Abstract
Background
The most widely accepted staging system for colorectal cancer (CRC) is the tumor-node-metastasis (TNM) classification. In Japan, the Japanese Classification of Colorectal, Appendiceal, and Anal Carcinoma (JCCRC) system is used. The two systems differ mainly in relation to tumor deposits (TD) and metastasis in the regional lymph nodes along the main feeding arteries and lateral pelvic lymph nodes (N3). Here, we investigated the prognostic ability of the two systems for stage III CRC.
Methods
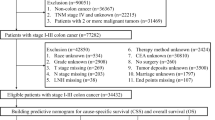
We reviewed 696 consecutive patients who underwent curative resection of stage III CRC at the National Cancer Center Hospital between May 2007 and April 2014. We examined the clinicopathological features of CRC and predicted overall survival (OS) and relapse-free survival (RFS) according to the 8th TNM and 9th JCCRC systems. The systems were compared using Akaike’s information criterion (AIC), Harrell’s concordance index (C-index), and time-dependent receiver-operating characteristic (ROC) curves.
Results
The 9th JCCRC system was more clinically effective according to AIC (OS, 1199 vs. 1206; RFS, 2047 vs. 2057), showed better discriminatory ability according to the C-index (OS, 0.65 vs. 0.62; RFS, 0.62 vs. 0.58), and its time-dependent ROC curve was superior compared with the 8th TNM system.
Conclusion
These results suggest that the 9th JCCRC system has superior discriminative ability to the 8th TNM system, because the 9th JCCRC accounts for the presence of TD and N3 disease, which were both significant predictors of poor prognosis. Reconsidering the clinical value of these two factors in the TNM system could improve its clinical significance.


Similar content being viewed by others
Abbreviations
- AIC:
-
Akaike’s information criterion
- AUC:
-
Area under the curve
- CRC:
-
Colorectal cancer
- EX:
-
Extramural cancer deposits without lymph node structure
- JCCRC:
-
Japanese Classification of Colorectal, Appendiceal, and Anal Carcinoma
- JSCCR:
-
Japanese Society for Cancer of the Colon and Rectum
- LLNM:
-
Lateral pelvic lymph node metastasis
- LPLN:
-
Lateral pelvic lymph node
- MLN:
-
Main lymph node
- MLNM:
-
Main lymph node metastasis
- ND:
-
Tumor nodules
- OS:
-
Overall survival
- RFS:
-
Relapse-free survival
- ROC:
-
Receiver-operating characteristic
- TD:
-
Tumor deposits
- TNM:
-
Tumor-node-metastasis
- UICC:
-
Union for International Cancer Control
References
UICC (2017) TNM classification of malignant tumours, 8th edn. Wiley, New York
JSCCR (2018) Japanese classification of colorectal, appendiceal, and anal carcinoma, 9th edn. Kanehara & Co. Ltd, Tokyo
Shida D, Kanemitsu Y, Hamaguchi T et al (2019) Introducing the eighth edition of the tumor-node-metastasis classification as relevant to colorectal cancer, anal cancer and appendiceal cancer: a comparison study with the seventh edition of the tumor-node-metastasis and the Japanese classification of colorectal, appendiceal, and anal carcinoma. Jpn J Clin Oncol 49(4):321–328. https://doi.org/10.1093/jjco/hyy198
Shinto E, Hida JI, Ike H et al (2018) A new N staging system for colorectal cancer in the era of extended lymphadenectomy. Ann Surg Oncol 25(13):3891–3897. https://doi.org/10.1245/s10434-018-6786-x
Hashiguchi Y, Muro K, Saito Y et al (2020) Japanese society for cancer of the colon and rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25(1):1–42. https://doi.org/10.1007/s10147-019-01485-z
Shinto E, Hida JI, Kobayashi H et al (2018) Prominent information of jN3 positive in stage III colorectal cancer removed by D3 dissection: retrospective analysis of 6866 patients from a multi-institutional database in Japan. Dis Colon Rectum 61(4):447–453. https://doi.org/10.1097/DCR.0000000000001009
Han L, Mo S, Xiang W et al (2019) Prognostic accuracy of different lymph node staging system in predicting overall survival in stage IV colon cancer. Int J Colorectal Dis. https://doi.org/10.1007/s00384-019-03486-w
Komori K, Fujita S, Mizusawa J et al (2019) Predictive factors of pathological lateral pelvic lymph node metastasis in patients without clinical lateral pelvic lymph node metastasis (clinical stage II/III): the analysis of data from the clinical trial (JCOG0212). Eur J Surg Oncol 45(3):336–340. https://doi.org/10.1016/j.ejso.2018.11.016
Fujita S, Yamamoto S, Akasu T et al (2003) Lateral pelvic lymph node dissection for advanced lower rectal cancer. Br J Surg 90(12):1580–1585. https://doi.org/10.1002/bjs.4350
Ueno M, Oya M, Azekura K et al (2005) Incidence and prognostic significance of lateral lymph node metastasis in patients with advanced low rectal cancer. Br J Surg 92(6):756–763. https://doi.org/10.1002/bjs.4975
Sugihara K, Kobayashi H, Kato T et al (2006) Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum 49(11):1663–1672. https://doi.org/10.1007/s10350-006-0714-z
Ueno H, Mochizuki H, Hashiguchi Y et al (2007) Extramural cancer deposits without nodal structure in colorectal cancer optimal categorization for prognostic staging. Am J Clin Pathol 127:287–294. https://doi.org/10.1309/903UT10VQ3LC7B8L
Ueno H, Mochizuki H, Akagi Y et al (2012) Optimal colorectal cancer staging criteria in TNM classification. J Clin Oncol 30(13):1519–1526. https://doi.org/10.1200/jco.2011.39.4692
Chen VW, Hsieh MC, Charlton ME et al (2014) Analysis of stage and clinical/prognostic factors for colon and rectal cancer from SEER registries: AJCC and collaborative stage data collection system. Cancer 120(Suppl 23):3793–3806. https://doi.org/10.1002/cncr.29056
Wong-Chong N, Motl J, Hwang G et al (2018) Impact of tumor deposits on oncologic outcomes in stage III colon cancer. Dis Colon Rectum 61(9):1043–1052. https://doi.org/10.1097/dcr.0000000000001152
Basnet S, Lou Q-F, Liu N et al (2018) Tumor deposit is an independent prognostic indicator in patients who underwent radical resection for colorectal cancer. J Cancer 9(21):3979–3985. https://doi.org/10.7150/jca.27475
Pellino G, Warren O, Mills S et al (2018) Comparison of Western and Asian guidelines concerning the management of colon cancer. Dis Colon Rectum 61(2):250–259. https://doi.org/10.1097/dcr.0000000000001012
Kamarudin AN, Cox T, Kolamunnage-Dona R (2017) Time-dependent ROC curve analysis in medical research: current methods and applications. BMC Med Res Methodol 17(1):53–53. https://doi.org/10.1186/s12874-017-0332-6
Nagayoshi K, Ueki T, Nishioka Y et al (2014) Tumor deposit is a poor prognostic indicator for patients who have stage II and III colorectal cancer with fewer than 4 lymph node metastases but not for those with 4 or more. Dis Colon Rectum 57(4):467–474. https://doi.org/10.1097/dcr.0000000000000059
Tong LL, Gao P, Wang ZN et al (2012) Is the seventh edition of the UICC/AJCC TNM staging system reasonable for patients with tumor deposits in colorectal cancer? Ann Surg 255(2):208–213. https://doi.org/10.1097/SLA.0b013e31821ad8a2
Song YX, Gao P, Wang ZN et al (2012) Can the tumor deposits be counted as metastatic lymph nodes in the UICC TNM staging system for colorectal cancer? PLoS ONE 7(3):e34087. https://doi.org/10.1371/journal.pone.0034087
Jin M, Roth R, Rock JB et al (2015) The impact of tumor deposits on colonic adenocarcinoma AJCC TNM staging and outcome. Am J Surg Pathol 39(1):109–115. https://doi.org/10.1097/pas.0000000000000320
Wang S, Guan X, Ma M et al (2020) Reconsidering the prognostic significance of tumour deposit count in the TNM staging system for colorectal cancer. Sci Rep 10(1):89. https://doi.org/10.1038/s41598-019-57041-2
Bertelsen CA, Neuenschwander AU, Jansen JE et al (2015) Disease-free survival after complete mesocolic excision compared with conventional colon cancer surgery: a retrospective, population-based study. Lancet Oncol 16(2):161–168. https://doi.org/10.1016/s1470-2045(14)71168-4
Blanche P, Dartigues JF, Jacqmin-Gadda H (2013) Estimating and comparing time-dependent areas under receiver operating characteristic curves for censored event times with competing risks. Stat Med 32(30):5381–5397. https://doi.org/10.1002/sim.5958
Blanche P, Kattan MW, Gerds TA (2019) The c-index is not proper for the evaluation of $t$-year predicted risks. Biostatistics 20(2):347–357. https://doi.org/10.1093/biostatistics/kxy006
Bansal A, Heagerty PJ (2018) A tutorial on evaluating the time-varying discrimination accuracy of survival models used in dynamic decision making. Med Decis Making 38(8):904–916. https://doi.org/10.1177/0272989x18801312
Funding
None to report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No author has any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Kitamura, K., Shida, D., Sekine, S. et al. Comparison of model fit and discriminatory ability of the 8th edition of the tumor-node-metastasis classification and the 9th edition of the Japanese classification to identify stage III colorectal cancer. Int J Clin Oncol 26, 1671–1678 (2021). https://doi.org/10.1007/s10147-021-01955-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-021-01955-3