Abstract
Background
A recent meta-analysis showed that obesity increased the conversion rate and postoperative morbidity of rectal cancer surgery, but did not influence pathological results. However, this meta-analysis included patients with cancer of the upper rectum and had many biases. The aim of the present retrospective study was to investigate the impact of obesity, defined as a body mass index (BMI) ≥ 30 kg/m2, on postoperative morbidity and short- and long-term oncologic outcomes of total mesorectal excision for mid and low rectal cancer in consecutive patients.
Methods
This study included all eligible patients who were operated on for mid and lower rectal cancer between 1999 and 2018 in our hospital. We compared 90-day postoperative morbidity and mortality, and short- and long-term oncologic outcomes between obese and non-obese patients.
Results
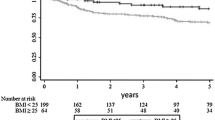
Three hundred and ninety patients [280 males, mean age 65.7 ± 11.3 years, 59 obese individuals (15.1%)] were included. There was no difference in the 90-day mortality rate between obese and non-obese groups (p = 0.068). There was a difference in the overall 90-day morbidity rate between the obese and non-obese groups that disappeared after propensity score matching of the patients. There was no difference in short-term oncological parameters, with a median follow-up of 43 (20–84) months, and there were no significant differences in disease-free and overall survival between obese and non-obese patients (p = 0.42 and p = 0.11, respectively).
Conclusions
Obesity does not affect the 90-day morbidity rate, or short- and long-term oncologic results in patients operated on for mid and lower rectal cancer.



Similar content being viewed by others
References
Swinburn BA, Kraak VI, Allender S et al (2019) The global syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. Lancet 393:791–846
Czernichow S, Renuy A, Rives-Lange C et al (2021) Evolution of the prevalence of obesity in the adult population in France, 2013–2016: the Constances study. Sci Rep 11:14152
Mcmillan DC, Sattar N, Lean M, McArdle CS (2006) Obesity and cancer. BMJ 333:1109–1111
Gendall KA, Raniga S, Kennedy R, Frizelle FA (2007) The impact of obesity on outcome after major colorectal surgery. Dis Colon Rectum 50:2223–2237
Hotouras A, Ribas Y, Zakeri SA et al (2016) The influence of obesity and body-mass index on the outcome of laparoscopic colorectal surgery: a systematic literature review. Colorectal Dis 2016:O337–O366
Hrabe JE, Sherman SK, Charlton ME, Cromwell JW, Byrn JC (2014) Effect of BMI on outcomes in proctectomy. Dis Colon Rectum 57:608–615
Miskovic D, Foster J, Agha A et al (2015) Standardization of laparoscopic total mesorectal excision for rectal cancer: a structured international expert consensus. Ann Surg 261:716–722
Poon JT, Law WL (2009) Laparoscopic resection for rectal cancer: a review. Ann Surg Oncol 16:3038–3047
Rottoli M, Bona S, Rosati R et al (2009) Laparoscopic rectal resection for cancer: effects of conversion on short-term outcome and survival. Ann Surg Oncol 16:1279–1286
Tepper JE, O’Conell MJ, Niedzwiecki D et al (2001) Impact of number of nodes retrieved on outcome in patients with rectal cancer. J Clin Oncol 19:157–163
Görög D, Nagy P, Péter A, Perner F (2003) Influence of obesity on lymph node recovery from rectal resection specimens. Pathol Oncol Res 2003:180–183
Kang J, Baek SE, Kim T et al (2012) Impact of fat obesity on laparoscopic total mesorectal excision: more reliable indicator than Body Mass Index. Int J Colorectal Dis 27:497–505
Qiu Y, Liu Q, Chen G et al (2016) Outcome of rectal cancer surgery in obese and nonobese patients: a meta-analysis. World J Surg Oncol 14:23–30
You JF, Tang R, Changchien CR et al (2009) Effect of Body Mass Index on the outcome of patients with rectal cancer receiving curative anterior resection: disparity between the upper and lower rectum. Ann Surg 249:783–787
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
http://www.who.int/mediacentre/factsheets/fs311/en/index.htm. Accessed 16 Feb 2021
https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000025441587. Accessed 16 Feb 2021
Girard E, Trilling B, Rabattu PY, Sage PY, Chaffanjon P, Faucheron JL (2019) Level of inferior mesenteric artery ligation in low rectal cancer surgery: high tie preferred over low tie. Tech Coloproctol 23:267–271
Jarry J, Faucheron JL, Moreno W, Bellera CA, Evrard S (2011) Delayed colo-anal anastomosis is an alternative to prophylactic diverting stoma after total mesorectal excision for middle and low rectal carcinomas. Eur J Surg Oncol 37:127–133
Denost Q, Rouanet P, Faucheron JL et al (2017) To drain or not to drain infraperitoneal anastomosis after rectal excision for cancer. The GRECCAR 5 randomized trial. Ann Surg 265:474–480
Bege T, Lelong B, Francon D, Turrini O, Guiramand J, Delpero JR (2009) Impact of obesity on short-term results of laparoscopic rectal cancer resection. Surg Endosc 23:1460–1464
Denost Q, Quintane L, Buscail E, Martenot M, Laurent C, Rullier E (2013) Short- and long-term impact of Body Mass Index on laparoscopic rectal cancer surgery. Colorectal Dis 15:463–469
Meyerhardt JA, Tepper JE, Niedzwiecki D et al (2004) Impact of Body Mass Index on outcomes and treatment-related toxicity in patients with stage II and III rectal cancer: findings from intergroup Trial 0114. J Clin Oncol 22:648–657
Ishii Y, Hasegawa H, Nishibori H et al (2005) Impact of visceral obesity on surgical outcome after laparoscopic surgery for rectal cancer. Br J Surg 92:1261–1262
Ballian N, Yamane B, Leverson G et al (2010) Body Mass Index does not affect postoperative morbidity and oncologic outcomes of total mesorectal excision for rectal adenocarcinoma. Ann Surg Oncol 17:1606–1613
Chern H, Chou J, Donkor C et al (2010) Effects of obesity in rectal cancer surgery. J Am Coll Surg 211:55–60
Balentine CJ, Wilks J, Robinson C et al (2010) Obesity increases wound infections in rectal cancer surgery. J Surg Res 163:35–39
Karahasanoglu T, Hamzaoglu I, Baca B, Aytac E, Kirbiyik E (2011) Impact of increased Body Mass Index on laparoscopic surgery for rectal cancer. Eur Surg Res 46:87–93
Ballian N, Lubner MG, Munoz A et al (2012) Visceral obesity is associated with outcomes of total mesorectal excision for rectal adenocarcinoma. J Surg Oncol 105:365–370
Oyasiji T, Baldwin K, Katz SC, Espat NJ, Somasundar P (2012) Feasibility of purely laparoscopic resection of locally advanced rectal cancer in obese patients. World J Surg Oncol 10:147–151
Aytac E, Lavery IC, Kalady MF, Kiran RP (2013) Impact of obesity on operation performed, complications, and long-term outcomes in terms of restoration of intestinal continuity for patients with mid and low rectal cancer. Dis Colon Rectum 56:689–697
Clark W, Siegel EM, Chen YA et al (2013) Quantitative measures of visceral adiposity and Body Mass Index in predicting rectal cancer outcomes after néoadjuvant chemoradiation. J Am Coll Surg 216:1070–1081
Bokey L, Chapuis PH, Dent OF (2014) Impact of obesity on complications after resection for rectal cancer. Colorectal Dis 16:896–906
Sun Y, Xu Z, Lin H et al (2017) Impact of Body Mass Index on treatment outcome of neoadjuvant chemoradiotherapy in locally advanced rectal cancer. Eur J Surg Oncol 43:1828–1834
Lee KH, Kang B, Ahn BK (2018) Higher visceral fat area/subcutaneous fat area ratio measured by computed tomography is associated with recurrence and poor survival in patients with mid and low rectal cancers. Int J Colorectal Dis 33:1303–1307
Paun BC, Cassie S, MacLean AR, Dixon E, Buie WD (2010) Postoperative complications following surgery for rectal cancer. Ann Surg 251:807–818
Stornes T, Wibe A, Endreseth BH (2016) Complications and risk prediction in treatment of elderly patients with rectal cancer. Int J Colorectal Dis 31:87–93
Makino T, Shukla PJ, RubinoF MJW (2012) The impact of obesity on perioperative outcomes after laparoscopic colorectal resection. Ann Surg 255:228–236
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval and Informed consent
The requirements for anonymization of personal data by the Data Protection Act 1998 were satisfied. According to the French Health Authority (HAS), this study was classified as category 3 (as defined by the French legislation “Jardé Law”); therefore, there was no need for the patient’s consent as it was considered an audit [17]. Study ethics approval was obtained on 19 May 2020 (CECIC Rhône-Alpes-Auvergne, Clermont-Ferrand, IRB 5891).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Fig. S1
: Propensity score-matching: absolute mean differences. (DOCX 92 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gutierrez, L., Bonne, A., Trilling, B. et al. Impact of obesity on morbidity and oncologic outcomes after total mesorectal excision for mid and low rectal cancer. Tech Coloproctol 27, 407–418 (2023). https://doi.org/10.1007/s10151-022-02725-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-022-02725-7