Abstract
Background
Hyperkalemia is prevalent in end-stage renal disease patients, being involved in life-threatening arrhythmias. Although polystyrene sulfonate (PS) is commonly used for the treatment of hyperkalemia, direct comparison of effects between calcium and sodium PS (CPS and SPS) on mineral and bone metabolism has not yet been studied.
Methods
In a randomized and crossover design, 20 pre-dialysis patients with hyperkalemia (>5 mmol/l) received either oral CPS or SPS therapy for 4 weeks.
Results
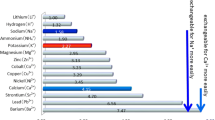
After 4-week treatments, there was no significant difference of changes in serum potassium (K) from the baseline (ΔK) between the two groups. However, SPS significantly decreased serum calcium (Ca) and magnesium (Mg) and increased intact parathyroid hormone (iPTH) values, whereas CPS reduced iPTH. ΔiPTH was inversely correlated with ΔCa and ΔMg (r = −0.53 and r = −0.50, respectively). Furthermore, sodium (Na) and atrial natriuretic peptide (ANP) levels were significantly elevated in patients with SPS, but not with CPS, whereas ΔNa and ΔANP were significantly correlated with each other in all the patients. We also found that ΔNa and Δ(Na to chloride ratio) were positively correlated with ΔHCO3 −. In artificial colon fluid, CPS increased Ca and decreased Na. Furthermore, SPS greatly reduced K, Mg, and NH3.
Conclusion
Compared with SPS, CPS may be safer for the treatment of hyperkalemia in pre-dialysis patients, because it did not induce hyperparathyroidism or volume overload.



Similar content being viewed by others
References
Einhorn LM, Zhan M, Hsu VD, Walker LD, Moen MF, Seliger SL, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169(12):1156–62.
Torlén K, Kalantar-Zadeh K, Molnar MZ, Vashistha T, Mehrotra R. Serum potassium and cause-specific mortality in a large peritoneal dialysis cohort. Clin J Am Soc Nephrol. 2012;7(8):1272–84.
Jarman PR, Kehely AM, Mather HM. Hyperkalaemia in diabetes: prevalence and associations. Postgrad Med J. 1995;71(839):551–2.
Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–9.
Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345(12):851–60.
Palmer BF. Managing hyperkalemia caused by inhibitors of the renin-angiotensin-aldosterone system. N Engl J Med. 2004;351(6):585–92.
Takaichi K, Takemoto F, Ubara Y, Mori Y. Analysis of factors causing hyperkalemia. Intern Med. 2007;46(12):823–9.
Sterns RH, Grieff M, Bernstein PL. Treatment of hyperkalemia: something old, something new. Kidney Int. 2016;89(3):546–54.
Watson M, Abbott KC, Yuan CM. Damned if you do, damned if you don’t: potassium binding resins in hyperkalemia. Clin J Am Soc Nephrol. 2010;5(10):1723–6.
Tomino Y, Yamazaki T, Shou I, Tsuge T, Satake K, Takeda Y, et al. Dose-response to a jelly preparation of calcium polystyrene sulfonate in patients with hyperkalemia–changes in serum potassium levels with or without a RAAS inhibitor. Clin Nephrol. 2007;68(6):379–85.
Lepage L, Dufour AC, Doiron J, Handfield K, Desforges K, Bell R, et al. Randomized clinical trial of sodium polystyrene sulfonate for the treatment of mild hyperkalemia in CKD. Clin J Am Soc Nephrol. 2015;10(12):2136–42.
Berlyne GM, Janabi K, Shaw AB. Dangers of resonium A in the treatment of hyperkalemia in renal failure. Lancet. 1966;1(7430):167–9.
Frohnert PP, Johnson WJ, Mueller GJ, Tauxe WN, McCall JT. Resin treatment of hyperkalemia. II. Clinical experience with a cation exchange resin (calcium cycle). J Lab Clin Med. 1968;71(5):840–6.
Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004;15(8):2208–18.
Block GA, Zaun D, Smits G, Persky M, Brillhart S, Nieman K, et al. Cinacalcet hydrochloride treatment significantly improves all-cause and cardiovascular survival in a large cohort of hemodialysis patients. Kidney Int. 2010;78(6):578–89.
Komaba H, Kakuta T, Fukagawa M. Diseases of the parathyroid gland in chronic kidney disease. Clin Exp Nephrol. 2011;15(6):797–809.
Jadoul M, Albert JM, Akiba T, Akizawa T, Arab L, Bragg-Gresham JL, et al. Incidence and risk factors for hip or other bone fractures among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2006;70(7):1358–66.
Taniguchi M, Fukagawa M, Fujii N, Hamano T, Shoji T, Yokoyama K, et al. Serum phosphate and calcium should be primarily and consistently controlled in prevalent hemodialysis patients. Ther Apher Dial. 2013;17(2):221–8.
Fukagawa M, Kido R, Komaba H, Onishi Y, Yamaguchi T, Hasegawa T, et al. Abnormal mineral metabolism and mortality in hemodialysis patients with secondary hyperparathyroidism: evidence from marginal structural models used to adjust for time-dependent confounding. Am J Kidney Dis. 2014;63(6):979–87.
George J, Majeed W, Mackenzie IS, Macdonald TM, Wei L. Association between cardiovascular events and sodium-containing effervescent, dispersible, and soluble drugs: nested case-control study. BMJ. 2013;347:f6954.
Takase H, Sugiura T, Kimura G, Ohte N, Dohi Y. Dietary sodium consumption predicts future blood pressure and incident hypertension in the Japanese normotensive general population. J Am Heart Assoc. 2015;4(8):e001959.
Manabe R, Fukami K, Ando R, Sakai K, Kusumoto T, Hazama T, et al. Effects of switching from calcium carbonate to lanthanum carbonate on bone mineral metabolism in hemodialysis patients. Ther Apher Dial. 2013;17(Suppl 1):35–40.
Clase CM, Norman GL, Beecroft ML, Churchill DN. Albumin-corrected calcium and ionized calcium in stable haemodialysis patients. Nephrol Dial Transplant. 2000;15(11):1841–6.
Hynes D, Bates S, Loughman A, Klim S, French C, Kelly AM. Arteriovenous blood gas agreement in intensive care patients with varying levels of circulatory compromise: a pilot study. Crit Care Resusc. 2015;17(4):253–6.
Yamada T, Alpers D, Laine L, Owyang C, Powell D. Approach to the patient with diarrhea. Textb Gastroenterol. 2003;1:858–64.
Evans BM, Jones NC, Milne MD, Yellowlees H. Ion-exchange resins in the treatment of anuria. Lancet. 1953;265(6790):791–5.
Li M, Jiang J, Yue L. Functional characterization of homo- and heteromeric channel kinases TRPM6 and TRPM7. J Gen Physiol. 2006;127(5):525–37.
Kumar R, Thompson JR. The regulation of parathyroid hormone secretion and synthesis. J Am Soc Nephrol. 2011;22(2):216–24.
Brown EM, Gamba G, Riccardi D, Lombardi M, Butters R, Kifor O, et al. Cloning and characterization of an extracellular Ca(2+)-sensing receptor from bovine parathyroid. Nature. 1993;366(6455):575–80.
Brown EM, MacLeod RJ. Extracellular calcium sensing and extracellular calcium signaling. Physiol Rev. 2001;81(1):239–97.
Shoback DM, Thatcher JG, Brown EM. Interaction of extracellular calcium and magnesium in the regulation of cytosolic calcium and PTH release in dispersed bovine parathyroid cells. Mol Cell Endocrinol. 1984;38(2–3):179–86.
Sakaguchi Y, Shoji T, Hayashi T, Suzuki A, Shimizu M, Mitsumoto K, et al. Hypomagnesemia in type 2 diabetic nephropathy: a novel predictor of end-stage renal disease. Diabetes Care. 2012;35(7):1591–7.
Sakaguchi Y, Fujii N, Shoji T, Hayashi T, Rakugi H, Isaka Y. Hypomagnesemia is a significant predictor of cardiovascular and non-cardiovascular mortality in patients undergoing hemodialysis. Kidney Int. 2014;85(1):174–81.
Bolland MJ, Avenell A, Baron JA, Grey A, MacLennan GS, Gamble GD, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341:c3691.
Jadoul M, Karaboyas A, Goodkin DA, Tentori F, Li Y, Labriola L, et al. Potassium-binding resins: associations with serum chemistries and interdialytic weight gain in hemodialysis patients. Am J Nephrol. 2014;39(3):252–9.
Powell DW, Berschneider HM, Lawson LD, Martens H. Regulation of water and ion movement in intestine. Ciba Found Symp. 1985;112:14–33.
Kamel KS, Schreiber M. Asking the question again: are cation exchange resins effective for the treatment of hyperkalemia? Nephrol Dial Transplant. 2012;27(12):4294–7.
van de Strihou CY, Dieu JP. Potassium deficiency acidosis in the dog: effect of sodium and potassium balance on renal response to a chronic acid load. Kidney Int. 1977;11(5):335–47.
Lindner G, Schwarz C, Grüssing H, Kneidinger N, Fazekas A, Funk GC. Rising serum sodium levels are associated with a concurrent development of metabolic alkalosis in critically ill patients. Intensive Care Med. 2013;39(3):399–405.
Luke RG, Galla JH. It is chloride depletion alkalosis, not contraction alkalosis. J Am Soc Nephrol. 2012;23(2):204–7.
Seifter JL. Integration of acid-base and electrolyte disorders. N Engl J Med. 2014;371(19):1821–31.
Acknowledgement
This work was supported, in part, by Grants-in-Aid for Welfare and Scientific Research (C) (no. 16k09637) (K.F) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Fukami has received honoraria such as lecture fees from Sanwa (Sanwa Kagaku Kenkyusyo). This paper has not been published previously in whole or part.
Human rights
(with IRB approval number) All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional ethics committee at which the studies were conducted (Approval No. 13170) and with the 1964 Helsinki Declaration and its later amendments of comparable ethical standards. This trial was registered with the University Hospital Medical Information Network clinical trials database (UMIN 000021955).
Informed consent
Informed consent was obtained from all individual participants included in the study.
About this article
Cite this article
Nakayama, Y., Ueda, K., Yamagishi, Si. et al. Compared effects of calcium and sodium polystyrene sulfonate on mineral and bone metabolism and volume overload in pre-dialysis patients with hyperkalemia. Clin Exp Nephrol 22, 35–44 (2018). https://doi.org/10.1007/s10157-017-1412-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-017-1412-y