Abstract
Lumbosacral instrumentation continues to be challenging due to complex biomechanical force distributions and poor sacral bone quality. Various techniques have therefore been established. The aim of this study was to investigate the outcome of patients treated with S2-alar-iliac (S2AI), S2-alar (S2A), and iliac (I) instrumentation as the most caudal level. Sixty patients underwent one of the 3 techniques between January 2012 and June 2017 (S2AI 18 patients, S2A 20 patients, I 22 patients). Mean age was 70.4 ± 8.5 years. Screw loosening (SL) and sacroiliac joint (SIJ) pain were evaluated during the course at 3-month and maximum follow-up (FU). All patients completed 3-month FU, the mean FU period was 2.5 ± 1.5 years (p = 0.38), and a median of 5 segments was operated on (p = 0.26), respectively. Bone mineral density (BMD), derived opportunistically from computed tomography (CT), did not significantly differ between the groups (p = 0.66), but cages were more frequently implanted in patients of the S2A group (p = 0.04). SL of sacral or iliac screws was more common in patients of the S2A and I groups compared with the S2AI group (S2AI 16.7%, S2A 55.0%, I 27.3% of patients; p = 0.03). SIJ pain was more often improved in the S2AI group not only after 3 months but also at maximum FU (S2AI 61.1%, S2A 25.0%, I 22.7% of patients showing improvement; p = 0.02). Even in shorter or mid-length lumbar or thoracolumbar constructs, S2AI might be considered superior to S2A and I instrumentation due to showing lower incidences of caudal SL and SIJ pain.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Instrumentation of the lumbosacral spine continues to be a challenging area in spine surgery, particularly due to complex local anatomy, unique biomechanical force distributions, and comparatively poor sacral bone quality. Various concepts for construct improvement have therefore been developed. However, there is a high rate of screw loosening (SL), instrumentation failure, pseudarthrosis, and sacroiliac joint (SIJ) pain (up to 83%) [1,2,3].
The Galveston technique and iliac screws were the first approaches trying to improve caudal instrumentation by extending the construct down to the pelvis [4, 5]. However, although iliac screws were proven to be superior to the Galveston technique in terms of construct strength, iliac screws were shown to cause pain due their prominence, ending in revision surgery in about 22% of cases [5, 6]. Moreover, instrumentation down to the sacrum puts a long cranial cantilever on the SIJ, not only reducing the durability of the construct but also causing a biomechanical overload and therefore severe pain of the SIJ, which was reported in a systematic review to occur in 37 ± 28.48% (range 6–75%) of patients [7].
The search for alternative techniques to this point ended in the description and clinical establishment of the S2-alar-iliac (S2AI) screw trajectory [8]. By crossing 3 cortical bone structures (sacral bone plus SIJ) and allowing for long screw pinching between the compact bone of the pelvis, while also allowing for small incisions due to diverging trajectories and in-line rod bending, this technique offers a variety of advantages over iliac screw placements [9]. Likewise, due to the rigid trans-SIJ trajectory, this technique inhibits any SIJ motion, in contrast to iliac screws and is therefore assumed to better avoid postoperative SIJ pain. On the other hand, some colleagues argue that this rigid SIJ fixation causes reduced but necessary motion inside the SIJ, thus potentially reducing the patients’ quality of life [10]. Moreover, the trajectory is more demanding, thus causing potentially more vascular complications inside the small pelvis or even requiring spinal navigation to ease the approach [11].
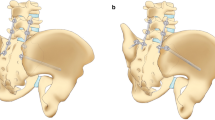
S2-alar-iliac technique. This slide shows the axial computed tomography (CT) slice of bilateral S2-alar-iliac (S2AI) screws. The entry point is between the dorsal S1 and S2 foramens. The screw then crosses the sacroiliac joint into the pelvis above the iliac notch via a trajectory targeting the head of the femur
We therefore hypothesize that instrumentations including S2AI screws are less prone to SL and SIJ pain compared with other established techniques. Thus, the aim of this study was to investigate differences in outcome between patients treated with S2AI, S2-alar (S2A), and iliac (I) instrumentation as the most caudal level.
Materials and methods
Study design
We reviewed all medical records and specifically checked the pre- and postoperative examinations including imaging studies, as well as postoperative follow-up (FU). The study enrolled 60 consecutive patients (35 male and 25 female) who underwent instrumentation by one of the 3 techniques between January 2012 and June 2017 as revision surgery after initial instrumentation (S2AI 18 patients [Fig. 1], 50% females, 72.1 ± 7.4 years; S2A 20 patients, 35% females, 69.8 ± 8.6 years; I 22 patients, 41% females, 69.5 ± 9.0 years). Outcome (SL and gluteal pain due to SIJ pain) was compared between the 3 groups considering preoperative, 3-month FU, and maximum FU examinations. Pain was routinely evaluated over the whole observation period during treatment and FU using a 10-point visual analogue scale.
Bone mineral density (BMD) was opportunistically assessed in preoperative imaging by computed tomography (CT) [12]. The 3 groups were comparable regarding the surgical approach and strategy of the treatment, especially in terms of the degree to which their deformities were corrected. The decision to perform one procedure versus another was based on the surgeons’ general preference. No patient criteria were taken into account in making this decision. SL was determined via CT images in all 3 planes by a conference of neurosurgeons and neuroradiologists.
Ethics
This study was approved by our local ethics committee (registration number: 159/16S) and was conducted in accordance with the Declaration of Helsinki. Informed consent was not required due to the retrospective character of the study and the conditions of our local ethics committee.
Statistics
All analyses were performed with the statistical software R (version 3.6.1; https://www.r-project.org/). p values < 0.05 were considered statistically significant.
General characteristics of the investigated cohort were presented stratified in 3 groups: S2AI, S2A, and I, depending on the surgical technique. Means and standard deviation (SD), median and ranges, or absolute or relative numbers were calculated. Depending on data distribution, analyses of variance (ANOVA), Kruskal-Wallis tests, or Chi-squared tests were used to assess differences in the analyzed parameters between the 3 groups.
The proportions and absolute numbers of patients with SIJ pain according to preoperative assessment, as well as at 3-month and maximum FU, were calculated stratified by group, respectively. Furthermore, proportions and absolute numbers of patients with improvement, deterioration, and unchanged status in SIJ pain at maximum FU compared with the preoperative status were calculated. Differences in these proportions between the 3 groups were assessed using Chi-squared or Fisher’s exact tests.
Potential predictors for improvement in SIJ pain were assessed, again stratified by group. Specifically, mean and SD, median and ranges, or absolute or relative numbers were calculated in patients with improvement and in patients with deterioration or unchanged status regarding SIJ pain. Associations with this status were tested using t tests, Mann-Whitney U tests, or Chi-squared tests. Improvement at maximum FU compared with the preoperative status was considered. The Benjamini-Hochberg procedure was used for correction of multiple testing regarding these prediction analyses, assuming a false discovery rate of 25%.
Results
General results and group differences
Participants’ mean age was 70.4 ± 8.5 years. The general demographics of all 3 groups are outlined in Table 1. Overall, the 3 groups were highly comparable and showed no statistically significant differences regarding baseline characteristics at the preoperative state. All patients received a 2-rod titanium construct.
All patients completed 3-month FU; maximum FU times were 2.3 ± 0.9 (S2AI), 3.0 ± 1.7 (S2A), and 2.4 ± 1.6 (I) years (p = 0.38). A median of 4.5 to 5 segments (S2AI, S2A) and 3 segments (I) was operated on (p = 0.26), extending to S2 or the os ilium, respectively. BMD as assessed opportunistically by CT did not significantly differ between the groups (p = 0.66). Cages were more frequently implanted in patients of the S2A group (p = 0.04).
Caudal screw loosening
SL of sacral or iliac screws was more common in patients of the S2A and I groups when compared with the S2AI group (S2AI 16.7%, S2A 55.0%, I 27.3% of patients; p = 0.03).
Improvement in sacroiliac joint pain
Gluteal pain as a clinical sign for SIJ pain was more often improved in the S2AI group not only after 3 months but also at maximum FU (S2AI 61.1%, S2A 25.0%, I 22.7% of patients showing improvement; p = 0.02; Table 2). While the S2A group already had a low rate of preoperative SIJ pain, the pain was comparable in the S2AI and I groups but significantly better in the S2AI group at 3-month and maximum FU. While 61.1% of patients in the S2AI group improved from their preoperatively existing SIJ pain, only 25.0% in the S2A and 18.2% in the I group improved at 3-month FU.
Specifically, predictors of SIJ pain at maximum FU were the number of fused segments and the number of screws per side from previous surgery among the S2AI group (Table 3), but these predictors did not survive correction for multiple comparisons. However, patients with SIJ pain at FU also required revision surgery significantly more often, in most cases due to and as a sign of SL.
Complications
There were no perioperative screw-related vascular or visceral surgical complications due to sacral or iliac screws; however, there was one screw-related aortic dissection due to an L2 screw in the I group. In the S2AI group, cerebrospinal fluid (CSF) leakage due to surgery was observed in 3 patients (16.7%), whereas hematoma occurred in 1 patient (5.6%). Furthermore, 3 patients (15.0%) of the S2A group showed CSF leakage, and 2 (10.0%) showed hematoma, whereas another 2 patients (10.0%) showed screw dislocation with cement leakage in 1 case. Among patients of the I group, 1 patient (4.5%) showed screw dislocation.
Regarding postoperative medical complications, urinary tract infection was most common (S2AI 4 patients, S2A 2 patients), followed by deep vein thrombosis (S2AI 2 patients, S2A 1 patient, I 2 patients), partially with related pulmonary artery embolism (S2AI 1 patient, I 2 patients). Two patients of the S2A group developed pneumonia, 1 patient of the S2AI group had a postoperative non-ST-elevation myocardial infarction, and 1 patient of the I group had postoperative endocarditis.
Discussion
Our main findings were that S2AI showed superiority compared with S2A and I techniques in terms of reduced caudal SL and a lower rate of SIJ pain. Additionally, none of the differences between groups significantly promoted these effects.
Considering the results, any of the 3 techniques is better than using S1 instrumentation as the caudal part at all [3]. While spinopelvic fixation is nowadays achieved via a range of approaches, iliac and S2AI screws are presently the most commonly used ones. Caudal instrumentation down to the pelvic ring offers reinforced biomechanical strength, especially if long fusions extend to the sacrum or in cases of sacrectomy, osteoporosis, and deformity surgery necessitating osteotomies or general revisions [13]. Clinically, additional iliac screws have been shown to be superior in neuromuscular spinal deformities and overall pediatric patients [14]. The same is true in adult revision cases after failed lumbosacropelvic fixation. Even in those cases, lumbosacral fusion could be promoted [15].
Although literature reports a considerably high rate of lumbosacral non-fusion of up to 83%, the rate was considerably lower in our series, despite the analyzed groups and despite all cases being revision cases [1, 2, 16,17,18]. Although iliac screws became standard over the last decade in many centers due to superior construct endurance, screw prominence can induce pain, sitting difficulty, and can even require screw removal [1, 19, 20]. However, this was not the case in our iliac screw cohort. Despite new technical reports on reducing iliac screw prominence, S2AI screws do not harbor this issue at all [21]. Typically, and as our series does, such surgeries harbor not only an increased risk of perioperative surgical but also medical complications [22], despite the outcome usually being affected [23].
The current best level of evidence originates from a meta-analysis of 5 retrospective studies reporting a significantly lower rate of revision surgery, wound infection, and screw-related pain for S2AI versus iliac screws [22]. However, this study reported heterogeneous data of different centers with therefore even reported selection bias. Furthermore, although our study, as does the reported one, also reflects level III evidence, it not only reports on homogeneous single-center data but also investigates the potential of such instrumentation to treat SIJ pain originating from overstressed SIJ due to long cranial cantilever transmitted by the sacral instrumentation, which is a sparsely investigated issue. While another study showed that S2AI screws cause less postoperative SIJ pain compared with S1, S2, or L5 screws as the caudal end of the construct, our study actually shows that in this matter, S2AI screws are even superior to iliac screws [24]. With these results, our study is the first to prove not only that S2AI screws improve already existing SIJ pain, but also the superiority of this approach to iliac screws. Although both techniques bridge the SIJ, there seems to be some remaining minor but still sufficient movement within the SIJ in case that iliac screws are used. S2AI screws, in contrast, go directly through the SIJ and therefore cease even minor movement within the SIJ. This not only is relevant surgically considering SIJ pain as a disabling sequelae of sacral instrumentation but also shows us, impressively, how little movement within the SIJ is able to elicit this pain and how large the forces onto the SIJ after instrumentation down to the sacrum need to be. This is relevant especially when considering trans-SIJ plating as a sufficient treatment of SIJ pain.
In previous studies, such as the already mentioned meta-analysis, there was a difference in indications for spinopelvic instrumentation and in the rate of patients receiving anterior cage support [22], which was not the case in our series. Furthermore, the lower rate of SL of the S2AI screws compared with sacral and iliac screws is well in accordance with previous data, which seems mostly due to omission of connectors as a potential source of failure and the stronger cortical purchase by crossing 3 cortical bone structures. Crossing 3 cortical bone structures seems to be the main issue defining the persistence of the S2AI screws. A cadaveric study proved that 65-mm S2AI screws were as strong as 80-mm S2AI and 90-mm iliac screws, showing that the tricortical purchase and not the overall length seems decisive [25]. Considering additional anterior column support via the anterior, oblique, and lateral of posterior cages is regarded as essential to promote fusion and relieve stress from posterior elements [13, 26]. Despite our cohort reporting a direct comparison of 3 very homogeneous groups of one center, mean FU was long enough to be within the commonly reported time prone to SL. Nonetheless, our cohort does not report standardized questionnaires and can therefore only report the subjectively experienced gluteal pain plus the objectively detected SL.
Conclusion
In conclusion, even in shorter or mid-length lumbar or thoracolumbar constructs, S2AI might be considered superior to S2A and I instrumentation due to lower incidences of caudal SL and SIJ pain. However, the superiority not only is in the outcome, but the surgical technique also provides some advantages by allowing for small incisions due to diverging trajectories, less dissection, and in-line rod bending without the need for additional connectors. Because the trajectory is more demanding, thus potentially causing more anterior complications, we recommend spinal navigation to ease the approach, as done in all cases of this study. Although our data might be partially biased, the results and clinical experience are clear. We therefore advocate for the S2AI technique as the caudal end of longer instrumentations. Future prospective studies enrolling larger series should be conducted to confirm these initial results.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C (2006) Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976) 31(3):303–308. https://doi.org/10.1097/01.brs.0000197193.81296.f1
Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G (2006) Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976) 31(20):2329–2336. https://doi.org/10.1097/01.brs.0000238968.82799.d9
Yasuda T, Hasegawa T, Yamato Y, Kobayashi S, Togawa D, Banno T, Arima H, Oe S, Matsuyama Y (2016) Lumbosacral junctional failures after long spinal fusion for adult spinal deformity-which vertebra is the preferred distal instrumented vertebra? Spine Deform 4(5):378–384. https://doi.org/10.1016/j.jspd.2016.03.001
Allen BL Jr, Ferguson RL (1982) The Galveston technique for L rod instrumentation of the scoliotic spine. Spine (Phila Pa 1976) 7(3):276–284. https://doi.org/10.1097/00007632-198205000-00014
Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS (2002) Outcome and complications of long fusions to the sacrum in adult spine deformity: Luque-Galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976) 27(7):776–786. https://doi.org/10.1097/00007632-200204010-00017
Schwend RM, Sluyters R, Najdzionek J (2003) The pylon concept of pelvic anchorage for spinal instrumentation in the human cadaver. Spine (Phila Pa 1976) 28(6):542–547. https://doi.org/10.1097/01.BRS.0000049925.58996.66
Colo G, Cavagnaro L, Alessio-Mazzola M, Zanirato A, Felli L, Formica M (2019) Incidence, diagnosis and management of sacroiliitis after spinal surgery: a systematic review of the literature. Musculoskelet Surg 104:111–123. https://doi.org/10.1007/s12306-019-00607-0
Chang TL, Sponseller PD, Kebaish KM, Fishman EK (2009) Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976) 34(5):436–440. https://doi.org/10.1097/BRS.0b013e318194128c
Hasan MY, Liu G, Wong HK, Tan JH (2020) Postoperative complications of S2AI versus iliac screw in spinopelvic fixation: a meta-analysis and recent trends review. Spine J 20(6):964–972. https://doi.org/10.1016/j.spinee.2019.11.014
Casaroli G, Bassani T, Brayda-Bruno M, Luca A, Galbusera F (2019) What do we know about the biomechanics of the sacroiliac joint and of sacropelvic fixation? A literature review. Med Eng Phys 76:1–12. https://doi.org/10.1016/j.medengphy.2019.10.009
Laratta JL, Shillingford JN, Meredith JS, Lenke LG, Lehman RA, Gum JL (2018) Robotic versus freehand S2 alar iliac fixation: in-depth technical considerations. J Spine Surg 4(3):638–644. https://doi.org/10.21037/jss.2018.06.13
Schwaiger BJ, Gersing AS, Baum T, Noel PB, Zimmer C, Bauer JS (2014) Bone mineral density values derived from routine lumbar spine multidetector row CT predict osteoporotic vertebral fractures and screw loosening. AJNR Am J Neuroradiol 35(8):1628–1633. https://doi.org/10.3174/ajnr.A3893
Kebaish KM (2010) Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976) 35(25):2245–2251. https://doi.org/10.1097/BRS.0b013e3181f5cfae
Sponseller PD, Yang JS, Thompson GH, McCarthy RE, Emans JB, Skaggs DL, Asher MA, Yazici M, Poe-Kochert C, Kostial P, Akbarnia BA (2009) Pelvic fixation of growing rods: comparison of constructs. Spine (Phila Pa 1976) 34(16):1706–1710. https://doi.org/10.1097/BRS.0b013e3181ab240e
Harimaya K, Mishiro T, Lenke LG, Bridwell KH, Koester LA, Sides BA (2011) Etiology and revision surgical strategies in failed lumbosacral fixation of adult spinal deformity constructs. Spine (Phila Pa 1976) 36(20):1701–1710. https://doi.org/10.1097/BRS.0b013e3182257eaf
Stovall DO Jr, Goodrich JA, Lundy D, Standard SC, Joe C, Preston CD (1997) Sacral fixation technique in lumbosacral fusion. Spine (Phila Pa 1976) 22(1):32–37. https://doi.org/10.1097/00007632-199701010-00006
Peelle MW, Lenke LG, Bridwell KH, Sides B (2006) Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: Galveston rod versus iliac and lumbosacral screws. Spine (Phila Pa 1976) 31(20):2392–2398; Discussion 2399. https://doi.org/10.1097/01.brs.0000238973.13294.16
Kim YJ, Bridwell KH, Lenke LG, Cho KJ, Edwards CC 2nd, Rinella AS (2006) Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Joint Surg Am 88(4):721–728. https://doi.org/10.2106/JBJS.E.00550
Elder BD, Ishida W, Lo SL, Holmes C, Goodwin CR, Kosztowski TA, Bydon A, Gokaslan ZL, Wolinsky JP, Sciubba DM, Witham TF (2017) Use of S2-alar-iliac screws associated with less complications than iliac screws in adult lumbosacropelvic fixation. Spine (Phila Pa 1976) 42(3):E142–E149. https://doi.org/10.1097/BRS.0000000000001722
Mazur MD, Ravindra VM, Schmidt MH, Brodke DS, Lawrence BD, Riva-Cambrin J, Dailey AT (2015) Unplanned reoperation after lumbopelvic fixation with S-2 alar-iliac screws or iliac bolts. J Neurosurg Spine 23(1):67–76. https://doi.org/10.3171/2014.10.SPINE14541
Sohn S, Chung CK, Kim YJ, Kim CH, Park SB, Kim H (2016) Modified iliac screw fixation: technique and clinical application. Acta Neurochir 158(5):975–980. https://doi.org/10.1007/s00701-016-2772-x
De la Garza RR, Nakhla J, Sciubba DM, Yassari R (2018) Iliac screw versus S2 alar-iliac screw fixation in adults: a meta-analysis. J Neurosurg Spine 30(2):253–258. https://doi.org/10.3171/2018.7.SPINE18710
Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG (2007) The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 32(24):2764–2770. https://doi.org/10.1097/BRS.0b013e31815a7644
Unoki E, Miyakoshi N, Abe E, Kobayashi T, Abe T, Kudo D, Shimada Y (2019) Sacropelvic fixation with S2 alar iliac screws may prevent sacroiliac joint pain after multisegment spinal fusion. Spine (Phila Pa 1976) 44(17):E1024–E1030. https://doi.org/10.1097/BRS.0000000000003041
O'Brien JR, Yu W, Kaufman BE, Bucklen B, Salloum K, Khalil S, Gudipally M (2013) Biomechanical evaluation of S2 alar-iliac screws: effect of length and quad-cortical purchase as compared with iliac fixation. Spine (Phila Pa 1976) 38(20):E1250–E1255. https://doi.org/10.1097/BRS.0b013e31829e17ff
Guler UO, Cetin E, Yaman O, Pellise F, Casademut AV, Sabat MD, Alanay A, Grueso FS, Acaroglu E, European Spine Study G (2015) Sacropelvic fixation in adult spinal deformity (ASD); a very high rate of mechanical failure. Eur Spine J 24(5):1085–1091. https://doi.org/10.1007/s00586-014-3615-1
Funding
Open Access funding provided by Projekt DEAL. The study was financed by institutional grants.
Author information
Authors and Affiliations
Contributions
Conceptualization: Sandro M. Krieg, Nico Sollmann, Bernhard Meyer
Methodology: Sandro M. Krieg, Nico Sollmann, Sebastian Ille, Lucia Albers, Bernhard Meyer
Formal analysis and investigation: Sandro M. Krieg, Nico Sollmann, Sebastian Ille, Lucia Albers, Bernhard Meyer
Writing—original draft preparation: Sandro M. Krieg, Nico Sollmann
Writing—review and editing: Sebastian Ille, Lucia Albers, Bernhard Meyer
Funding acquisition: Sandro M. Krieg, Bernhard Meyer
Resources: Sandro M. Krieg, Bernhard Meyer
Supervision: Bernhard Meyer
Corresponding author
Ethics declarations
Conflict of interest
SK is consultant for Nexstim Plc (Helsinki, Finland) and Spineart Deutschland GmbH (Frankfurt, Germany) and received honoraria from Medtronic (Meerbusch, Germany) and Carl Zeiss Meditec (Oberkochen, Germany). SK and BM received research grants and are consultants for Brainlab AG (Munich, Germany). BM received honoraria, consulting fees, and research grants from Medtronic (Meerbusch, Germany), icotec ag (Altstätten, Switzerland), and Relievant Medsystemy Inc. (Sunnyvale, CA, USA), honoraria and research grants from Ulrich Medical (Ulm, Germany), honoraria and consulting fees from Spineart Deutschland GmbH (Frankfurt, Germany) and DePuy Synthes (West Chester, PA, USA), and royalties from Spineart Deutschland GmbH (Frankfurt, Germany). NS received honoraria from Nexstim Plc (Helsinki, Finland). SI is consultant for Brainlab AG (Munich, Germany). However, all authors declare that they have no conflict of interest regarding the materials used or the results presented in this study.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (registration number: 159/16S) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was not required due to the retrospective character of the study and conditions of our local ethics committee.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ethics committee registration number: 159/16S
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Krieg, S.M., Sollmann, N., Ille, S. et al. Revision by S2-alar-iliac instrumentation reduces caudal screw loosening while improving sacroiliac joint pain—a group comparison study. Neurosurg Rev 44, 2145–2151 (2021). https://doi.org/10.1007/s10143-020-01377-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01377-1