growth retardation. J Am Soc Nephrol. 2005;16:2762–8.
Russo LM, Sandoval RM, Campos SB, et al. Impaired tubular uptake explains albuminuria in early diabetic nephropathy. J Am Soc Nephrol. 2009;20:489–94.
Comper WD, Hilliard LM, Nikolic-Paterson DJ, et al. Disease-dependent mechanisms of albuminuria. Am J Physiol Renal Physiol. 2008;295:F1589-600.
Hoppe B, Leumann E, Milliner DSM. Urolithiasis and nephrocalcinosis in childhood. In: Geary DF, Schaefer F, editors. Comprehensive pediatric nephrology. Maryland Heights: Mosby Elsevier; 2008. pp. 499–525.
Speeckaert M, SDelanghe J. Assessment of renal function. In: Turner N, Lamerie N, Goldsmith DJ, et al., editors. Oxford textbook of clinical nephrology. Oxford: Oxford University Press; 2016. pp. 61–66.
Ikeda A, Konta T, Takasaki S, et al. In a non-diabetic Japanese population, the combination of macroalbuminuria and increased urine β2-microglobulin predicts a decline of renal function: the Takahata study. Nephrol Dial Transpl. 2009;24:841–7.
Hogg RJ, Portman RJ, Milliner D, et al. Evaluation and management of proteinuria and nephrotic syndrome in children: recommendations from a pediatric nephrology panel established at the National Kidney Foundation conference on proteinuria, albuminuria, risk, assessment, detection, and elimination (PARADE). Pediatrics. 2000;105:1242–9.
Poyrazoglu HM, Dusunsel R, Yazici C, et al. Urinary uric acid: creatinine ratios in healthy Turkish children. Pediatr Int. 2009;51:526–9.
Aoshima K. Epidemiology of renal tubular dysfunction in the inhabitants of a cadmium-polluted area in the Jinzu River basin in Toyama Prefecture. Tohoku J Exp Med. 1987;152:151–72.
Nakano M, Aoshima K, Katoh T, et al. Elevation of urinary trehalase activity in patients of itai–itai disease. Arch Toxicol. 1987;60:300–3.
Uemura O, Nagai T, Ishikura K, et al. Creatinine-based equation to estimate the glomerular filtration rate in Japanese children and adolescents with chronic kidney disease. Clin Exp Nephrol. 2014;18:626–33.
Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Hibi Y, Uemura O, Nagai T, et al. The ratios of urinary β2-microglobulin and NAG to creatinine vary with age in children. Pediatr Int. 2015;57:79–84.
Nishida M, Kawakatsu H, Komatsu H, et al. Values for urinary β2-microglobulin and N-acetyl-beta-d-glucosaminidase in normal healthy infants. Acta Paediatr Jpn. 1998;40:424–6.
Muzi-Filho H, Souza AM, Bezerra CG, et al. Rats undernourished in utero have altered Ca2+ signaling and reduced fertility in adulthood. Physiol Rep. 2015;3(10):3/10/e12587.
Stiburkova B, Bleyer AJ. Changes in serum urate and urate excretion with age. Adv Chronic Kidney Dis. 2012;19:372–6.
Wilcox WD. Abnormal serum uric acid levels in children. J Pediatr. 1996;128:731–41.
Prieur B, Cordeau-Lossouarn L, Rotig A, et al. Perinatal maturation of rat kidney mitochondria. Biochem J. 1995;305:675–80.
Ashton N, Al-Wasil SH, Bond H, et al. The effect of a low-protein diet in pregnancy on offspring renal calcium handling. Am J Physiol Regul Integr Comp Physiol. 2007;293:R759–65.
Ribel-Madsen A, Ribel-Madsen R, Brons C, et al. Plasma acylcarnitine profiling indicates increased fatty acid oxidation relative to tricarboxylic acid cycle capacity in young, healthy low birth weight men. Physiol Rep. 2016;4(19):4/19/e12977.
Vasarhelyi B, Dobos M, Reusz GS, et al. Normal kidney function and elevated natriuresis in young men born with low birth weight. Pediatr Nephrol. 2000;15:96–100.
Awazu M, Arai M, Ohashi S, et al. Tubular dysfunction mimicking Dent’s disease in 2 infants born with extremely low birth weight. Case Rep Nephrol Dial. 2017;7:13–7.
Pallet N, Chauvet S, Chasse JF, et al. Urinary retinol binding protein is a marker of the extent of interstitial kidney fibrosis. PLoS One. 2014;9:e84708.
Nauta FL, Scheven L, Meijer E, et al. Glomerular and tubular damage markers in individuals with progressive albuminuria. Clin J Am Soc Nephrol. 2013;8:1106–14.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national ethical guidelines for medical and health research involving human subjects and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was not obtained but the option of opting out was provided as approved by the ethics committee at Keio University School of Medicine.
About this article
Cite this article
Matsumura, K., Matsuzaki, Y., Hida, M. et al. Tubular dysfunction in extremely low birth weight survivors. Clin Exp Nephrol 23, 395–401 (2019). https://doi.org/10.1007/s10157-018-1645-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-018-1645-4