Abstract
Purpose
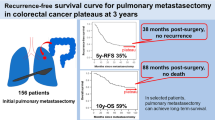
The aim of this study was to elucidate a potential risk factor for early relapse after pulmonary metastasectomy of colorectal cancer and to propose an optimal treatment strategy for lung metastasis with an aggressive nature.
Methods
Seventy patients who underwent pulmonary metastasectomy for diachronically measurable pulmonary lesions were retrospectively analyzed. We calculated the tumor doubling time (TDT) as the growth rate of lung metastasis and divided the study population into two groups: Rapid (TDT ≤ 100 days) and Slow (TDT > 100 days).
Results
The patients consisted of 47 males and 23 females, with a mean age of 63 years. Forty-two patients had a relapse after pulmonary metastasectomy with a median follow-up duration of 24 months. There was a significant difference in relapse-free survival between the Rapid and Slow groups (p = 0.047). Using a multivariate analysis, no preoperative chemotherapy and a high level of serum carcinoembryonic antigen were proven to be significant risk factors for relapse after metastasectomy. Meanwhile, multivariate analyses among 37 patients without preoperative chemotherapy indicated that TDT was the sole significant factor for relapse-free survival. In addition, eight of nine patients with relapse within 12 months were placed into the Rapid group.
Conclusions
Although this was a preliminary study with a small number of patients, it suggested that lung metastases demonstrating a TDT of 100 days or less have a high risk of early relapse after metastasectomy.


Similar content being viewed by others
References
Onaitis MW, Petersen RP, Haney JC et al (2009) Prognostic factors for recurrence after pulmonary resection of colorectal cancer metastases. Ann Thorac Surg 87:1684–1688
Iida T, Nomori H, Shiba M et al (2013) Prognostic factors after pulmonary metastasectomy for colorectal cancer and rationale for determining surgical indications: a retrospective analysis. Ann Surg 257:1059–1064
Nordlinger B, Sorbye H, Glimelius B et al (2008) Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet 371:1007–1016
Usuda K, Saito Y, Sagawa M et al (1994) Tumor doubling time and prognostic assessment of patients with primary lung cancer. Cancer 74:2239–2244
Friberg S, Mattson S (1997) On the growth rates of human malignant tumors: implications for medical decision making. J Surg Oncol 65:284–297
Schwartz M (1961) A biomathematical approach to clinical tumor growth. Cancer 14:1272–1294
Kanemitsu Y, Kato T, Hirai T, Yasui K (2004) Preoperative probability model for predicting overall survival after resection of pulmonary metastases from colorectal cancer. Br J Surg 91:112–120
Golfinopoulos V, Salanti G, Pavlidis N, Ioannidis JP (2007) Survival and disease-progression benefits with treatment regimens for advanced colorectal cancer: a meta-analysis. Lancet Oncol 8:898–911
Takei H, Kondo H, Miyaoka E et al (2014) Surgery for small cell lung cancer: a retrospective analysis of 243 patients from Japanese Lung Cancer Registry in 2004. J Thorac Oncol 9:1140–1145
Tjandra JJ, Chan MK (2007) Follow-up after curative resection of colorectal cancer: a meta-analysis. Dis Colon Rectum 50:1783–1799
NCC Network. NCCN Clinical Practice Guidelines in Oncology. Version 2.2013
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kohei Yokoi received a research grant from the Takeda Science Foundation.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10147_2015_889_MOESM1_ESM.tif
Three cases of pulmonary metastasectomy. (A) No need of perioperative chemotherapy. A 74-year-old female had a solitary pulmonary nodule of 10 mm in diameter in her left upper lobe at the time of resection for the primary colon cancer (left). The size of the pulmonary nodule increased to 13 mm seven months after colectomy, and the TDT was calculated to be 189 days (right). The lesion was proven to be a metastasis by VATS excision, and she is currently in a stable condition 6 years after the metastasectomy without receiving chemotherapy (TIFF 265 kb)
10147_2015_889_MOESM2_ESM.tif
(B) Early relapse after metastasectomy. A 63-year-old male had a lung metastasis in his left lower lobe 20 months after resection of the colon cancer (left). The pulmonary lesion rapidly grew, and the TDT was 32 days (right). He had bone metastasis nine months after segmentectomy for the lung metastasis and died four months later (TIFF 389 kb)
10147_2015_889_MOESM3_ESM.tif
(C) Preoperative chemotherapy followed by metastasectomy. A 71-year-old male had a lung metastasis and the TDT was calculated to be 44 days (left to middle). Preoperative chemotherapy was administered, and the tumor size decreased from 15 to 7 mm (middle to right). Right upper lobectomy was performed and he is currently in a stable condition 26 months after metastasectomy without relapse (TIFF 228 kb)
About this article
Cite this article
Kawaguchi, K., Uehara, K., Nakayama, G. et al. Growth rate of chemotherapy-naïve lung metastasis from colorectal cancer could be a predictor of early relapse after lung resection. Int J Clin Oncol 21, 329–334 (2016). https://doi.org/10.1007/s10147-015-0889-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-015-0889-1



