Abstract
Background
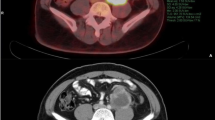
Survival in patients with retroperitoneal liposarcoma (RPLS) depends on the surgical management of the dedifferentiated foci. The present study investigated the diagnostic yield of contrast-enhanced CT, 18F-fluorodeoxyglucose positron emission tomography (PET), and diffusion-weighted MRI in terms of dedifferentiated foci within the RPLS.
Methods
Patients treated with primary or recurrent RPLS who underwent the above imaging between January 2010 and December 2021 were retrospectively reviewed. The diagnostic accuracy of the three modalities for histologic subtype of dedifferentiated liposarcoma (DDLS) and French Federation of Cancer Center (FNCLCC) grade 2/3 were compared using receiver operating characteristic curves and areas under the curves (AUCs).
Results
The cohort involved 32 patients with 53 tumors; 30 of which exhibited DDLS and 31 of which did FNCLCC grades 2/3. The optimal thresholds for predicting DDLS were mean CT value of 31 Hounsfield Unit (HU) (AUC = 0.880, 95% CI 0.775–0.984; p < 0.001), maximum standardized uptake value (SUVmax) of 2.9 (AUC = 0.865 95% CI 0.792–0.980; p < 0.001), while MRI failed to differentiate DDLS. The cutoff values for distinguishing FNCLCC grades 1 and 2/3 were a mean CT value of 24 HU (AUC = 0.858, 95% CI 0.731–0.985; p < 0.001) and SUVmax of 2.9 (AUC = 0.885, 95% CI 0.792–0.978; p < 0.001). MRI had no sufficient power to separate these grades.
Conclusions
Contrast-enhanced CT and PET were useful for predicting DDLS and FNCLCC grade 2/3, while MRI was inferior to these two modalities.





Similar content being viewed by others
References
Matthyssens LE, Creytens D, Ceelen WP (2015) Retroperitoneal liposarcoma: current insights in diagnosis and treatment. Front Surg. https://doi.org/10.3389/fsurg.2015.00004
Brennan MF, Antonescu CR, Moraco N et al (2014) Lessons learned from the study of 10,000 patients with soft tissue sarcoma. Ann Surg 260(3):416–422
Dehner CA, Hagemann IS, Chrisinger JSA (2021) Retroperitoneal dedifferentiated liposarcoma. Am J Clin Pathol 56(5):920–925
Lahat G, Madewell JE, Anaya DA et al (2009) Computed tomography scan-driven selection of treatment for retroperitoneal liposarcoma histologic subtypes. Cancer 115(5):1081–1090
Bhosale P, Wang J, Varma D et al (2016) Can abdominal computed tomography imaging help accurately identify a dedifferentiated component in a well-differentiated liposarcoma? J Comput Assist Tomogr 40(6):872–879
Parkes A, Urquiola E, Bhosale P et al (2020) PET/CT imaging as a diagnostic tool in distinguishing well-differentiated versus dedifferentiated Liposarcoma. Sarcoma. https://doi.org/10.1155/2020/8363986
Li CP, Liu DN, Zhou NN et al (2021) Prediction of histologic subtype and FNCLCC grade by SUVmax measured on 18F-FDG PET/CT in patients with retroperitoneal Liposarcoma. Contrast Media Mol Imaging. https://doi.org/10.1155/2021/7191363
Subramaniam S, Callahan J, Bressel M et al (2021) The role of 18F-FDG PET/CT in retroperitoneal sarcomas-a multicenter retrospective study. J Surg Oncol 123(4):1081–1087
Koh D-M, Collins DJ (2007) Diffusion-weighted MRI in the body: applications and challenges in oncology. AJR Am J Roentgenol 188(6):1622–1635
Padhani AR, Liu G, Koh DM et al (2009) Diffusion-weighted magnetic resonance imaging as a cancer biomarker: consensus and recommendations. Neoplasia 11(2):102–125
Bozgeyik Z, Onur MR, Poyraz AK (2013) The role of diffusion weighted magnetic resonance imaging in oncologic settings. Quant Imaging Med Surg 3(5):269–278
Sbaraglia M, Bellan E, Dei Tos AP (2021) The 2020 WHO classification of soft tissue tumours: news and perspectives. Pathologica 113(2):70–84
Guillou L, Coindre JM, Bonichon F et al (1997) Comparative study of the national cancer institute and French federation of cancer centers sarcoma group grading systems in a population of 410 adult patients with soft tissue sarcoma. J Clin Oncol 15(1):350–362
Xue G, Wang Z, Li C et al (2021) A novel nomogram for predicting local recurrence-free survival after surgical resection for retroperitoneal liposarcoma from a Chinese tertiary cancer center. Int J Clin Oncol 26(1):145–153
van Houdt WJ, Fiore M, Barretta F et al (2020) Patterns of recurrence and survival probability after second recurrence of retroperitoneal sarcoma: A study from TARPSWG. Cancer 126(22):4917–4925
Gronchi A, Strauss DC, Miceli R et al (2016) Variability in patterns of recurrence after resection of primary retroperitoneal sarcoma (RPS): a report on 1007 patients from the multi-institutional collaborative rps working group. Ann Surg 263(5):1002–1009
Singer S, Antonescu CR, Riedel E et al (2003) Histologic subtype and margin of resection predict pattern of recurrence and survival for retroperitoneal liposarcoma. Ann Surg 238(3):358–370
Tseng WW, Madewell JE, Wei W et al (2014) Locoregional disease patterns in well-differentiated and dedifferentiated retroperitoneal liposarcoma: implications for the extent of resection? Ann Surg Oncol 21(7):2136–2143
Jensen OM, Høgh J, Ostgaard SE et al (1991) Histopathological grading of soft tissue tumours prognostic significance in a prospective study of 278 consecutive cases. J Pathol 163(1):19–24
Neuhaus SJ, Barry P, Clark MA et al (2005) Surgical management of primary and recurrent retroperitoneal liposarcoma. Br J Surg 92(2):246–252
Linehan DC, Lewis JJ, Leung D et al (2000) Influence of biologic factors and anatomic site in completely resected liposarcoma. J Clin Oncol 18(8):1637–1643
Jha AK, Rodríguez JJ, Stopeck AT (2016) A maximum-likelihood method to estimate a single ADC value of lesions using diffusion MRI. Magn Reson Med 76(6):1919–1931
Walker-Samuel S, Orton M, Boult JKR et al (2011) Improving apparent diffusion coefficient estimates and elucidating tumor heterogeneity using Bayesian adaptive smoothing. Magn Reson Med 65(2):438–447
Walker-Samuel S, Orton M, McPhail LD et al (2009) Robust estimation of the apparent diffusion coefficient (ADC) in heterogeneous solid tumors. Magn Reson Med 62(2):420–429
Muzaffar R, Koester E, Frye S et al (2020) Development of simple methods to reduce the exposure of the public to radiation from patients who have undergone 18F-FDG PET/CT. J Nucl Med Technol 48(1):63–67
Shaish H, Kang SK, Rosenkrantz AB (2017) The utility of quantitative ADC values for differentiating high-risk from low-risk prostate cancer: a systematic review and meta-analysis. Abdom Radiol (NY) 42(1):260–270
Hou B, Xiang S-F, Yao G-D et al (2014) Diagnostic significance of diffusion-weighted MRI in patients with cervical cancer: a meta-analysis. Tumour Biol 35(12):11761–11769
Gabelloni M, Faggioni L, Neri E (2019) Imaging biomarkers in upper gastrointestinal cancers. BJR Open. https://doi.org/10.1259/bjro.20190001
Schurink NW, Lambregts DMJ, Beets-Tan RGH (2019) Diffusion-weighted imaging in rectal cancer: current applications and future perspectives. Br J Radiol 92(1096):20180655
Satoh S, Kitazume Y, Ohdama S et al (2008) Can malignant and benign pulmonary nodules be differentiated with diffusion-weighted MRI? AJR Am J Roentgenol 191(2):464–470
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Nakashima, Y., Yokoyama, Y., Ogawa, H. et al. Which modality is better to diagnose high-grade transformation in retroperitoneal liposarcoma? Comparison of computed tomography, positron emission tomography, and magnetic resonance imaging. Int J Clin Oncol 28, 482–490 (2023). https://doi.org/10.1007/s10147-022-02287-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-022-02287-6