Abstract
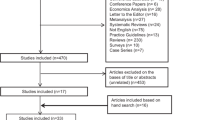
Whether intermittent pneumatic compression (IPC) is a more effective form of thromboprophylaxis than anticoagulants in individuals undergoing neurosurgery remains controversial. Relevant studies are sparse and inconsistent. Therefore, direct comparisons are difficult to perform and impractical. Hence, we summarized and compared the efficacy and safety of IPC and anticoagulants for the prevention of venous thromboembolism (VTE) in adults undergoing cranial or spinal procedures. Several electronic databases were searched for randomized controlled trials on the use of IPC and anticoagulants for thromboembolism prevention in neurosurgical patients, from inception to August 6, 2019. Studies reporting the selected endpoints were included in direct and Bayesian network meta-analyses to estimate the relative effects of the interventions. Overall, our analysis included 18 trials comprising 2474 patients. Both IPC (RR, 0.41; 95% CrI, 0.26–0.60) and chemical prophylaxis (RR, 0.48; 95% CrI, 0.28–0.68) were found to be more efficacious than the placebo in reducing the risk of deep vein thrombosis (DVT). In addition, our analysis also demonstrated that both IPC (RR, 0.10; 95% CrI, 0.01–0.60) and chemical prophylaxis (RR, 0.31; 95% CrI, 0.05–1.00) reduced the risk of pulmonary embolism (PE) significantly more than the placebo. Based on the available evidence of moderate-to-good quality, IPC is equivalent to anticoagulants for thromboprophylaxis in terms of efficacy. Evidence to support or negate the use of pharmacological prophylaxis in terms of safety is lacking. The results of ongoing and future large randomized clinical trials are needed.




Similar content being viewed by others
References
Epley D (2000) Pulmonary emboli risk reduction. J Vasc Nurs 18:61–68 quiz 69-70
Heit JA (2012) Estimating the incidence of symptomatic postoperative venous thromboembolism: the importance of perspective. JAMA 307:306–307
Beckman MG, Hooper WC, Critchley SE, Ortel TL (2010) Venous thromboembolism: a public health concern. Am J Prev Med 38:S495–S501
Cerrato D, Ariano C, Fiacchino F (1978) Deep vein thrombosis and low-dose heparin prophylaxis in neurosurgical patients. J Neurosurg 49:378–381
Collen JF, Jackson JL, Shorr AF, Moores LK (2008) Prevention of venous thromboembolism in neurosurgery: a metaanalysis. Chest 134:237–249
Agnelli G (2004) Prevention of venous thromboembolism in surgical patients. Circulation 110:IV-4–IV-12
Guyatt GH, Akl EA, Crowther M, Gutterman DD, Schuunemann HJ (2012) Executive summary: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:7s–47s
Danish SF, Burnett MG, Stein SC (2004) Prophylaxis for deep venous thrombosis in patients with craniotomies: a review. Neurosurg Focus 17:E2
Hamilton MG, Yee WH, Hull RD, Ghali WA (2011) Venous thromboembolism prophylaxis in patients undergoing cranial neurosurgery: a systematic review and meta-analysis. Neurosurgery 68:571–581
Iorio A, Agnelli G (2000) Low-molecular-weight and unfractionated heparin for prevention of venous thromboembolism in neurosurgery: a meta-analysis. Arch Intern Med 160:2327–2332
Giancarlo Agnelli MD, Franco Piovella MD, Pio Buoncristiani MD et al (1998) Enoxaparin plus compression stockings compared with compression stockings alone in the prevention of venous thromboembolism after elective neurosurgery. N Engl J Med 110:Iv4–I12
Danish SF, Burnett MG, Ong JG, Sonnad SS, Maloney-Wilensky E, Stein SC (2005) Prophylaxis for deep venous thrombosis in craniotomy patients: a decision analysis. Neurosurgery 56:1286–1292 discussion 1292-1284
Shaikhouni A, Baum J, Lonser RR (2018) Deep vein thrombosis prophylaxis in the neurosurgical patient. Neurosurg Clin N Am 29:567–574
Prell J, Schenk G, Taute BM et al (2018) Reduced risk of venous thromboembolism with the use of intermittent pneumatic compression after craniotomy: a randomized controlled prospective study. J Neurosurg Mar 1:1–7
Sobieraj-Teague M, Hirsh J, Yip G et al (2012) Randomized controlled trial of a new portable calf compression device (Venowave) for prevention of venous thrombosis in high-risk neurosurgical patients. J Thromb Haemost 10:229–235
Kurtoglu M, Yanar H, Bilsel Y, Guloglu R, Kizilirmak S, Buyukkurt D, Granit V (2004) Venous thromboembolism prophylaxis after head and spinal trauma: intermittent pneumatic compression devices versus low molecular weight heparin. World J Surg 28:807–811
Dickinson LD, Miller LD, Patel CP, Gupta SK (1998) Enoxaparin increases the incidence of postoperative intracranial hemorrhage when initiated preoperatively for deep venous thrombosis prophylaxis in patients with brain tumors. Neurosurgery 43:1074–1081
Schunemann HJ, Cushman M, Burnett AE et al (2018) American Society of Hematology 2018 guidelines for management of venous thromboembolism: prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv 2:3198–3225
Anderson DR, Morgano GP, Bennett C et al (2019) American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv 3:3898–3944
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, Mulrow C, Catalá-López F, Gøtzsche PC, Dickersin K, Boutron I, Altman DG, Moher D (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162:777–784
Turpie AG, Gallus A, Beattie WS, Hirsh J (1977) Prevention of venous thrombosis in patients with intracranial disease by intermittent pneumatic compression of the calf. Neurology 27:435–438
Skillman JJ, Collins REC, Coe NP et al (1978) Prevention of deep vein thrombosis in neurosurgical patients: a controlled, randomized trial of external pneumatic compression boots. Surgery 83:354–358
Turpie AGG, Delmore T, Hirsh J, Hull R, Genton E, Hiscoe C, Gent M (1979) Prevention of venous thrombosis by intermittent sequential calf compression in patients with intracranial disease. Thromb Res 15:611–616
Gruber UF, Rem J, Meisner C, Gratzl O (1984) Prevention of thromboembolic complications with miniheparin-dihydroergotamine in patients undergoing lumbar disc operations. Eur Arch Psychiatry Neurol Sci 234:157–161
Weitz J, Michelsen J, Gold K, Owen J, Carpenter D (1986) Effects of intermittent pneumatic calf compression on postoperative thrombin and plasmin activity. Thromb Haemost 56:198–201
Bucci MN, Papadopoulos SM, Chen JC, Campbell JA, Hoff JT (1989) Mechanical prophylaxis of venous thrombosis in patients undergoing craniotomy: a randomized trial. Surg Neurol 32:285–288
Turpie AG, Hirsh J, Gent M, Julian D, Johnson J (1989) Prevention of deep vein thrombosis in potential neurosurgical patients: a randomized trial comparing graduated compression stockings alone or graduated compression stockings plus intermittent pneumatic compression with control. Arch Intern Med 149:679–681
Nurmohamed MT, van Riel AM, Henkens CM et al (1996) Low molecular weight heparin and compression stockings in the prevention of venous thromboembolism in neurosurgery. Thromb Haemost 75:233–238
Wautrecht JC, MacQuaire V, Vandesteene A et al (1996) Prevention of deep vein thrombosis in neurosurgical patients with brain tumors: a controlled, randomized study comparing graded compression stockings alone and with intermittent sequential compression. Correlation with pre- and postoperative fibrinolysis. Preliminary results. Int Angiol 15:5–10
Constantini S, Kanner A, Friedman A, Shoshan Y, Israel Z, Ashkenazi E, Gertel M, Even A, Shevach Y, Shalit M, Umansky F, Rappaport ZH (2001) Safety of perioperative minidose heparin in patients undergoing brain tumor surgery: a prospective, randomized, double-blind study. J Neurosurg 94:918–921
Hamidi S, Riazi M (2015) Incidence of venous thromboembolic complications in instrumental spinal surgeries with preoperative chemoprophylaxis. J Korean Neurosurg Soc 57:114–118
Melon E, Keravel Y, Gaston A (1991) Deep venous thrombosis prophylaxis by low molecular weight heparin in neurosurgical patients. Anesthesiology 75:A214
Arnold PM, Harrop JS, Merli G, Tetreault LG, Kwon BK, Casha S, Palmieri K, Wilson JR, Fehlings MG, Holmer HK, Norvell DC (2017) Efficacy, safety, and timing of anticoagulant thromboprophylaxis for the prevention of venous thromboembolism in patients with acute spinal cord injury: a systematic review. Global Spine J 7:138S–150S
O’Connell S, Bashar K, Broderick BJ, Sheehan J, Quondamatteo F, Walsh SR, ÓLaighin G, Quinlan LR (2016) The use of intermittent pneumatic compression in orthopedic and neurosurgical postoperative patients: a systematic review and meta-analysis. Ann Surg 263:888–889
Khan NR, Patel PG, Sharpe JP, Lee SL, Sorenson J (2018) Chemical venous thromboembolism prophylaxis in neurosurgical patients: an updated systematic review and meta-analysis. J Neurosurg 129:906–915
Funding
This work was funded by the 1.3.5 Project for Disciplines of Excellence of West China Hospital of Sichuan University (grant number: ZY2016102).
Author information
Authors and Affiliations
Contributions
Dr. Fang was the guarantor of the review. Dr. You received the funding.
Project design: Wang, Zhang, and Fang; data collection: Wang, Zhang, Fang, Jia, Faramand, You, and Xu; manuscript drafting: Wang, Zhang, Fang, Jia, Faramand, You, and Xu; statistical analysis: Wang, Zhang, Fang, Jia, Faramand, You, and Xu; manuscript revision: Wang, Zhang, Fang, Faramand, and You. Supervision: Wang, Zhang, and Fang.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not required.
Informed consent
Not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 1453 kb)
Rights and permissions
About this article
Cite this article
Wang, X., Zhang, Y., Fang, F. et al. Comparative efficacy and safety of pharmacological prophylaxis and intermittent pneumatic compression for prevention of venous thromboembolism in adult undergoing neurosurgery: a systematic review and network meta-analysis. Neurosurg Rev 44, 721–729 (2021). https://doi.org/10.1007/s10143-020-01297-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01297-0