Abstract
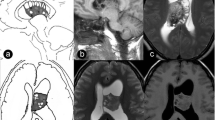
Microcystic meningioma (MM) is a rare subtype of intracranial meningiomas, with clinical and radiologic features not well characterized in the literature. Based on our experience, we propose a classification system of intracranial MMs. We reviewed the medical records, radiographic studies, and operative notes of a group of consecutive patients with intracranial MM. The mean age of the 69 patients was 46.8 ± 10.6 years (range, 21–75 years). Three types of intracranial MMs could be identified. Type 1 MMs presented as a solid lesion, hypointense or isointense on T1WI, hyperintense on T2WI, and homogeneous or heterogeneous enhancement, and were found in 43 patients (67.2%). Type 2 MMs represented signals similar to CSF both on T1WI and T2WI, and faint reticular enhancement with marginal enhancement, and these were found in 7 patients (10.9%). Type 3 MMs consisted of cystic-solid or cystic lesion and were found in 14 patients (21.9%). Significant differences were observed among the different types of MMs for the following variables: sex, presence of severe peritumoral brain edema (PTBE), and extent of tumor resection. Females were found in all of patients with type 2 MMs, but were only 35.7% of those with type 3 MMs (P = 0.018). Severe PTBEs were more common among patients with type 1 MMs (55.8%) than among those with type 2 (14.3%) and type 3 MMs (14.3%) (P = 0.007). Type 1 MMs (97.7%) were associated with a significantly higher rate of gross total resection compared with the other two types (71.4 and 78.6%) (P = 0.019). Total length of hospital stay after craniotomy ranged from 4 to 30 days (median, 8 days). There were no significant differences in progression-free survival among the three types of MMs (P = 0.788). The current classification identifies three distinct types of intracranial MM based on their radiological findings and growth patterns. The type 1 MMs are more commonly associated with severe PTBE. Type 2 and Type 3 MMs have a higher predilection towards parasaggital location with venous involvement and therefore have a lower rate of gross total resection.





Similar content being viewed by others
Abbreviations
- MM :
-
microcystic meningioma
- T1WI :
-
T1-weighted images
- T2WI :
-
T2-weighted images
- WHO :
-
World Health Organization
- MRI :
-
magnetic resonance image
- PTBE :
-
peritumoral brain edema
- EI :
-
edema index
- KPS :
-
Karnofsky performance scale
- GTR :
-
gross total resection
- STR:
-
subtotal resection
- VEGF :
-
vascular endothelial growth factor
- PFS :
-
progression-free survival
- OS :
-
overall survival
- PM :
-
psammomatous meningioma
References
Boukobza M, Cebula H, Pop R, Kouakou F, Sadoun A, Coca HA, Polivka M, Diemidio P, Ganau M, George B, Froelich S, Proust F, Chibbaro S (2016) Cystic meningioma: radiological, histological, and surgical particularities in 43 patients. Acta Neurochir 158:1955–1964
Buetow MP, Buetow PC, Smirniotopoulos JG (1991) Typical, atypical, and misleading features in meningioma. Radiographics 11:1087–1106
Burger PC (1995) Revising the World Health Organization (WHO) blue book—‘Histological typing of tumours of the central nervous system’. J Neuro-Oncol 24:3–7
Cha S, Knopp EA, Johnson G, Wetzel SG, Litt AW, Zagzag D (2002) Intracranial mass lesions: dynamic contrast-enhanced susceptibility-weighted echo-planar perfusion MR imaging. Radiology 223:11–29
Chen CJ, Tseng YC, Hsu HL, Jung SM (2008) Microcystic meningioma: importance of obvious hypointensity on T1-weighted magnetic resonance images. J Comput Assist Tomogr 32:130–134
Christov C, Lechapt-Zalcman E, Adle-Biassette H, Nachev S, Gherardi RK (1999) Vascular permeability factor/vascular endothelial growth factor (VPF/VEGF) and its receptor flt-1 in microcystic meningiomas. Acta Neuropathol 98:414–420
Danisman MC, Kelesoglu KS, Sivri M, Koplay M, Paksoy Y (2017) Microcystic meningioma: difficulties in diagnosis and magnetic resonance imaging findings. Acta Neurol Belg 117:745–747
Goldman CK, Bharara S, Palmer CA, Vitek J, Tsai JC, Weiss HL, Gillespie GY (1997) Brain edema in meningiomas is associated with increased vascular endothelial growth factor expression. Neurosurgery 40:1269–1277
Hakyemez B, Yildirim N, Erdoğan C, Kocaeli H, Korfali E, Parlak M (2006) Meningiomas with conventional MRI findings resembling intraaxial tumors: can perfusion-weighted MRI be helpful in differentiation? Neuroradiology 48:695–702
Kalani MY, Cavallo C, Coons SW, Lettieri SC, Nakaji P, Porter RW, Spetzler RF, Feiz-Erfan I (2015) Long-term follow-up of surgical resection of microcystic meningiomas. J Clin Neurosci 22:713–717
Kalkanis SN, Carroll RS, Zhang J, Zamani AA, Black PM (1996) Correlation of vascular endothelial growth factor messenger RNA expression with peritumoral vasogenic cerebral edema in meningiomas. J Neurosurg 85:1095–1101
Kim SH, Kim DG, Kim CY, Choc G, Chang KH, Jung HW (2003) Microcystic meningioma: the characteristic neuroradiologic findings. J Korean Neurosurg S 35:401–406
Kleihues P, Burger PC, Scheithauer BW (1993) The new WHO classification of brain tumours. Brain Pathol 3:255–268
Kubota Y, Ueda T, Kagawa Y, Sakai N, Hara A (1997) Microcystic meningioma without enhancement on neuroimaging: case report. Neurol Med Chir (Tokyo) 37:407–410
Kuchna I, Matyja E, Wierzba-Bobrowicz T, Mazurowski W (1994) Microcystic meningioma—a rarely occurring morphological variant of meningioma. Folia Neuropathol 32:259–263
Kunimatsu A, Kunimatsu N, Kamiya K, Katsura M, Mori H, Ohtomo K (2016) Variants of meningiomas: a review of imaging findings and clinical features. Jpn J Radiol 34:459–469
Lin Z, Zhao M, Ren X, Wang J, Li Z, Chen X, Wang Y, Li X, Wang C, Jiang Z (2017) Clinical features, radiologic findings, and surgical outcomes of 65 intracranial psammomatous meningiomas. World Neurosurg 100:395–406
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820
Matsushima N, Maeda M, Takamura M, Matsubara T, Taki W, Takeda K (2007) MRI findings of atypical meningioma with microcystic changes. J Neuro-Oncol 82:319–321
Michaud J, Gagne F (1983) Microcystic meningioma. Clinicopathologic report of eight cases. Arch Pathol Lab Med 107:75–80
Nishio S, Takeshita I, Morioka T, Fukui M (1994) Microcystic meningiomas: clinicopathological features of 6 cases. Neurol Res 16:251–256
Osawa T, Tosaka M, Nagaishi M, Yoshimoto Y (2013) Factors affecting peritumoral brain edema in meningioma: special histological subtypes with prominently extensive edema. J Neuro-Oncol 111:49–57
Ostrom QT, Gittleman H, Farah P, Ondracek A, Chen Y, Wolinsky Y, Stroup NE, Kruchko C, Barnholtz-Sloan JS (2013) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2006–2010. Neuro-Oncology 15(suppl 2):ii1–ii56
Paek SH, Kim CY, Kim YY, Park IA, Kim MS, Kim DG, Jung HW (2002) Correlation of clinical and biological parameters with peritumoral edema in meningioma. J Neuro-Oncol 60:235–245
Paek SH, Kim SH, Chang KH, Park CK, Kim JE, Kim DG, Park SH, Jung HW (2005) Microcystic meningiomas: radiological characteristics of 16 cases. Acta Neurochir 147:965–972
Provias J, Claffey K, delAguila L, Lau N, Feldkamp M, Guha A (1997) Meningiomas: role of vascular endothelial growth factor/vascular permeability factor in angiogenesis and peritumoral edema. Neurosurgery 40:1016–1026
Raza SM, Gallia GL, Brem H, Weingart JD, Long DM, Olivi A (2010) Perioperative and long-term outcomes from the management of parasagittal meningiomas invading the superior sagittal sinus. Neurosurgery 67:885–893
Rishi A, Black KS, Woldenberg RW, Overby CM, Eisenberg MB, Li JY (2011) Microcystic meningioma presenting as a cystic lesion with an enhancing mural nodule in elderly women: report of three cases. Brain Tumor Pathol 28:335–339
Roser F, Nakamura M, Ritz R, Bellinzona M, Dietz K, Samii M, Tatagiba MS (2005) Proliferation and progesterone receptor status in benign meningiomas are not age dependent. Cancer 104:598–601
Sawada K, Tamaki M, Hashimoto H, Karakama J, Sato Y, Hara M, Tone O (2016) A case of microcystic meningioma with a difficult preoperative diagnosis. Jpn J Neurosurg (Tokyo) 25:62–68
Schober R, Himuro H, Wechsler W (1988) Cystic changes and vascular permeability in meningiomas. Clin Neuropathol 7:16–21
Shimoji K, Yasuma Y, Mori K, Eguchi M, Maeda M (1999) Unique radiological appearance of a microcystic meningioma. Acta Neurochir 141:1119–1121
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 20:22–39
Sitthinamsuwan B, Khampalikit I, Nunta-aree S, Srirabheebhat P, Witthiwej T, Nitising A (2012) Predictors of meningioma consistency: a study in 243 consecutive cases. Acta Neurochir 154:1383–1389
Tamiya T, Ono Y, Matsumoto K, Ohmoto T (2001) Peritumoral brain edema in intracranial meningiomas: effects of radiological and histological factors. Neurosurgery 49:1046–1051
Vernooij MW, Ikram MA, Tanghe HL, Vincent AJ, Hofman A, Krestin GP, Niessen WJ, Breteler MM, van der Lugt A (2007) Incidental findings on brain MRI in the general population. N Engl J Med 357:1821–1828
Vignes JR, Sesay M, Rezajooi K, Gimbert E, Liguoro D (2008) Peritumoral edema and prognosis in intracranial meningioma surgery. J Clin Neurosci 15:764–768
Watts J, Box G, Galvin A, Brotchie P, Trost N, Sutherland T (2014) Magnetic resonance imaging of meningiomas: a pictorial review. Insights Imaging 5:113–122
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this retrospective study formal consent was not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Lin, Z., Zhao, M., Li, X. et al. Characteristic features and proposed classification in 69 cases of intracranial microcystic meningiomas. Neurosurg Rev 42, 443–453 (2019). https://doi.org/10.1007/s10143-018-0982-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-018-0982-9