Abstract
This is a retrospective monocentric study. The aim of this study is to analyze the incidence of recurrent or junctional lumbar foraminal herniated disc, in patients treated with trans pars microsurgical approach. Foraminal lumbar disc herniation represents a challenging pathology for the spinal surgeon. The appropriate surgical approach still represents a matter of debate. Several open and minimally-invasive techniques have been developed, in order to allow a proper tissue exposure and preserving the vertebral stability. The trans pars approach has already been described as a possible alternative, allowing excellent exposure of the herniated fragment with minimum bone removal. While few studies have analyzed the very low rate of post-operative instability, no articles deal with the incidence of post-operative herniated disc recurrence or junctional disc herniation in patients treated with this technique. We enrolled 160 patients operated at our institution. A univariate and multivariate analysis of possible factors influencing outcome (age, sex, level and BMI) was performed. Outcome variables were recurrent or junctional herniated disc. At the end, 135 patients were analyzed. Of the 135 patients, six presented recurrent herniated disc (4.4%) and other three developed a junctional herniation (2.2%). The occurrence of junctional herniated disc or recurrent herniated disc was not influenced by the analyzed variables, both at univariate and at multivariate analyses. The trans pars approach presents a low rate of recurrence and junctional herniation. Age, sex, level, and BMI do not influence the recurrence rate, both at same level and at junctional level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lumbar disc herniation (LDH)-related back pain still represents the most common pathological condition that the spine surgeon faces in his or her clinical practice [1,2,3], and among them, lumbar foraminal disc herniations (FLDH) are undoubtedly the case that results in the most severe pain for the patient and the greatest likelihood of neurological deficits [4]. Over time, several surgical approaches have been proposed for their treatment most of which involve massive bony removal so as to achieve wider exposure at the expense, however, of potentially undermining the stability of the spine [5, 6].
In order to minimize vertebral instability, relatively new surgical techniques focused on obtaining maximum exposure with minimal bone removal have been proposed.
The trans pars interarticularis approach is one of them, and its main focus is at exposing the herniated fragment in the foramen of conjugation by partial removal of the vertebral isthmus alone without touching the joint in any way thus preserving the stability of the segment [7, 8].
This approach has been demonstrated to be safe and effective to treat FHLD [8].
However, evidences on possible recurrence of LDH or occurrence of a junctional LDH in patients with FLDH treated with the trans pars approach are limited.
A recent literature meta analysis [9] shows how the recurrence rate of nucleus pulpous herniation after discectomy is a wide common problem with rates ranging from 2 to 25% despite the surgical technique used in the absence of any work specifically analyzing the trans pars technique.
Similarly, at the present day, no recent studies in literature exist specifically dealing with junctional herniations after discectomies in general and with microscopic trans pars techniques in particular; the only existing studies are about adjacent segment pathology after lumbar arthrodesis [10,11,12].
The aim of this retrospective study is therefore to specifically analyze the rate of recurrent or junctional LDH after treating a FLHD with the microscopic trans pars approach and to show if patients’ characteristics such as age, sex, level, and BMI could influence this rate.
Surgical technique
The trans pars approach is a microsurgical technique with the aim to give access to the foraminal region of interest (in order to decompress the nerve root, to perform a discectomy, treat the herniated disc syndrome, and prevent the relapse) in a less destructive manner compared to other microsurgical options available but achieving the same result in terms of efficacy.
The patient is under general anesthesia, prone, or in the knee-chest position.
A paramedian incision of approximately 3 cm must be carried out about 1cm far from midline; a dissection of the subcutaneous tissue from the underlying fascia must be performed, and therefore, the fascia is cut in the whereabouts of the lateral aspect of the spinous process.
A subperiostal dissection of the multifidus muscle must be carried out; the surgeon must carry on the dissection laterally to expose the inferior facet joint and the pars interarticularis.
The pars interarticularis (as known as isthmus) from the surgical view lies right above the intervertebral foramen, from which the nervous root corresponding to the upper vertebra transits. A dissector is then placed in the angle between the superior aspect of the inferior facet joint and the lateral aspect of the pars interarticularis as a radiopaque marker. The removal of the lateral aspect of the isthmus must be carried out using a twist-drill; also, a small part of the superior aspect of the inferior facet joint can be removed; the removal of the medial portion of the pars interarticularis is completed using Kerrison rongeurs. The surgeon has now visual on the lateral portion of the ligamentum flavum, which can be cut and removed.
As a result, the intraforaminal structures are now exposed: the nerve root lies usually cranially, while the disc space can usually be seen in the caudal part of the surgical window. Once the herniated disc into the foramen is identified, it must be gently and safely isolated from the nerve root then removed. Finally, a complete hemostasis of the site must be obtained and the fascia, the subcutaneous tissue, and the skin are closed in layers.
Materials and methods
This is a retrospective study enrolling patients suffering from foraminal herniated lumbar disc (FLDH) and treated with microsurgical trans pars approach.
Local ethical committee approved the present study (55/2019/Oss/AOUFe).
Patients
Demographic and pre- and postoperative clinical characteristics were recorded for all patients (age, sex, BMI), including pain assessment and nerve root palsy (length of symptomatic period, presence of motor deficit, and radicular pain before the operation) (Table 1).
Indication for surgery were persistent radicular pain after 4–6 weeks of unsuccessful conservative and medical treatment and/or presence of nerve root palsy. Contraindications to surgery were active cardiovascular disease (acute heart insufficiency, recent myocardial infarction, unstable coronary syndrome) and other contraindications to general anesthesia (i.e., pneumonia, and sepsis).
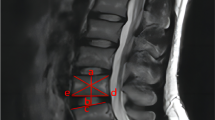
All patients underwent preoperative MRI and were evaluated for motor recovery and persistence of pain at regular intervals until the third year after discharge. In the event that the patient reported persistence of pain with the same characteristics as preoperatively or the onset of new low back pain with sciatalgic radiations, a new MRI was recommended in order to highlight recurrence and/or the onset of junctional herniation.
Statistical analysis
The statistical analyses were carried out using the Statistical Package for the Social Sciences, a software package for Windows (version 11.0.1; SPSS, Inc.) (Microsoft Corporation, One Microsoft Way Redmond, WA 98052-7329, USA).
Univariate analysis (Fisher exact test) included impact of age (range 25–86 years), sex, level (range L2/L3 to L5/S1), and BMI (range 18–38.5 kg/m [2] median value = 26.8 kg/m [2] ) on outcome variables, i.e., evidence of junctional herniated disc at follow-up and evidence of recurrence of herniated disc at follow-up. Logistic regression analysis was used for defining the impact of the aforementioned variables on outcome variables. Results presenting p ≤ 0.05 were considered statistically significant.
Results
Demographic characteristics
We enrolled at the beginning 160 patients with purely foraminal herniated disc operated using trans pars microscopic approach at Ferrara University Hospital between January 2015 and January 2020; 25 were lost during the follow-up in the period between the surgery and the outpatient visit. Therefore, we collected a total of 135 patients, 94 males (69.6%) and 41 females (30.4%), with the age range of 25–86 years old and the median age of 61.3 years old.
In 132 out of 135 (97.8%) the BMI was available with a range of 18.0–38.5 kg/m [2] and the median BMI was 26.8 kg/m [2].
Clinical characteristics
The locations of the LDHs were as follows: 17 patients presented L2-L3 FLDH (12.87%), 39 L3-L4 FLDH (29.54%), 62 L4-L5 FLDH (46.96%), 16 L5-S1 FLDH (12.12%), and 1 had a FLDH at both L3-L4 and L4-L5 level (0.75%). The right side was the most involved (78 patients – 59.01%), while the left side was affected in 57 cases (43.18%), even though one patient had bilateral involvement (0.75%).
Before surgery, 38 patients had symptoms for 1 month or less (28.03%), while 97 had symptoms for more than 1 month (74.24%); median length of symptomatic period was 4.2 months, while the range was 1 week to 94 months. Before surgery, all of 135 patients had radicular pain (100%) and 91 (67.04%) patients presented with a motor deficit: 33 patients had foot dorsiflexion deficit (36.2%), 3 plantar-flexion (3.3%), 54 presented deficit of the thigh strength (59.3%), one had a deficit of the adduction of the thigh (0.76%), and 7 of hip flexion (7.7%). Seven patients had more than one motor deficit.
Outcomes
There were no major complications (CSF leak or hemorrhage) during or immediately following surgery.
Blood losses were minimal, no patients needed to be transfused after these surgeries; hospitalization times were minimal too with about 24 h on average of hospital stay with mobilization on the first post op day.
Among 135 patients, 6 experienced recurrence at the same level treated (4.4%): 1 patient presented L3/L4 recurrence after 2 weeks of follow-up treated with left laminectomy; 1 patient had right L3/L4 recurrence after 4 months of follow-up and not retreated because of patient’s choice; 1 patient had left L4/L5 recurrence after 18 months retreated with microscopic trans pars approach; one had a recurrence after 5 months; another one after 7 months both re-treated successfully with trans pars approach; and one patient presented contralateral foraminal LDH after 20 months and was successfully treated surgically.
Among 135 patients, 3 had junctional herniation after surgery (2.2%). One of them had two FLDH at L3-L4 and L4-L5 levels and experienced a junctional asymptomatic herniation at L2-L3 level 33 months after surgery objectively demonstrated with an MRI. One patient treated for L4-L5 FLDH presented a symptomatic L3-L4 junctional herniation 30 months after surgery, which was treated successfully with two peri-radicular steroid injections. One patient treated for L3-L4 FLDH presented a junctional L4-L5 herniation 10 months after surgery, demonstrated through MRI and successfully treated with peri-radicular steroid injections.
Among 91 patient that experienced radicular deficit before surgery, 70 patients referred total recovery in daily activities (75.8%), 18 patients referred partial recovery in daily activities (19.8%), and 3 patients referred no recovery in daily activities (3.3%).
All patients (100%) had radicular pain preoperatively (mean NRS 8, range 6–10, Table 1). After surgery, 96 patients referred no pain (71.1%), 14 patients referred low back pain without sciatica (10.4%), 23 referred diminished but residual radicular pain (17 %), and 2 patients (1.5% of the total) referred that the pain had not changed.
The results of the statistical analysis performed showed that the occurrence of junctional herniated disc or recurrent herniated disc were not influenced by the analyzed variables, both at univariate and at multivariate analyses (Tables 2 and 3).
Discussion
At the authors’ best knowledge, this is the first study specifically analyzing the rate of recurrences at the same level or at a junctional level in patients with FLHD treated by the microsurgical trans pars approach.
Despite the extensive debate in literature as to what is the best approach in the surgical treatment of these conditions and despite its detractors claiming that the trans isthmus technique is burdened by a higher number of recurrences due to the narrow surgical corridor that would not allow optimal control toward the medial side of the herniation, our results show that out of 135 cases analyzed, 6 recurrences occurred at the same level (4,4%) and only 5 of them were retreated with surgery.
Moreover, the rate of junctional herniation after surgery was also low; only 3 cases out of 135 were detected (2.2%) and none of these cases required surgery.
In order to compare our results, we performed a brief literature review in which it emerges, as said before, that nowadays there are no available published studies specifically analyzing recurrence and/or junctional disc herniation rate after this kind of surgery.
The only pertinent results were obtained combining on Pubmed search the terms “foraminal disc herniation AND recurrence” and “foraminal disc herniation OR recurrence”, including studies which analyzed the rate of hernial recurrence after surgery also with far lateral techniques and excluding items of instrumented surgery; papers in which endoscopic techniques were used and articles in other languages than English (see Table 4).
Porchet [8] et al. published in 1999 results about 202 patients operated with far lateral technique (187 trans muscular, 15 para muscular). Only 9 out of 202 developed recurrence at the same level (4 reoperated with far lateral technique, 5 with standard interlaminar technique given paramedian recurrence) with a calculated recurrence rate of 4.45 %.
Kotil et al in 2007 [13] published a paper analyzing 14 patients with foraminal/extra foraminal L5/S1 disc herniations treated with trans-muscular technique in which they reported no postoperative recurrence.
In 2018, resuming a technique already proposed in 2003 by Greiner-Perth [14], Abdelgawaad and colleagues [15] performed 76 surgeries with microscopic assisted percutaneous nucleotomy technique for foraminal and extraforaminal lumbar disc herniations obtaining recurrences in only two treated cases (2.63 % of recurrence rate).
A more recent modification of the technique proposed by Abdelgaawad was developed in 2021 by Alhashash. According to this modification, 50 patients with herniated foraminal discs were treated obtaining only 2 recurrences (4%) [16].
A Japanese 2021 study proposed an alternative technique for the treatment of lumbar foraminal pathologies involving hemilaminectomy with laminoplasty, however, this technique was only used in 4 patients with extraforaminal disc herniations and in 44 patients with lumbar herniations not specifying how many of these were foraminal and how many were paramedian. The recurrence rate was settled at 6.25 % (3 recurrent disc hernias out of 48 treated) and in all cases that required re operation a TLIF (transforaminal lumbar inter body fusion) was performed [16].
Except for Porchet’s work in which 2 junctional recurrences are reported and Tanaka’s work in which 1 junctional LDH is reported; no junctional recurrences are detected in the other cited works.
Few years ago De Bonis et al. proposed a different, more conservative approach for the minimally invasive treatment of FLDH that would allow access to the foramen of conjugation only with minimal bony removal at the level of the isthmus: the trans pars interarticularis microscopic approach [17].
Although this approach is not entirely new, it has long been criticized both because of its learning curve and because, in the eyes of its detractors, for the possible difficulty to manage any hernias that extend even medially, potentially thereby promoting the rate of recurrence in the absence, however, of specific literature on the subject.
Results of the present study is intended as a natural complement to the previous published in 2017 adding an analysis of 135 consecutive cases operated with this technique in terms of recurrence rate and the onset of junctional herniations.
Our results show the trans pars approach is comparable to other approaches reported in the current literature (reported by Porchet, Abdelgawaad, and Alhashash, sightly minor comparing it with the Tanaka’s work) in terms of recurrence rate (4.4%) and junctional herniation rate (2.2%).
The trans pars technique is less invasive in terms of muscular damage than, for example, the far lateral trans muscular techniques, using a smaller skin incision, that is comparable to that used for the medial herniectomies (3 cm on average).
It was not in the aim of this paper the analysis of post op instability; we have already published a paper that specifically addressed that issue (De Bonis et al. Spine 2017) [17]. In this series, we did not perform a radiological follow-up, but in patients that clinically presented post-op problems (recurrence of HD, junctional HD, persistent pain). All these patients (39 out of 135 cases) performed MRI and dynamic X-rays, showing no signs of instability and that is because the trans pars technique, as seen, only requires the removal of a very small portion of bone at the histmus level, without touching the articular complex in any way.
All of the above considerations also greatly affect the extremely short surgical times (the average duration of the surgery is about 70 min) as well as a shorter postoperative hospitalization and an earlier return to activities of daily living.
Lastly, the results obtained from statistical analyses show no significant correlations between the rate of LDH recurrence (whether junctional or at the same level) neither with the patient's age nor, more importantly, with BMI.
The latter finding about the non-correlation between BMI and recurrence rate is interesting and in contrast not only with the common thinking, that would like to see a higher probability of recurrences with higher values, but also with some studies published recently in literature although different surgical techniques were used.
As example, Siccoli et al. in 2022 [18] found this correlation statistically significant (p = 0.017), the same has done by Wang et al. in 2022 [19] that found a significant correlation both with BMI and patient age (BMI p = 0.001, age p < 0.001) while Li et al. [20] showed that only a BMI above 25 is somehow related to an increased risk of recurrence considering a wide population sample but operated with percutaneous endoscopic technique.
Several authors have published their series of patients with foraminal lumbar herniation operated either with the endoscope or with the microscope.
No series directly compare these two approaches. Nonetheless, outcome variables in terms of pain control seem to be similar [17, 21,22,23].
The population sample analyzed in our study is undoubtedly smaller compared to that reported in previously cited papers but, to date, it appears to be the largest treated with the trans pars microscopic technique so this data, while not reaching statistical significance, are nonetheless important and worthy of future investigation perhaps by enlarging the sample.
Correlations between age and outcome, sex and outcome, and age/sex/ BMI/treated level were also not significant in these analyses (Table 2).
Conclusion
Trans pars microscopic approach for the treatment of FLDH is effective and safe. Recurrence rate in our series is consistently low and in line with the current literature, as well as the onset of junctional LDH rate. Age, sex, BMI, and level of the herniated disc do not influence the rate of recurrences both at same level and at junctional level.
Data availability
The data in this study are shown in Table 1; further information about the statistics is accessible upon request to the authors.
Change history
19 September 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10143-023-02158-2
References
Schroeder GD, Guyre CA, Vaccaro AR (2016) The epidemiology and pathophysiology of lumbar disc herniation. Seminars in Spine Surgery 28(1):2–7. https://doi.org/10.1053/j.semss.2015.08.003
Asch HL, Lewis PJ, Moreland DB et al (2002) Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? J Neurosurg 96:34
Koebbe CJ, Maroon JC, Abla A et al (2002) Lumbar microdiscectomy: a historical perspective and current technical considerations. Neurosurg Focus 13:E3
Epstein N (2002) Foraminal and far lateral lumbar disc herniations: surgical alternatives and outcome measures. Spinal Cord 40:491–500. https://doi.org/10.1038/sj.sc.3101319
Lofrese G, Mongardi L, De Bonis P, Trapella G et al (2017) Surgical treatment of intraforaminal/extraforaminal lumbar disc herniations: Many approaches for few surgical routes. Acta Neurochir (Wien) 159(7):1273–1281
Bernucci et al. Translaminar microsurgical approach for lumbar herniated nucleus pulposus in the Hidden zone. Spine 32,2,281-284, 2007.
Di Lorenzo N, Porta F, Onnis G et al (1998) Pars interarticularis fenestration in the treatment of foraminal lumbar disc herniation: a further surgical approach. Neurosurgery 42:87
Porchet F, Chollet-Bornand A, De Tribolet N (1999) Long-term follow up of patients surgically treated by the far-lateral approach for foraminal and extraforaminal lumbar disc herniations. J Neurosurg 90:59–66
Shepard N, Cho W (2019) Recurrent lumbar disc herniation: a review. Global Spine Journal 9(2):202–209. https://doi.org/10.1177/2192568217745063)
Chiu JC, Clifford T, Princenthal R, Shaw S (2005) Junctional disc herniation syndrome in post spinal fusion treated with endoscopic spine surgery. Surg Technol Int 14:305–315
Landi A, Grasso G, Mancarella C, Dugoni DE, Gregori F, Iacopino G, Bai HX, Marotta N, Iaquinandi A, Delfini R (2018) Recurrent lumbar disc herniation: Is there a correlation with the surgical technique? A multivariate analysis. J Craniovertebr Junction Spine 9(4):260–266. https://doi.org/10.4103/jcvjs.JCVJS_94_18
Ahsan K, Khan SI, Zaman N, Ahmed N, Montemurro N, Chaurasia B (2021) Fusion versus nonfusion treatment for recurrent lumbar disc herniation. J Craniovertebr Junction Spine 12(1):44–53. https://doi.org/10.4103/jcvjs.JCVJS_153_20
Kotil K, Akcetin M, Bilge T (2007) A minimally invasive transmuscular approach to far-lateral L5-S1 level disc herniations: a prospective study. J Spinal Disord Tech 20(2):132–138. https://doi.org/10.1097/01.bsd.0000211268.43744.2a
Greiner-Perth R, Böhm H, Allam Y (2003) A new technique for the treatment of lumbar far lateral disc herniation: technical note and preliminary results. Eur Spine J 12:320–324
Alhashash M, Gendy H, Shousha M (2022) Extra-laminar microscopic-assisted percutaneous nucleotomy (EL-MAPN) for the treatment of foraminal lumbar disc prolapse, a modified minimally invasive approach. Arch Orthop Trauma Surg 142(10):2405–2411. https://doi.org/10.1007/s00402-021-03846-8
Tanaka M, Kanayama M, Hashimoto T, Oha F et al (2021) Clinical outcomes and postoperative radiographic assessment of osteoplastic hemilaminectomy in the treatment of lumbar foraminal nerve root compression. Spine Surg Relat Res 5(6):352–358. https://doi.org/10.22603/ssrr.2020-0203
De Bonis P, Mongardi L, Cavallo M. A et al. (2017) Transpars microscopic approach for the treatment of purely foraminal herniated lumbar disc. A Clinical, Radiological, Two-center Study. Spine 42(6):E371–E378. https://doi.org/10.1097/BRS.0000000000001839
Siccoli A, Staartjes VE, Klukowska AM, Muizelaar JP, Schröder ML (2022) Overweight and smoking promote recurrent lumbar disk herniation after discectomy. Eur Spine J 31(3):604–613. https://doi.org/10.1007/s00586-022-07116-y
Wang F, Chen K, Lin Q et al (2022) Earlier or heavier spinal loading is more likely to lead to recurrent lumbar disc herniation after percutaneous endoscopic lumbar discectomy. J Orthop Surg Res 17:356. https://doi.org/10.1186/s13018-022-03242-x)
Li H, Deng W, Wei F, Zhang L, Chen F (2023) Factors related to the postoperative recurrence of lumbar disc herniation treated by percutaneous transforaminal endoscopy: a meta-analysis. Front. Surg 9:1049779. https://doi.org/10.3389/fsurg.2022.1049779
Greil ME, Ogunlade JI, Bergquist J et al (2023) Full-endoscopic trans-pars interarticularis approach for far lateral lumbar discectomy. Eur Spine J 32:2709–2716. https://doi.org/10.1007/s00586-023-07698-1
Oertel JM, Burkhardt BW (2017) Endoscopic intralaminar approach for the treatment of lumbar disc herniation.Oertel JM, Burkhardt BW. World Neurosurg 103:410–418. https://doi.org/10.1016/j.wneu.2017.03.132
Oertel JM, Burkhardt BW (2023) Microendoscopic surgery for degenerative disorders of the cervical and lumbar spine: the influence of the tubular workspace on instrument angulation, clinical outcome, complications, and reoperation rates. J Pers Med. 13(6):912. https://doi.org/10.3390/jpm13060912
Funding
Open access funding provided by Università degli Studi di Ferrara within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
M.M and C.A.E.G wrote the manuscript and prepared tables. A.S, M.A.C, and P.D.B reviewed the paper. M.M and P.D.B designed the work. P.D.B coordinated the research team
Corresponding author
Ethics declarations
Ethics approval
Local ethical committee approved the present study (55/2019/Oss/AOUFe).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The authors regret that the author names that appears in the original article were incorrect. The first and last names were swapped.
The original article has been corrected.
Supplementary information
(MP4 294 MB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Monticelli, M., Gelmi, C.A.E., Scerrati, A. et al. Recurrent or junctional lumbar foraminal herniated disc in patients operated with trans pars microscopic approach. Neurosurg Rev 46, 211 (2023). https://doi.org/10.1007/s10143-023-02109-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-02109-x