Abstract
Retrospective observational study. To determine the efficacy and safety of bioactive glass ceramics mixed with autograft in the treatment of spondylodiscitis. Thirty-four patients with spondylodiscitis underwent surgery using autologous bone graft augmented by antibiotic loaded bioactive glass ceramic granules. Twenty-five patients aging 6 to 77, completed 1-year follow-up. The lumbosacral junction was affected in 3, lumbar spine in 13, one each in the dorso-lumbar junction and sacrum, and 7 dorsal spines. The organism isolated was Mycobacterium tuberculosis in 15, Methicillin sensitive Staphylococcus aureus (MSSA) in 4, Pseudomonas aeruginosa in 4, Klebsiella pneumoniae in one, Burkholderia pseudomallei in 1, and mixed infections in 2. All patients had appropriate antibiotic therapy based on culture and sensitivity. Clinical and radiological evaluation of all the patients was done at 6 weeks, 3 months, 6 months, and 12 months after the surgery. Twenty-three patients improved clinically and showed radiographic fusion between 6 and 9 months. The patient with Burkholderia infection died due to fulminant septicemia with multi organ failure while another patient died at 9 months due to an unrelated cardiac event. The mean Visual Analogue Score (VAS) at the end of 1-year was 2 with radiological evidence of fusion in all patients. There were no re-infections or discharging wounds, and the 30-day re-admission rate was 0. Bioactive glass ceramics is a safe and effective graft expander in cases of spondylodiscitis. The absorption of antibiotics into the ceramic appears to help the elimination of infection.








Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Albee FH (1920) Studies in bone growth: triple calcium phosphate as a stimulus to osteogenesis. Ann Surg 71(1):32–39. https://doi.org/10.1097/00000658-192001000-00006
Pape HC, Evans A, Kobbe P (2010) Autologous bone graft: properties and techniques. J Orthop Trauma 24(Suppl 1):S36-40. https://doi.org/10.1097/BOT.0b013e3181cec4a1
Khan SN, Cammisa FP Jr, Sandhu HS, Diwan AD, Girardi FP, Lane JM (2005) The biology of bone grafting. J Am Acad Orthop Surg 13(1):77–86
Dimitriou R, Mataliotakis GI, Angoules AG, Kanakaris NK, Giannoudis PV (2011) Complications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic review. Injury 42(Suppl 2):S3-15. https://doi.org/10.1016/j.injury.2011.06.015
Albee FH (1996) Bone graft surgery. Clin Orthop Relat Res 324:5–12. https://doi.org/10.1097/00003086-199603000-00002
Köster K, Karbe E, Kramer H, Heide H, König R (1976) Experimenteller Knochenersatz durch resorbierbare Calciumphosphat-Keramik [Experimental bone replacement with resorbable calcium phosphate ceramic (author’s transl)]. Langenbecks Arch Chir 341(2):77–86. https://doi.org/10.1007/BF01262779. (German)
Branemark PI (1983) Osteointegration and its experimental background. J Prosthetic Dent 50:399–410. https://doi.org/10.1016/S0022-3913(83)80101-2
Baino F, Novajra G, Vitale-Brovarone C (2015) Bioceramics and Scaffolds: a winning combination for tissue engineering. Front Bioeng Biotechnol 3:202. https://doi.org/10.3389/fbioe.2015.00202
Hench LL, Splinter RJ, Allen WC, Greenlee TK (1971) Bonding mechanisms at the interface of ceramic prosthetic materials. J Biomed Mater Res 5:117–141. https://doi.org/10.1002/jbm.820050611
Hench LL (2006) The story of bioglass. J Mater Sci Mater Med 17(11):967–78. https://doi.org/10.1007/s10856-006-0432-z
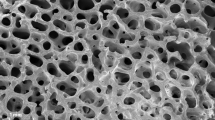
Barberi J, Baino F, Fiume E, Orlygsson G, Nommeots-Nomm A, Massera J, Verné E (2019) Robocasting of SiO2-based bioactive glass scaffolds with porosity gradient for bone regeneration and potential load-bearing applications. Mater (Basel) 12(17):2691. https://doi.org/10.3390/ma12172691
Varma HK, Sivakumar R (1996) Preparation and characterization of free flowing hydroxyapatite powders. Phosphorus Res Bull 6:35–38. https://doi.org/10.3363/prb1992.6.0_35
Srinivasan A, Varma HK, Kumary TV, John A et al (2002) Preliminary in vitro and in vivo characterization of a sol–gel derived bioactive glass–ceramic system. Bull Mater Sci 25(5):419–429. https://doi.org/10.1007/BF02708021
John A, Varma HK, Kumari TV, Nisha VR, Narayanan D (2005) Cytocompatibility studies of a novel bioactive glass coated porous hydroxyapatite bioceramic for use as a bone substitute. Key Eng Mater 284–286:317–320. https://doi.org/10.4028/www.scientific.net/kem.284-286.317
Jain AK, Rajasekaran S, Raj JK, Myneedu VP (2020) Tuberculosis of the Spine. J Bone Joint Surg 102(7):617–628. https://doi.org/10.2106/JBJS.19.00001
Kehrer M, Pedersen C, Jensen TG, Lassen AT (2014) Increasing incidence of pyogenic spondylodiscitis: A 14-year population-based study. J Infect 68(4):313–320. https://doi.org/10.1016/j.jinf.2013.11.011. (ISSN 0163-4453)
Pola E, Taccari F, Autore G et al (2018) Multidisciplinary management of pyogenic spondylodiscitis: epidemiological and clinical features, prognostic factors and long- term outcomes in 207 patients. Eur Spine J 27(Suppl 2):229–236. https://doi.org/10.1007/s00586-018-5598-9
Menon KV, Tamer MMS (2016) Epidemiologic and demographic attributes of primary spondylodiscitis in a Middle Eastern population sample. World Neurosurg 295:31–9. https://doi.org/10.1016/j.wneu.2016.07.088. (S1878- 8750(16)30632-5)
Simon D, Manuel S, Varma H (2013) Novel nanoporous bioceramic spheres for drug delivery application: a preliminary in vitro investigation. Oral Surg Oral Med Oral Pathol Oral Radiol 115(3):e7-14. https://doi.org/10.1016/j.oooo.2011.10.021
Wu C, Zreiqat H (2010) Porous bioactive diopside (CaMgSi(2)O(6)) ceramic microspheres for drug delivery. Acta Biomater 6(3):820–829. https://doi.org/10.1016/j.actbio.2009.09.025
Romagnoli C, D’Asta F, Brandi ML (2013) Drug delivery using composite scaffolds in the context of bone tissue engineering. Clin Cases Miner Bone Metab 10(3):155–161
Michelinakis E (1972) Treatment of chronic osteomyelitis with the continuous irrigation-suction method. Acta Orthop Scand 43(1):25–31. https://doi.org/10.3109/17453677208988660
Jeanneret B, Magerl F (1994) Treatment of osteomyelitis of the spine using percutaneous suction/irrigation and percutaneous external spinal fixation. J Spinal Disord 7(3):185–205. https://doi.org/10.1097/00002517-199407030-00001
Walenkamp GH, Vree TB, Vanrens TJ (1986) Gentamicin–PMMA Beads: Pharmacokinetic and Nephrotoxicological Study. Clin Orthop Relat Res 205:171–183
Seligson D, Berling S (2015) Antibiotic-laden PMMA bead chains for the prevention of infection in compound fractures: current state of the art. Eur J Orthop Surg Traumatol 25(6):969–974. https://doi.org/10.1007/s00590-015-1652-z
Ge SM, Harvey EJ (2021) Collagen fleece in orthopaedic infections. OTA Int 4(3):e111. https://doi.org/10.1097/OI9.0000000000000111
van Vugt TAG, Walraven JMB, Geurts JAP, Arts JJC (2018) Antibiotic-loaded collagen sponges in clinical treatment of chronic osteomyelitis: a systematic review. J Bone Joint Surg Am 100(24):2153–2161. https://doi.org/10.2106/JBJS.17.01140
Nagineni VV, James AR, Alimi M, Hofstetter C, Shin BJ, Njoku I Jr, Tsiouris AJ, Härtl R (2012) Silicate-substituted calcium phosphate ceramic bone graft replacement for spinal fusion procedures. Spine (Phila Pa 1976) 37(20):E1264-72. https://doi.org/10.1097/BRS.0b013e318265e22e
Alimi M, Navarro-Ramirez R, Parikh K, Njoku I, Hofstetter CP, Tsiouris AJ, Härtl R (2017) Radiographic and clinical outcome of silicate-substituted calcium phosphate (Si-CaP) ceramic bone graft in spinal fusion procedures. Clin Spine Surg 30(6):E845-52. https://doi.org/10.1097/BSD.0000000000000432
Menon KV, Varma HK (2005) Tibial plateau fractures treated with percutaneously introduced synthetic porous hydroxyapatite granules. Eur J Orthop Surg Traumatol 15(3):205–213
Acharya KN, Kumar RJ, Varma HK, Menon KV (2008) Hydroxyapatite-bioactive glass ceramic composite as standalone graft substitute for posterolateral fusion of lumbar spine: a prospective matched and controlled study. J Spinal Disord Tech 21(2):106–1121 (Drug Eluting Ceramics in the Field of Spinal Infections)
Inzana JA, Schwarz EM, Kates SL, Awad HA (2016) Biomaterials approaches to treating implant associated osteomyelitis. Biomaterials 81:58–71
Menon VK, Kumar KM, Al GK (2014) One-stage biopsy, debridement, reconstruction, and stabilization of pyogenic vertebral osteomyelitis. Global Spine J 4(2):93–99. https://doi.org/10.1055/s-0034-1370789
Salamanna F, Tschon M, Borsari V, Pagani S, Martini L, Fini M (2020) Spinal fusion procedures in the adult and young population: a systematic review on allogenic bone and synthetic grafts when compared to autologous bone. J Mater Sci Mater Med 31(6):51. https://doi.org/10.1007/s10856-020-06389-3
Simon D, Kumar KA, Sivadasan SB, Varma H, Balan A (2020) Hydroxyapatite carriers as drug eluting agents—An In Vitro analysis. Indian J Dent Res 31(3):481
Nickoli MS, Hsu WK (2014) Ceramic-based bone grafts as a bone grafts extender for lumbar spine arthrodesis: a systematic review. Global Spine J 4(3):211–6. https://doi.org/10.1055/s-0034-1378141
Plantz MA, Gerlach EB, Hsu WK (2021) Synthetic bone graft materials in spine fusion: current evidence and future trends. Int J Spine Surg 15(1):104–112. https://doi.org/10.14444/8058
Unnikrishnan V, Venugopal A, Sivadasan SB, Boniface Fernandez F, Arumugam S, PR HV, et al (2022) Cellular and sub-chronic toxicity of hydroxyapatite porous beads loaded with antibiotic in rabbits, indented for chronic osteomyelitis. Int J Pharm. 616:121535. https://doi.org/10.1016/j.ijpharm.2022.121535
Author information
Authors and Affiliations
Contributions
MB, VKM and HV conceptualised the study; MB and VKM wrote the main text; MB, VKM and UK analysed and interpreted the data; UK, SR and AM prepared the figures; MB and VKM approved the version to be published.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of Declaration of Helsinki. Approval was granted by the Ethics Committee of University vide letter No: BVDUMC/IEC/130.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Borde, M.D., Menon, V.K., Kanade, U.P. et al. Drug eluting bioactive glass ceramics for fusion in spondylodiscitis: a pilot study. Neurosurg Rev 47, 80 (2024). https://doi.org/10.1007/s10143-024-02317-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-024-02317-z