Abstract
Background
The efficacy of adjuvant chemotherapy for high-risk stage II colon cancer (CC) has not been well established. Using propensity score matching, we previously reported that the 3-year disease-free survival (DFS) rate was significantly higher in patients treated with uracil and tegafur plus leucovorin (UFT/LV) against surgery alone. We report the final results, including updated 5-year overall survival (OS) rates and risk factor analysis outcomes.
Methods
In total, 1902 high-risk stage II CC patients with T4, perforation/penetration, poorly differentiated adenocarcinoma/mucinous carcinoma, and/or < 12 dissected lymph nodes were enrolled in this prospective, non-randomized controlled study based on their self-selected treatment. Oral UFT/LV therapy was administered for six months after surgery.
Results
Of the 1880 eligible patients, 402 in Group A (surgery alone) and 804 in Group B (UFT/LV) were propensity score-matched. The 5-year DFS rate was significantly higher in Group B than in Group A (P = 0.0008). The 5-year OS rates were not significantly different between groups. The inverse probability of treatment weighting revealed significantly higher 5-year DFS (P = 0.0006) and 5-year OS (P = 0.0122) rates in group B than in group A. Multivariate analyses revealed that male sex, age ≥ 70 years, T4, < 12 dissected lymph nodes, and no adjuvant chemotherapy were significant risk factors for DFS and/or OS.
Conclusion
The follow-up data from our prospective non-randomized controlled study revealed a considerable survival advantage in DFS offered by adjuvant chemotherapy with UFT/LV administered for six months over surgery alone in individuals with high-risk stage II CC.
Trial registration
Japan Registry of Clinical Trials: jRCTs031180155 (date of registration: 25/02/2019), UMIN Clinical Trials Registry: UMIN000007783 (date of registration: 18/04/2012).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most common malignancy and second most frequent cause of cancer-related mortality worldwide [1]. According to the American Society of Clinical Oncology, the National Comprehensive Cancer Network, and the European Society for Medical Oncology, it is recommended that patients with stage II colon cancer (CC) and a high risk of recurrence receive adjuvant chemotherapy [2,3,4,5]. According to the Japanese Society for Cancer of the Colon and Rectum’s clinical practice guidelines, adjuvant chemotherapy is recommended for stage II colorectal cancer patients who have a high likelihood of recurrence [6]. Nevertheless, while the advantages of adjuvant chemotherapy for stage III CC are well-established, its benefits for stage II CC remain uncertain due to the absence of conclusive data from randomized controlled studies [7, 8]. Additionally, the risk factors for recurrence in stage II CC remain to be fully established [9,10,11]. Subset analyses of the MOSAIC study revealed no statistically significant improvement in the efficacy of adjuvant therapy with the addition of oxaliplatin to 5-fluorouracil (FL) for stage II CC, regardless of the presence or absence of risk factors for recurrence [12].
Oral uracil and tegafur plus leucovorin (UFT/LV) have demonstrated effectiveness and safety comparable to those of intravenous 5-fluorouracil/LV in individuals with stage II/III cancer in Japan [13, 14]. A definitive advantage of oral UFT/LV as adjuvant chemotherapy over intravenous 5-fluorouracil/LV is increased convenience [14]. We conducted a multicenter prospective trial with two arms, one of which was non-randomized. Patients diagnosed with stage II CC were given the option to either undergo surgery alone or surgery followed by oral UFT/LV. Propensity score (PS) matching [15, 16] was employed to mitigate confounding biases in comparing between the groups. Due to an insufficient number of patients enrolled in the randomized arm, it was excluded from the analyses. In this prospective study utilizing PS matching, a 6-month course of oral UFT/LV therapy demonstrated an enhancement in the 3-year disease-free survival (DFS) rate in comparison to surgery alone (UFT/LV = 80.9%, surgery alone = 74.0%; hazard ratio = 0.64; 95% CI 0.50 to 0.83; P = 0.0006). Furthermore, it exhibited an acceptable safety profile among patients who underwent curative-intent resection for stage II CC [17]. Additionally, multivariate analyses indicated that oral UFT/LV postoperative therapy for 6 months was a significant independent prognostic factor for DFS [18]. Nevertheless, the overall survival (OS) data provided in the previous study were preliminary. Herein, we present the final results of the study, including the updated 5-year DFS and OS rates, and report the outcomes of risk factor analyses for DFS and OS.
Patients and methods
The specifics of the study protocol are available in our previous report [19].
Patients
Eligible patients, aged 20–80 years, with histologically confirmed stage II colon adenocarcinoma, met at least one of the following criteria: T4 disease, perforation/penetration, poorly differentiated adenocarcinoma/mucinous carcinoma, or < 12 dissected lymph nodes. Additionally, they had undergone R0 resection, possessed an Eastern Cooperative Oncology Group performance status of 0/1, and were able to commence the study treatment with oral UFT/LV within eight weeks post-surgery.
Ethics approval and consent to participate
Prior to enrollment, written informed consent was obtained from all patients. The multi-institutional study, designated as JFMC46-1201, received approval from the Certified Review Board (CRB3180009) of the National Cancer Center Hospital East and was conducted in compliance with the Declaration of Helsinki.
Allocation to treatment
This prospective, non-randomized controlled study was based on patients’ self-selected treatments: surgery alone (Group A) or surgery followed by UFT/LV (Group B). Patients in Group A underwent blood tests every 3 months and chest and abdominal computed tomography examinations every 6 months for up to 5 years or until confirmation of recurrence, occurrence of other malignancies, or death. Colonoscopy was also performed 1 and 3 years after surgery. Further details regarding the UFT/LV treatment can be found in our previous report [17]. Following the completion of the 6-month UFT/LV therapy, patients were monitored according to the same schedule used in Group A, with the exception that adverse events (AEs) were monitored from the start of the UFT/LV therapy until 28 days after the final dose.
Endpoints
The primary endpoint of the study was to evaluate DFS, which was the period between the registration date and the first occurrence of secondary cancer, recurrence, or death form any cause. The secondary endpoints were OS, which was the duration from the registration date to death from any cause, as well as the frequency of AEs based on their severity. The prognostic indicators for DFS and OS were determined through a multivariate analysis.
Statistical analysis
The target sample size was projected to be 1,715 patients, with a 1:2 ratio between Groups A and B [19]. To assess survival benefits, 1:2 PS matching was employed to mitigate confounding biases when comparing Groups A and B [15, 16]. Prespecified potential confounding factors for PS estimation included sex, age (≥ 70 or < 70 years), T4 disease, bowel perforation, poorly differentiated adenocarcinoma, mucinous carcinoma, number of dissected lymph nodes (≥ 12 or < 12), and number of participating patients at each institution (≥ 5 or < 5). Further details regarding the PS matching method can be found in our previous reports [17, 19]. The Kaplan–Meier method was utilized to estimate the 5-year DFS and OS rates in each group, with 95% confidence intervals calculated using Greenwood’s formula.
Analyses were additionally conducted utilizing inverse probability of treatment weighting (IPTW) based on the estimated PSs [20]. For IPTW analysis, standard errors were calculated using a robust sandwich variance estimator [21]. Multivariate analyses of prognostic factors, including age, sex, tumor location, depth of tumor invasion, perforation/penetration, poorly differentiated component, mucinous component, number of examined lymph nodes, number of participating patients at each institution, tumor location, and postoperative adjuvant chemotherapy, were executed using Cox proportional hazard regression via the backward elimination approach, with a significance level of P = 0.05 for exclusion. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
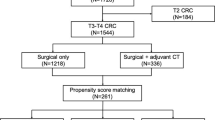
Patient characteristics before and after PS matching
A total of 1902 patients from 321 Japanese institutions were enrolled in this study between May 2012 and April 2016. Of these, 1880 patients were deemed eligible for the non-randomized study, comprising 641 patients in Group A and 1239 patients in Group B. Following 1:2 propensity score matching, 402 patients in Group A and 804 patients in Group B were successfully matched, with no significant differences observed in the eight confounding factors between the groups, as detailed in a prior report [17]. The standardized difference for all confounding factors was < 0.08.
Survival outcomes in the PS-matched population
As of the data cut-off date on January 13, 2022, the median follow-up time for DFS in Groups A and B was 60.5 months (interquartile range [IQR], 59.9–63.1 months) in the PS-matched population. The 5-year DFS rate was significantly higher in Group B (76.3% [73.1–79.1%]) than in Group A (68.8% [63.9–73.2%]) (HR = 0.66 [0.51–0.84]; P = 0.0008) (Fig. 1a). The median follow-up time for OS in Groups A and B was 61.3 months (IQR, 60.3–65.3 months) in the PS-matched population. No significant difference was observed in the 5-year OS rate between Group A (89.0% [85.3–91.8%]) and Group B (91.2% [89.0–93.0%]) (HR = 0.74 [0.50–1.10]; P = 0.1391) (Fig. 1b).
Disease-free and overall survival in patients with resected high-risk stage II colon cancer. a Disease-free and b overall survival in the propensity score-matched groups. c Disease-free and d overall survival in the inverse probability of treatment weighting groups. Group A (blue): surgery alone; Group B (green): surgery followed by UFT/LV treatment. CI confidence interval, DFS disease-free survival, HR hazard ratio, OS overall survival, UFT/LV uracil, and tegafur plus leucovorin. P values were obtained using the log-rank test
Events in the PS-matched population
There were 121 (30.1%) and 190 (23.6%) DFS events in Groups A and B, respectively. Recurrence of primary CC occurred in 75 patients (18.7%) in Group A commonly in the lung and liver, and in 127 patients (15.8%) in Group B, most commonly in the peritoneum and liver. The median time to recurrence was significantly longer in Group B (17.3 months; range, 1.8–59.8 months) than in Group A (8.7 months; range, 2.0–52.6 months) (P < 0.0001). Moreover, 45 (11.2%) and 72 (9.0%) OS events (all deaths) occurred in Groups A and B, respectively (Table 1).
Survival outcomes in the IPTW population
The patients’ background characteristics were well balanced between Group A (n = 641) and Group B (n = 1239), as shown in a previous report [17]. The median follow-up time for DFS was 60.5 months (IQR, 60.0–63.0 months) and the 5-year DFS rate (95% CI) was significantly higher in Group B (75.6% [73.0–78.0%]) than in Group A (68.1% [64.0–71.9%]) (HR = 0.71 [0.59–0.86]; P = 0.0006) (Fig. 1c). The median follow-up time for OS was 61.3 months (IQR, 60.3–65.2 months), and the 5-year OS rate was significantly higher in Group B (92.1% [90.4–93.5%]) than in Group A (88.3% [85.3–90.8%]) (HR = 0.66 [0.49–0.90]; P = 0.0122) (Fig. 1d).
Subgroup analyses were conducted to ascertain prognostic factors for DFS and OS within the IPTW population. Regarding both DFS (Fig. 2) and OS (Fig. 3), the estimation of hazard ratios and 95% CIs showed that the potential benefit from UFT/LV chemotherapy could not be ruled out across most subgroups delineated by baseline prognostic factors. Additionally, a significant benefit from UFT/LV was established in several subgroups.
Hazard ratios and 95% CIs for DFS events in patients treated with surgery followed by UFT/LV treatment compared with those in patients treated with surgery alone according to baseline prognostic factors (inverse probability of treatment-weighting groups). Analyses were conducted using a Cox regression model. CI confidence interval, DFS disease-free survival, UFT/LV uracil and tegafur plus leucovorin
Hazard ratios and 95% CIs for death in patients treated with surgery followed by UFT/LV treatment compared with those in patients treated with surgery alone according to baseline prognostic factors (inverse probability of treatment weighting groups). Analyses were conducted using a Cox regression model. CI confidence interval, OS overall survival, UFT/LV uracil and tegafur plus leucovorin
In the multivariate analysis, the Cox proportional hazards model identified the following statistically significant prognostic factors for DFS and OS: age, sex, T factor, number of dissected lymph nodes, and postoperative adjuvant chemotherapy. The effects of the UFT/LV treatment on these factors were consistent (Table 2).
Treatment with UFT/LV and safety
The details of treatment with UFT/LV and its safety profile can be found in our previous report [17]. The 6-month oral UFT/LV therapy was safe and well tolerated as postoperative adjuvant chemotherapy.
Discussion
Based on the 3-year DFS improvement previously reported in this trial [17], we suggested that adjuvant UFT/LV therapy should be considered beneficial after surgery for stage II CC with a high risk of recurrence, such as T4 disease, perforation/penetration, poorly differentiated adenocarcinoma/mucinous carcinoma, and/or < 12 dissected lymph nodes. The Adjuvant Colon Cancer Endpoints (ACCENT) meta-analysis of adjuvant studies, which was performed before the approval of oxaliplatin and irinotecan for advanced disease, demonstrated that 3-year DFS is an excellent predictor of 5-year OS [22] and could be an appropriate primary endpoint for adjuvant studies in CC. Based on these findings, 3-year DFS was recognized by the US Food and Drug Administration as a primary endpoint for studies on adjuvant CC.
In this final analysis, encompassing an extended 5-year DFS period among the propensity score-matched patients, a statistically significant overall relative risk reduction of 34% for DFS events—encompassing recurrence and secondary cancer—was observed in favor of UFT/LV therapy, thus affirming the benefit previously reported 3-year DFS. However, no significant disparity was noted in the extended 5-year OS between the UFT/LV therapy and surgery-alone groups. This outcome suggests that while the 3-year DFS advantage persisted, it did not translate into a corresponding 5-year OS benefit in this study. Further analysis in ACCENT also indicated that patients with stage II CC had more prolonged survival following tumor recurrence than those with stage III CC [23]. This may explain why the significantly improved 3-year DFS in the present study did not translate into a 5-year OS benefit. The rate of 5-year OS events (all deaths) was extremely low for surgery alone (11.2%) and UFT/LV therapy (9.0%), with remarkably high 5-year OS rates of 89.0% and 91.2%, respectively. Recent improvements in chemotherapy, such as molecular targeted therapy with bevacizumab and cetuximab, as well as aggressive surgery for metastases, may have extended the survival time for patients with CC who experience postoperative recurrence [24, 25]. This possibly contributes to the prolonged survival observed after recurrence, which diminished the relationship between the 3-year DFS and 5-year OS rates in this study, which utilized a population matched by PS.
The rate of primary cancer recurrence within five years post-surgery was 18.7% (75 patients) among those treated with surgery alone and 15.8% (127 patients) among those receiving UFT/LV therapy. These figures remained consistent with those observed at the 3-year follow-up, as most postoperative relapses occurred within the initial three years. Nevertheless, 60% of patients (45 out of 75) in the surgery-alone group and 57% of patients (72 out of 127) in the UFT/LV group who experienced postoperative recurrence were still alive after five years of follow-up (data not shown). Consequently, no significant difference was observed in the 5-year OS between the surgery-alone and UFT/LV groups. Hence, an extended follow-up duration is warranted to detect potential improvements in OS following adjuvant chemotherapy, given the favorable overall prognosis of stage II CC patients. In the analysis of ACCENT, de Gramont et al. concluded that future trials evaluating adjuvant chemotherapy for stage II CC should incorporate a minimum follow-up of 6–7 years to determine a clinically relevant survival benefit [26]. Considering these findings, we believe that patients from the PS-matched population in the present study require extended follow-up for more than seven years before conclusions regarding the OS benefits of UFT/LV can be drawn.
IPTW patients treated with UFT/LV had significantly improved 5-year OS rates. This improvement could be attributed to the higher statistical power achieved by including all the patients (n = 1,880). Additionally, upon comparing hazard ratios and 95% CIs for death between IPTW patients treated with UFT/LV and those treated with surgery alone, based on baseline prognostic factors, the potential benefit of UFT/LV chemotherapy was not ruled out in the majority of defined subgroups. Furthermore, multivariate analysis revealed that UFT/LV adjuvant chemotherapy was a significant independent prognostic factor for improved OS.
Collectively, these data suggest that postoperative adjuvant chemotherapy using UFT/LV may be helpful in patients with stage II CC with risk factors for recurrence, such as T4 disease, perforation/penetration, poorly differentiated adenocarcinoma/mucinous carcinoma, and/or < 12 dissected lymph nodes. Multivariate analyses also suggested that sex, age, T4 disease, and number of dissected lymph nodes were significant risk factors for both DFS and OS in stage II CC. Moreover, based on multivariate analyses, only T4 disease, perforation/penetration, and the number of dissected lymph nodes were significant risk factors for relapse-free survival (RFS) (data not shown). Age and sex were identified as significant risk factors for both DFS and OS, considering the inclusion of secondary cancer and death due to multiple diseases. The observed results regarding recurrence risk factors may be attributed to the absence of D3 lymph node dissection, which involves comprehensive dissection of paracolic and mesenteric lymph nodes in most cases involving perforation or penetration [18]. This suggests a robust correlation between perforation/penetration and the number of dissected lymph nodes (< 12). Consequently, in line with the clinical guidelines published by ASCO [3] and ESMO [4], the depth of tumor invasion (T4) and the number of examined lymph nodes (< 12) were deemed reliable risk factors for recurrence.
Studies involving patients with stage II/III or III CC have shown that 5-fluorouracil (with or without oxaliplatin or LV), capecitabine (with or without oxaliplatin), and UFT/LV are effective adjuvant chemotherapies. However, the efficacy of these therapies in patients with stage II CC is inconsistent [12, 13, 27,28,29]. In a recent nationwide study and survey based on IPTW, long-term quality of life (QoL) diminished with adjuvant chemotherapy, with oxaliplatin-induced neurotoxicity closely associated with decreased QoL in patients with CC [30]. Therefore, we were particularly interested in adjuvant chemotherapy, which uses oral agents that are more convenient than oxaliplatin-based regimens, especially in patients with stage II CC. In this study, we applied PS matching to adjust for confounding variables to assess the effects of UFT/LV. An increasing number of studies have employed this analytical approach, and our findings suggest that it is indeed a suitable statistical method for achieving comparable distributions of observed baseline covariates. Currently, conducting a large-scale randomized clinical trial of adjuvant therapy for stage II CC with a long-term follow-up OS of > 7 years, as described above, is exceptionally challenging. Hence, we anticipate that data derived from meta-analyses and non-randomized controlled studies, analyzed using PS matching, will offer both statistically and clinically significant insights, especially concerning adjuvant therapy for stage II CC.
Despite the substantial contributions to the existing literature, our study does have some limitations. Although PS matching and IPTW were used to adjust for risk factors, some risk factors, such as microsatellite instability (MSI) [31, 32], were not considered; for instance, MSI status is known to influence the benefit of postoperative adjuvant chemotherapy with fluoropyrimidine alone in colon CC [31]. We also excluded lymphatic, vascular, and perineural invasion as risk factors due to potential inconsistencies in evaluation among the participating institutions. Further studies are necessary to validate the present results concerning the risk factors used for adjustment.
Conclusion
The outcomes of our prospective, non-randomized controlled study indicate that six months of adjuvant chemotherapy with oral UFT/LV leads to substantial survival benefits for patients with stage II CC who exhibit at least one of the following characteristics: T4 disease, perforation/penetration, poorly differentiated adenocarcinoma/mucinous carcinoma, or < 12 dissected lymph nodes. Our findings may inform tailored treatment strategies by emphasizing the importance of individual risk assessment in post-surgical care. Clinicians must judiciously evaluate the benefits of adjuvant therapy against its impact on patients’ QoL, especially given the varying responses based on risk factors such as T4 disease, perforation/penetration, and lymph node involvement. Our evidence supports a more personalized approach to treating stage II CC, guiding clinicians in making informed decisions that balance efficacy with patient well-being.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Sung H, Ferlay J, Siegel R et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249
National comprehensive cancer network. (2014) Clinical practice guidelines in oncology (NCCN Guidelines®). Colon Cancer. Version 2.2015 http://www2.tri-kobe.org/nccn/guideline/archive/colorectal2015/english/colon.pdf
Benson AB 3rd, Schrag D, Somerfield MR et al (2004) American society of clinical oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol 22:3408–3419
Schmoll HJ, Van Cutsem E, Stein A et al (2012) ESMO Consensus Guidelines for management of patients with colon and rectal cancer. A personalized approach to clinical decision making. Ann Oncol 23:2479–2516
Costas-Chavarri A, Nandakumar G, Temin S et al (2019) Treatment of patients with early-stage colorectal cancer: ASCO resource-stratified guideline. J Glob Oncol 5:1–19
Hashiguchi Y, Muro K, Saito Y et al (2020) Japanese society for cancer of the colon and rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25:1–42
Schippinger W, Samonigg H, Schaberl-Moser R et al (2007) A prospective randomised phase III trial of adjuvant chemotherapy with 5-fluorouracil and leucovorin in patients with stage II colon cancer. Br J Cancer 97:1021–1027
Eheman CR, O’Neil ME, Styles TS et al (2016) Use of adjuvant chemotherapy among stage II colon cancer patients in 10 population-based national program of cancer registries. J Registry Manag 43:179–186
Compton CC, Fielding LP, Burgart LJ et al (2000) Prognostic factors in colorectal cancer. College of American pathologists consensus statement 1999. Arch Pathol Lab Med 124:979–994
Amri R, England J, Bordeianou LG et al (2016) Risk stratification in patients with stage II colon cancer. Ann Surg Oncol 23:3907–3914
O’Connor ES, Greenblatt DY, LoConte NK et al (2011) Adjuvant chemotherapy for stage II colon cancer with poor prognostic features. J Clin Oncol 29:3381–3388
Tournigand C, Andre T, Bonnetain F et al (2012) Adjuvant therapy with fluorouracil and oxaliplatin in stage II and elderly patients (between ages 70 and 75 years) with colon cancer: subgroup analyses of the multicenter international study of oxaliplatin, fluorouracil, and leucovorin in the adjuvant treatment of colon cancer trial. J Clin Oncol 30:3353–3360
Lembersky BC, Wieand HS, Petrelli NJ et al (2006) Oral uracil and tegafur plus leucovorin compared with intravenous fluorouracil and leucovorin in stage II and III carcinoma of the colon: results from national surgical adjuvant breast and bowel project protocol C-06. J Clin Oncol 24:2059–2064
Kopec JA, Yothers G, Ganz PA et al (2007) Quality of life in operable colon cancer patients receiving oral compared with intravenous chemotherapy: results from national surgical adjuvant breast and bowel project trial C-06. J Clin Oncol 25:424–430
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28:3083–3107
Sadahiro S, Sakamoto K, Tsuchiya T et al (2022) Prospective observational study of the efficacy of oral uracil and tegafur plus leucovorin for stage II colon cancer with risk factors for recurrence using propensity score matching (JFMC46-1201). BMC Cancer 22:170
Sugimoto K, Sakamoto K, Tsuchiya T et al (2023) Prognostic factors in patients with high-risk stage II colon cancer after curative resection: a post hoc analysis of the JFMC46-1201 trial. Int J Colorectal Dis 38:260
Sadahiro S, Morita S, Sasaki K et al (2015) Treatment rationale and study design for clinical trial on the efficacy of UFT/LV for stage II colorectal cancer with risk factors for recurrence (JFMC46-1201). Clin Colorectal Cancer 14:277–280
Robins JM, Hernan MA, Brumback B (2000) Marginal structural models and causal inference in epidemiology. Epidemiology 11:550–560
Stefanski LA, Boos DD (2002) The calculus of m-estimation. Am Stat 56:29–38
Sargent DJ, Wieand HS, Haller DG et al (2005) Disease-free survival versus overall survival as a primary end point for adjuvant colon cancer studies: individual patient data from 20,898 patients on 18 randomized trials. J Clin Oncol 23:8664–8670
O’Connell MJ, Campbell ME, Goldberg RM et al (2008) Survival following recurrence in stage II and III colon cancer: findings from the ACCENT data set. J Clin Oncol 26:2336–2341
You XH, Jiang YH, Fang Z et al (2020) Chemotherapy plus bevacizumab as an optimal first-line therapeutic treatment for patients with right-sided metastatic colon cancer: a meta-analysis of first-line clinical trials. ESMO Open. https://doi.org/10.1136/esmoopen-2019-000605
Mody K, Bekaii-Saab T (2018) Clinical trials and progress in metastatic colon cancer. Surg Oncol Clin N Am 27:349–365
de Gramont A, Hubbard J, Shi Q et al (2010) Association between disease-free survival and overall survival when survival is prolonged after recurrence in patients receiving cytotoxic adjuvant therapy for colon cancer: simulations based on the 20,800 patient ACCENT data set. J Clin Oncol 28:460–465
Andre T, Boni C, Mounedji-Boudiaf L et al (2004) Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 350:2343–2351
Matsuda C, Ishiguro M, Teramukai S et al (2018) A randomised-controlled trial of 1-year adjuvant chemotherapy with oral tegafur-uracil versus surgery alone in stage II colon cancer: SACURA trial. Eur J Cancer 96:54–63
Andre T, Boni C, Navarro M et al (2009) Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 27:3109–3116
Malik YG, Benth JS, Hamre HM et al (2024) Chemotherapy reduces long-term quality of life in recurrence-free colon cancer survivors (LaTE study)-a nationwide inverse probability of treatment-weighted registry-based cohort study and survey. Colorectal Dis 26:22–33
Ribic CM, Sargent DJ, Moore MJ et al (2003) Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 349:247–257
Saridaki Z, Souglakos J, Georgoulias V (2014) Prognostic and predictive significance of MSI in stages II/III colon cancer. World J Gastroenterol 20:6809–6814
Acknowledgements
This study was supported by the Japanese Foundation for Multidisciplinary Treatment of Cancer. We would like to thank Editage (www.editage.com) for editing the English language.
Funding
This work was supported by Taiho Pharmaceutical Co., Ltd. (grant number: not applicable). The funder of this study had no role in the study design, data collection, analysis, and interpretation; writing, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
YO: data curation, formal analysis, investigation, resources, writing–original draft, and writing–review and editing. SS: conceptualization, data curation, formal analysis, investigation, project administration, resources, writing–original draft, and writing–review and editing. KS: data curation, resources, and writing–review and editing. TTsu: data curation, resources, and writing–review and editing. TTak: data curation, resources, and writing–review and editing. HO: data curation, resources, and writing–review and editing. TS: data curation, resources, and writing–review and editing. KK: data curation, resources, and writing–review and editing. HB: data curation, resources, and writing–review and editing. MIta: data curation, resources, and writing–review and editing. MIke: data curation, resources, and writing–review, and editing. MH: data curation, resources, and writing–review and editing. KM: data curation, resources, and writing–review and editing. HM: data curation, resources, and writing–review and editing. KT: data curation, resources, and writing–review and editing. MK: formal analysis and writing–review and editing. IH: formal analysis and writing, including review and editing. JS: formal analysis and writing–review and editing. MT: formal analysis, writing–original draft, and writing–review and editing. SM: conceptualization, data curation, investigation, writing–original draft, and writing–review and editing. The authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare the following financial interests/personal relationships, which may be considered potential competing interests: Takao Takahashi was awarded an endowed chair from Yakult Honsha outside the submitted work. Outside the submitted work, Hideo Baba received a grant and personal fees from Taiho Pharmaceutical. Outside the submitted work, Ichinosuke Hyodo received grants and personal fees from Taiho Pharmaceutical, Asahi Kasei Pharma, Chugai Pharmaceutical, Eisai, and Ono Pharmaceutical. Satoshi Morita received personal fees outside the submitted work from Bristol-Myers Squibb, Chugai Pharmaceutical, Taiho Pharmaceutical, Eli Lilly Japan, and AstraZeneca. All other authors have no conflicts of interest to declare.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ogata, Y., Sadahiro, S., Sakamoto, K. et al. Final analyses of the prospective controlled trial on the efficacy of uracil and tegafur/leucovorin as an adjuvant treatment for stage II colon cancer with risk factors for recurrence using propensity score-based methods (JFMC46-1201). Int J Clin Oncol 29, 1284–1292 (2024). https://doi.org/10.1007/s10147-024-02565-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-024-02565-5