Abstract
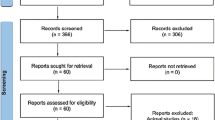
Over the last decades, minimally invasive techniques have revolutionized the endovascular treatment (EVT) of brain aneurysms. In parallel, the development of conscious sedation (CS), a potentially less harmful anesthetic protocol than general anesthesia (GA), has led to the course optimization of surgeries, patient outcomes, and healthcare costs. Nevertheless, the feasibility and safety of EVT of brain aneurysms under CS have yet to be assessed thoroughly. Herein, we systematically reviewed the medical literature about this procedure. In accordance with the PRISMA guidelines, four databases (PubMed, EMBASE, SCOPUS, and Cochrane Library) were queried to identify articles describing the EVT of brain aneurysms under CS. Successful procedural completion, complete aneurysm occlusion outcomes, intraoperative complications, clinical outcomes, and mortality rates assessed the feasibility and safety. Our search strategy yielded 567 records, of which 11 articles were included in the qualitative synthesis. These studies entailed a total of 1142 patients (40.7% females), 1183 intracranial aneurysms (78.4% in the anterior circulation and 60.9% unruptured at presentation), and 1391 endovascular procedures (91.9% performed under CS). EVT modalities under CS included coiling alone (63.2%), flow diversion (17.7%), stent-assisted coiling (10.6%), stenting alone (6.5%), onyx embolization alone (1.7%), onyx + stenting (0.2%), and onyx + coiling (0.2%). CS was achieved by combining two or more anesthetics, such as midazolam, fentanyl, and remifentanil. Selection criteria for CS were heterogenous and included patients’ history of pulmonary and cardiovascular diseases, outweighing the benefits of CS versus GA, a Hunt and Hess score of I–II, a median score of 3 in the American Society of Anesthesiology scale, and patient’s compliance with elective CS. Procedures were deemed successful or achieving complete aneurysm occlusion in 88.1% and 9.4% of reported cases, respectively. Good clinical outcomes were described in 90.4% of patients with available data at follow-up (mean time: 10.7 months). The procedural complication rate was 16%, and the mortality rate was 2.8%. No complications or mortality were explicitly attributed to CS. On the other hand, procedure abortion and conversion from CS to GA were deemed necessary in 5% and 1% of cases, respectively. The present study highlights the feasibility of performing EVT of brain aneurysms under CS as an alternative anesthetic protocol to GA. However, the limited nature of observational studies, methodological quality, the predominant absence of a comparative GA group, and clinical data during follow-up restrict a conclusive statement about the safety of EVT under CS. Accordingly, further research endeavors are warranted toward a higher level of evidence that can be translated into surgical practice.

Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References
Connolly ES, Rabinstein AA, Carhuapoma JR et al (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke 43(6):1711–1737. https://doi.org/10.1161/STR.0b013e3182587839
Thompson B, Brown R, Amin-Hanjani S et al (2015) Guidelines for the management of patients with unruptured intracranial aneurysms: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke (1970) 46(8):2368–2400. https://doi.org/10.1161/STR.0000000000000070
Dumont TM, Eller JL, Mokin M, Sorkin GC, Levy EI (2014) Advances in endovascular approaches to cerebral aneurysms. Neurosurgery 74(Suppl 1):17. https://doi.org/10.1227/NEU.0000000000000217
Riina HA, Eskridge J, Berenstein A (1998) Future endovascular management of cerebral aneurysms. Neurosurg Clin N Am 9(4):917–921
Waqas M, Monteiro A, Cappuzzo JM, Tutino VM, Levy EI (2022) Evolution of the patient-first approach: a dual-trained, single-neurosurgeon experience with 2002 consecutive intracranial aneurysm treatments. J Neurosurg 137(6):1751–1757. https://doi.org/10.3171/2022.2.JNS22105
Practice guidelines for sedation and analgesia by non-anesthesiologists: an updated report by the American Society of Anesthesiologists Task Force on Sedation and Analgesia by non-Anesthesiologists. Anesthesiology (Philadelphia). 2002;96(4):1004–1017. https://doi.org/10.1097/00000542-200204000-00031
Esmaeeli S, Valencia J, Buhl LK et al (2021) Anesthetic management of unruptured intracranial aneurysms: a qualitative systematic review. Neurosurg Rev 44(5):2477–2492. https://doi.org/10.1007/s10143-020-01441-w
Brinjikji W, Murad MH, Rabinstein AA, Cloft HJ, Lanzino G, Kallmes DF (2015) Conscious sedation versus general anesthesia during endovascular acute ischemic stroke treatment: a systematic review and meta-analysis. AJNR Am J Neuroradiol 36(3):525–529. https://doi.org/10.3174/ajnr.A4159
Rangel-Castilla L, Cress M, Munich S et al (2015) Feasibility, safety, and periprocedural complications of pipeline embolization for intracranial aneurysm treatment under conscious sedation: University at Buffalo neurosurgery experience. Neurosurgery. 11(Suppl 3(3)):426–430. https://doi.org/10.1227/NEU.0000000000000864
Murad MH, Sultan S, Haffar S, Bazerbachi F (2018) Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med 23(2):60–63. https://doi.org/10.1136/bmjebm-2017-110853
Wells GA, Shea B, O'Connell D et al The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 1 Dec 2022
Tso MK, Dossani RH, Waqas M, Rajah GB, Vakharia K, Siddiqui AH (2021) Coil occlusion of right M2 fusiform aneurysm after balloon-test occlusion: 2-dimensional video. World Neurosurgery 146:45. https://doi.org/10.1016/j.wneu.2020.10.129
Bhogal P, Chan N, Makalanda H, Wong K, Noblet J (2020) Transradial Woven EndoBridge device to treat a ruptured basilar tip aneurysm under conscious sedation. Interv Neuroradiol 26(6):779–784. https://doi.org/10.1177/1591019920927243
Sorenson TJ, Lanzino G, Rangel Castilla L (2019) Novel endovascular neck reconstruction and coiling technique for the treatment of a large wide-necked basilar apex aneurysm through a radial artery approach: 2-dimensional operative video. Oper Neurosurg (Hagerstown, Md.) 17(4):E157. https://doi.org/10.1093/ons/opz025
Song J, Lee C, Kim H (2018) Feasibility, safety, and periprocedural complications associated with endovascular treatment of ruptured intracranial aneurysms according to the depth of anesthesia. Am J Neuroradiol AJNR 39(9):1676–1681. https://doi.org/10.3174/ajnr.A5753
Griessenauer CJ, Shallwani H, Adeeb N et al (2017) Conscious sedation versus general anesthesia for the treatment of cerebral aneurysms with flow diversion: a matched cohort study. World Neurosurg. 102:1–5. https://doi.org/10.1016/j.wneu.2017.02.111
Ramaswamy R, Villwock MR, Shaw PM, Swarnkar A, Deshaies EM, Padalino DJ (2015) Open direct carotid artery access for coiling of an intracranial aneurysm under conscious sedation. Interv Neuroradiol 21(3):387–389. https://doi.org/10.1177/1591019915583220
Rahme R, Grande A, Jimenez L, Abruzzo TA, Ringer AJ (2014) Onyx HD-500 embolization of intracranial aneurysms: modified technique using continuous balloon inflation under conscious sedation. J Clin Neurosci 21(8):1383–1387. https://doi.org/10.1016/j.jocn.2014.01.004
Kan P, Jahshan S, Yashar P et al (2013) Feasibility, safety, and periprocedural complications associated with endovascular treatment of selected ruptured aneurysms under conscious sedation and local anesthesia. Neurosurgery 72(2):216–220. https://doi.org/10.1227/NEU.0b013e31827b9183
Ogilvy CS, Yang X, Jamil OA et al (2011) Neurointerventional procedures for unruptured intracranial aneurysms under procedural sedation and local anesthesia: a large-volume, single-center experience. J Neurosurg 114(1):120–128. https://doi.org/10.3171/2010.3.JNS091384
Qureshi AI, Suri MFK, Khan J et al (2001) Endovascular treatment of intracranial aneurysms by using Guglielmi detachable coils in awake patients: safety and feasibility. J Neurosurg 94(6):880–885. https://doi.org/10.3171/jns.2001.94.6.0880
Lee CZ, Gelb AW (2014) Anesthesia management for endovascular treatment. Curr Opin Anaesthesiol 27(5):484–488. https://doi.org/10.1097/ACO.0000000000000103
McDonald JS, Brinjikji W, Rabinstein AA, Cloft HJ, Lanzino G, Kallmes DF (2015) Conscious sedation versus general anaesthesia during mechanical thrombectomy for stroke: a propensity score analysis. J Neurointerv Surg 7(11):789–794. https://doi.org/10.1136/neurintsurg-2014-011373
Vatner SF (1978) Effects of anesthesia on cardiovascular control mechanisms. Environ Health Perspect 26:193–206. https://doi.org/10.1289/ehp.7826193
Harris M, Chung F (2013) Complications of general anesthesia. Clin Plast Surg 40(4):503–513. https://doi.org/10.1016/j.cps.2013.07.001
Lone PA, Wani NA, Ain QU, Heer A, Devi R, Mahajan S (2021) Common postoperative complications after general anesthesia in oral and maxillofacial surgery. Natl J Maxillofac Surg 12(2):206–210. https://doi.org/10.4103/njms.NJMS_66_20
Wu L, Zhao H, Weng H, Ma D (2019) Lasting effects of general anesthetics on the brain in the young and elderly: “mixed picture” of neurotoxicity, neuroprotection and cognitive impairment. J Anesth 33(2):321–335. https://doi.org/10.1007/s00540-019-02623-7
Volovici V, Verploegh IS, Satoer D et al (2023) Outcomes associated with intracranial aneurysm treatments reported as safe, effective, or durable: a systematic review and meta-analysis. JAMA Netw Open 6(9):e2331798. https://doi.org/10.1001/jamanetworkopen.2023.31798
Author information
Authors and Affiliations
Contributions
Conception and design: J.E.B.B.
Acquisition and standarization of data: J.E.B.B., K.K., A.M.B, L.B.O., S.B.
Analysis and interpretation of data: J.E.B.B., K.K., A.M.B., N.B., S.B.
Manuscript writing, and revision: J.E.B.B., K.K., A.M.B., R.A., J.W., R.B, J.L.A.S.
Study supervision: J.L.A.S, R.B.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Part of this work was accepted as an abstract at the 2022 Annual Congress of Neurological Surgeons in San Francisco, California, United States of America.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bocanegra-Becerra, J.E., Kersting, K., Blega, A.M. et al. Endovascular treatment of brain aneurysms under conscious sedation: a systematic review of procedural feasibility and safety. Neurosurg Rev 47, 42 (2024). https://doi.org/10.1007/s10143-023-02272-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-02272-1