Abstract
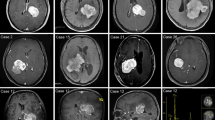
Giant lateral ventricular meningiomas (LVMs), with the largest diameter of at least 5 cm, form a distinct subset. The incidence of giant LVMs is considered to be relatively low. Here, we evaluated clinical characteristics, and clinical outcomes after microsurgical resection, especially functional outcomes and morbidity of giant LVMs. We retrospectively reviewed 49 patients with LVMs, including 18 giant LVMs from 2012 to 2020. And we analyzed clinical, histopathological, surgical, and outcome data at our institution. Giant LVMs were most commonly present in the fourth decade of patients with the male-to-female ratio of 1:2. The most common subtypes were transitional and fibrous. Most lesions were resected via the temporal or parieto-occipital approach in our series. The median volume of blood loss was higher in the giant group (900 vs. 600 ml, p = 0.02). Meanwhile, the median length of hospital stay was prolonged for giant LVMs (20.5 vs. 16.0 days, p < 0.01). The proportion of discharged functional deterioration was higher in giant LVMs (38.9% vs. 6.5%, p = 0.02). However, there was no statistical significance between functional deterioration and tumor size at long-term follow-up (p = 0.28). Giant LVMs patients suffered from neurological and regional complications more commonly, particularly from a postoperative hematoma (4/18 vs. 1/31), and hydrocephalus (2/18 vs. 0/31). Patients with giant LVMs had a high incidence of immediate functional deterioration after microsurgery, and there was no difference in functional deterioration between the giant and non-giant LVMS during long-term follow-up. Microsurgery entails a higher complication rate in giant LVMs. We need to pay special attention to preventing postoperative hematoma and hydrocephalus.


Similar content being viewed by others
References
Goldbrunner R, Stavrinou P, Jenkinson MD, Sahm F, Mawrin C, Weber DC et al (2021) EANO guideline on the diagnosis and management of meningiomas. Neuro Oncol. 23:1821–1834. https://doi.org/10.1093/neuonc/noab150
Ostrom QT, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS (2021) CBTRUS Statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2014-2018. Neuro Oncol. 23:iii1–iii105. https://doi.org/10.1093/neuonc/noab200
Pereira BJA, de Almeida AN, Paiva WS, de Aguiar PHP, Teixeira MJ, Marie SKN (2020) Natural history of intraventricular meningiomas: systematic review. Neurosurg Rev. 43:513–523. https://doi.org/10.1007/s10143-018-1019-0
Grujicic D, Cavallo LM, Somma T, Illic R, Milicevic M, Raicevic S et al (2017) Intraventricular meningiomas: a series of 42 patients at a single institution and literature review. World Neurosurg. 97:178–188. https://doi.org/10.1016/j.wneu.2016.09.068
Guidetti B, Delfini R, Gagliardi FM, Vagnozzi R (1985) Meningiomas of the lateral ventricles. Clinical, neuroradiologic, and surgical considerations in 19 cases. Surg Neurol. 24:364–370. https://doi.org/10.1016/0090-3019(85)90292-7
Haeren RHL, Rautalin I, Schwartz C, Korja M, Niemela M (2021) Surgery on giant meningiomas in very old patients entails frequent postoperative intracranial hemorrhages and atypical histopathology. J Neurooncol. 152:195–204. https://doi.org/10.1007/s11060-020-03693-4
Narayan V, Bir SC, Mohammed N, Savardekar AR, Patra DP, Nanda A (2018) Surgical management of giant intracranial meningioma: operative nuances, challenges, and outcome. World Neurosurg. 110:e32–e41. https://doi.org/10.1016/j.wneu.2017.09.184
Schwartz C, Jahromi BR, Lonnrot K, Hafez A, Maekawa H, Lehecka M et al (2021) Clinical outcome after microsurgical resection of intraventricular trigone meningiomas: a single-centre analysis of 20 years and literature overview. Acta Neurochir (Wien). 163:677–687. https://doi.org/10.1007/s00701-020-04520-5
Nanda A, Bir SC, Maiti T, Konar S (2016) Intraventricular meningioma: technical nuances in surgical management. World Neurosurg. 88:526–537. https://doi.org/10.1016/j.wneu.2015.10.071
Wang X, Cai BW, You C, He M (2007) Microsurgical management of lateral ventricular meningiomas: a report of 51 cases. Minim Invasive Neurosurg. 50:346–349. https://doi.org/10.1055/s-2007-993205
Delfini R, Acqui M, Oppido PA, Capone R, Santoro A, Ferrante L (1991) Tumors of the lateral ventricles. Neurosurg Rev. 14:127–133. https://doi.org/10.1007/bf00313037
Menon G, Nair S, Sudhir J, Rao R, Easwer HV, Krishnakumar K (2009) Meningiomas of the lateral ventricle - a report of 15 cases. Br J Neurosurg. 23:297–303. https://doi.org/10.1080/02688690902721862
Ma J, Cheng L, Wang G, Lin S (2014) Surgical management of meningioma of the trigone area of the lateral ventricle. World Neurosurg. 82:757–769. https://doi.org/10.1016/j.wneu.2014.05.026
Li Z, Li H, Jiao Y, Ma J, Wang S, Cao Y et al (2018) Clinical features and long-term outcomes of pediatric intraventricular meningiomas: data from a single neurosurgical center. Neurosurg Rev. 41:525–530. https://doi.org/10.1007/s10143-017-0884-2
Samanci Y, Oktug D, Yilmaz M, Sengoz M, Peker S (2020) Efficacy of gamma knife radiosurgery in the treatment of intraventricular meningiomas. J Clin Neurosci. 80:38–42. https://doi.org/10.1016/j.jocn.2020.08.016
Jiang Y, Lv L, Li J, Ma W, Chen C, Zhou P et al (2020) Clinical features, radiological findings, and treatment outcomes of high-grade lateral ventricular meningiomas: a report of 26 cases. Neurosurg Rev. 43:565–573. https://doi.org/10.1007/s10143-019-01078-4
Maiuri F, Mariniello G, Barbato M, Corvino S, Guadagno E, Chiariotti L et al (2021) Malignant intraventricular meningioma: literature review and case report. Neurosurg Rev. https://doi.org/10.1007/s10143-021-01585-3
Lyngdoh BT, Giri PJ, Behari S, Banerji D, Chhabra DK, Jain VK (2007) Intraventricular meningiomas: a surgical challenge. J Clin Neurosci. 14:442–448. https://doi.org/10.1016/j.jocn.2006.01.005
Fornari M, Savoiardo M, Morello G, Solero CL (1981) Meningiomas of the lateral ventricles. Neuroradiological and surgical considerations in 18 cases. J Neurosurg 54:64–74. https://doi.org/10.3171/jns.1981.54.1.0064
Nakamura M, Roser F, Bundschuh O, Vorkapic P, Samii M (2003) Intraventricular meningiomas: a review of 16 cases with reference to the literature. Surgical Neurology. 59:490–503. https://doi.org/10.1016/s0090-3019(03)00082-x
Jamshidi AO, Beer-Furlan A, Hardesty DA, Ditzel Filho LFS, Prevedello LM, Prevedello DM (2021) Management of large intraventricular meningiomas with minimally invasive port technique: a three-case series. Neurosurg Rev. 44:2369–2377. https://doi.org/10.1007/s10143-020-01409-w
Yu SQ, Wang JS, Chen SY, Liu XM, Li Y, Ding YM et al (2015) Diagnostic significance of intraoperative ultrasound contrast in evaluating the resection degree of brain glioma by transmission electron microscopic examination. Chin Med J (Engl) 128:186–190. https://doi.org/10.4103/0366-6999.149194
Lekht I, Brauner N, Bakhsheshian J, Chang KE, Gulati M, Shiroishi MS et al (2016) Versatile utilization of real-time intraoperative contrast-enhanced ultrasound in cranial neurosurgery: technical note and retrospective case series. Neurosurg Focus. 40:E6. https://doi.org/10.3171/2015.11.FOCUS15570
Goel A, Vutha R, Shah A, Singh K, Goel N, Shenoy A et al (2021) Large lateral intraventricular tumors - outcome of radical surgery. J Clin Neurosci. 88:205–212. https://doi.org/10.1016/j.jocn.2021.03.040
Dobran M, Marini A, Nasi D, Liverotti V, Benigni R, Iacoangeli M et al (2018) Surgical treatment and outcome in patients over 80 years old with intracranial meningioma. Clin Neurol Neurosurg. 167:173–176. https://doi.org/10.1016/j.clineuro.2018.02.024
Fornari M, Savoiardo M, Morello G, Solero CL (1981) Meningiomas of the lateral ventricles. Neuroradiological and surgical considerations in 18 cases. J Neurosurg. 54:64–74. https://doi.org/10.3171/jns.1981.54.1.0064
de Almeida AN, Pereira BJA, Pires Aguiar PH, Paiva WS, Cabrera HN, da Silva CC et al (2017) Clinical outcome, tumor recurrence, and causes of death: a long-term follow-up of surgically treated meningiomas. World Neurosurg. 102:139–143. https://doi.org/10.1016/j.wneu.2017.03.009
Tyagi G, Bhat DI, Devi BI, Shukla D (2019) Multiple Remote sequential supratentorial epidural hematomas-an unusual and rare complication after posterior fossa surgery. World Neurosurg. 128:83–90. https://doi.org/10.1016/j.wneu.2019.04.228
Lin Z, Wang C, Gao Z, Li X, Lan F, Liu T et al (2019) Clinical characteristics of and treatment protocol for trapped temporal horn following resection of lateral ventricular trigone meningioma: a single-center experience. J Neurosurg. 132:481–490. https://doi.org/10.3171/2018.11.jns182710
Lin Z, Zhang X, Shen S, Gao Z, Guan C, Liu T et al (2020) Postoperative delayed trapped temporal horn in patients with lateral ventricular trigone meningioma: risk factors, surgical management, and literature review. Eur J Surg Oncol. 46:2324–2330. https://doi.org/10.1016/j.ejso.2020.04.033
Wang Y, Lin Z, Li Z, Zhao M, Hu M, Zhang H et al (2016) The incidence and risk factors of postoperative entrapped temporal horn in trigone meningiomas. World Neurosurg. 90:511–517. https://doi.org/10.1016/j.wneu.2016.03.040
Data availability
Not applicable
Author information
Authors and Affiliations
Contributions
Dan Cao: conceptualization, methodology, writing—original draft. Yibo Ou and Xu Chen: writing—review and editing. Zhengqian Guo and Yong Chen: date curation, softwarea. Jian Chen: supervision
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study was performed under Institutional Review Board approval and did not require patient consent (file number:TJ-IRB20220327).
Human and animal ethics
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 2075 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cao, D., Ou, Y., Chen, X. et al. Clinical outcomes after microsurgical resection of giant lateral ventricular meningiomas. Neurosurg Rev 46, 33 (2023). https://doi.org/10.1007/s10143-022-01932-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-022-01932-y