Abstract
Background
Crush syndrome is a common injury, the main characteristics of which include acute kidney injury. However, there is still lack of reliable animal model of crush syndrome, and it also remains controversial as to which type of fluid should be chosen as a more appropriate treatment option for prevention and treatment of acute kidney injury.
Methods
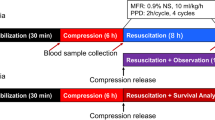
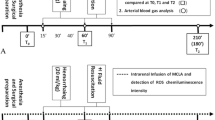
The rabbits were crushed at the lower limbs for 6 h with 36 times the body weight, which means the pressure of each leg was also 36 times the body weight. Fluid resuscitation was performed from 1 h prior to the end of the crush treatment until 24 h after the reperfusion. Tissue, blood and urine samples were collected at predetermined time points before and after reperfusion. Twelve rabbits in each group were taken for survival observation for 72 h.
Results
The model group showed elevated serum creatine kinase, aspartate aminotransferase, alanine aminotransferase, and K+ level, reduced serum Ca2+ level and Na+ level, and increased serum creatinine and blood urea nitrogen levels, neutrophil gelatinase-associated lipocalin, and kidney injury molecule-1 (p < 0.05). The 0.9 % normal saline (SAL) group and SAL plus 6 % hydroxyethyl starch 130/0.4 SAL/HES group showed reduced serum creatinine and blood urea nitrogen levels (p < 0.05). The SAL/HES group also showed reduced serum IL-6 and IL-10 levels (p < 0.05). The 72 h survival rate of the SAL/HES group was higher than that of the model group (p < 0.05).
Conclusion
The rabbit model of crush syndrome showed clinical features consistent with those of crush syndrome. There was no significant difference in the ability of preventing AKI after a crush injury between the two fluid solutions, while SAL/HES can improve the survival rate.




Similar content being viewed by others
References
He Q, Wang F, Li G, et al. Crush syndrome and acute kidney injury in the Wenchuan Earthquake. J Trauma. 2011;70:1213–8.
Better OS, Abassi ZA. Early fluid resuscitation in patients with rhabdomyolysis. Nat Rev Nephrol. 2011;7:416–22.
Murata I, Ooi K, Sasaki H, et al. Characterization of systemic and histologic injury after crush syndrome and intervals of reperfusion in a small animal model. J Trauma. 2011;70:1453–63.
James MF. Place of the colloids in fluid resuscitation of the traumatized patient. Curr Opin Anaesthesiol. 2012;25:248–52.
Ogilvie MP, Pereira BM, McKenney MG, et al. First report on safety and efficacy of hetastarch solution for initial fluid resuscitation at a level 1 trauma center. J Am Coll Surg. 2010;210:870–82.
James MF, Michell WL, Joubert IA, et al. Resuscitation with hydroxyethyl starch improves renal function and lactate clearance in penetrating trauma in a randomized controlled study: the FIRST trial (fluids in resuscitation of severe trauma). Br J Anaesth. 2011;107:693–702.
Urbano J, López-Herce J, Solana MJ, et al. Comparison of normal saline, hypertonic saline and hypertonic saline colloid resuscitation fluids in an infant animal model of hypovolemic shock. Resuscitation. 2012;83:1159–65.
Aksu U, Bezemer R, Yavuz B, et al. Balanced vs unbalanced crystalloid resuscitation in a near-fatal model of hemorrhagic shock and the effects on renal oxygenation, oxidative stress, and inflammation. Resuscitation. 2011;83:767–73.
Ozgüç H, Kahveci N, Akköse S, et al. Effects of different resuscitation fluids on tissue blood flow and oxidant injury in experimental rhabdomyolysis. Crit Care Med. 2005;33:2579–86.
Finfer S, Liu B, Taylor C, et al. Resuscitation fluid use in critically ill adults: an international cross-sectional study in 391 intensive care units. Crit Care. 2010;14:185.
Inan N, Iltar S, Surer H, et al. Effect of hydroxyethyl starch 130/0.4 on ischaemia/reperfusion in rabbit skeletal muscle. Eur J Anaesthesiol. 2009;26:160–5.
Walker AM, Lee K, Dobson GM, et al. The viscous behaviour of HES 130/0.4 (Voluven(R)) and HES 260/0.45 (Pentaspan(R)). Can J Anaesth. 2012;59:288–94.
Westphal M, James MF, Kozek-Langenecker S, et al. Hydroxyethyl starches: different products–different effects. Anesthesiology. 2009;111:187–202.
Dubin A, Dubin A, Pozo MO, et al. Comparison of 6% hydroxyethyl starch 130/0.4 and saline solution for resuscitation of the microcirculation during the early goal-directed therapy of septic patients. J Crit Care. 2010;25(659):e1–8.
Akimau P, Yoshiya K, Hosotsubo H, Takakuwa T, Tanaka H, et al. New experimental model of crush injury of the hindlimbs in rats. J Trauma. 2005;58:51–8.
Schick MA, Isbary TJ, Schlegel N, et al. The impact of crystalloid and colloid infusion on the kidney in rodent sepsis. Intensive Care Med. 2010;36:541–8.
Wang Y, Zhang L, Cai GY, et al. Fasudil ameliorates rhabdomyolysis-induced acute kidney injury via inhibition of apoptosis. Ren Fail. 2011;33:811–8.
Sun L, Xu S, Zhou M, et al. Effects of cysteamine on MPTP-induced dopaminergic neurodegeneration in mice. Brain Res. 2010;1335:74–82.
Bywaters EGL, Popjak G. Experimental crushing injury. Peripheral circulatory collapse and other effects of muscle necrosis in the rabbit. Surg Gyn Obst. 1942;75:612–27.
El-Abdellati E, Eyselbergs M, Sirimsi H, et al. An observational study on rhabdomyolysis in the intensive care unit. Exploring its risk factors and main complication: acute kidney injury. Ann Intensive Care. 2013;3:8.
Sever MS, Vanholder R, Lameire N. Management of crush-related injuries after disasters. N Engl J Med. 2006;354:1052–63.
Antonopoulos CN, Kalkanis A, Georgakopoulos G, et al. Neutrophil gelatinase-associated lipocalin in dehydrated patients: a preliminary report. BMC Res Notes. 2011;4:435.
Ferreira EL, Terzi RG, Silva WA, et al. Early colloid replacement therapy in a near-fatal model of hemorrhagic shock. Anesth Analg. 2005;101:1785–91.
Rubinstein I, Abassi Z, Coleman R, et al. Involvement of nitric oxide system in experimental muscle crush injury. J Clin Invest. 1998;101:1325–33.
Sonoi H, Matsumoto N, Ogura H, et al. The effect of antithrombin on pulmonary endothelial damage induced by crush injury. Shock. 2009;32:593–600.
Kaszaki J, Wolfárd A, Szalay L, et al. Pathophysiology of ischemia-reperfusion injury. Transplant Proc. 2006;38:826–8.
Arand M, Melzner H, Kinzl L, et al. Early inflammatory mediator response following isolated traumatic brain injury and other major trauma in humans. Langenbeck’s Arch Surg. 2001;386:241–8.
Chang CH, Hsiao CF, Yeh YM. Circulating interleukin-6 level is a prognostic marker for survival in advanced nonsmall cell lung cancer patients treated with chemotherapy. Int J Cancer. 2013;132(9):1977–85.
Shimazaki J, Matsumoto N, Ogura H, et al. Systemic involvement of high-mobility group box 1 protein and therapeutic effect of anti-high-mobility group box 1 protein antibody in a rat model of crush injury. Shock. 2012;37:634–8.
Sotnikova R, Nedelčevová J, Navarová J, et al. Protection of the vascular endothelium in experimental situations. Interdiscip Toxicol. 2011;4:20–6.
Acknowledgments
This work was partially supported by a research grant from Chinese PLA 12th Five-Year Plan for Medical Sciences (BWS11J027), a grant from National Natural Science Foundation of China (81170643), and a grant from National Key Technology R&D Program (2011BAI10B00).
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
About this article
Cite this article
Kong, Dy., Hao, Lr., Zhang, L. et al. Comparison of two fluid solutions for resuscitation in a rabbit model of crush syndrome. Clin Exp Nephrol 19, 1015–1023 (2015). https://doi.org/10.1007/s10157-015-1114-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-015-1114-2