Abstract
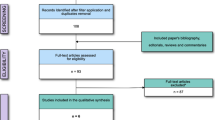
The purpose of this study was to determine the effect of aspirin therapy discontinuation on intraoperative blood loss in spinal surgery. We searched Medline and Google Scholar 1946 to January 2017 inclusive for case-control studies, cohort studies, and controlled trials reporting intraoperative blood loss during spinal surgery in patients on pre-operative aspirin. Other outcome measures reported in the eligible studies were collected as secondary outcomes. Two reviewers independently screened and extracted data from each study. Five retrospective cohort and two case-control studies were eligible for inclusion. Of the 1173 patients identified, 587 patients were never on aspirin (Ax), 416 patients had aspirin discontinued before surgery (Ad), ranging from 3 to 10 days, and 170 patients had aspirin continued until surgery (Ac). Six out of seven studies reported no statistically significant difference in intraoperative blood loss irrespective of aspirin discontinuation. Meta-analysis was not possible due to high risk of bias. Of the secondary outcome measures, operative time and postoperative complications were most commonly reported. One of six studies evaluating operative time reported a significantly longer operative time in the Ad group compared with the Ac group. The overall risk of postoperative haematoma in Ax, Ad, and Ac groups is 0.2% (n/N = 1/587), 0.2% (n/N = 1/416), and 1.2% (n/N = 2/170), respectively. No study reported a statistically significant difference in postoperative complications. There is no strong evidence demonstrating a difference in intraoperative blood loss, operation time, and postoperative complications, irrespective of aspirin discontinuation. This is, however, based on a limited number of studies and higher-quality research is required to answer this question with a higher degree of confidence.


Similar content being viewed by others
References
Akhavan-Sigari R, Rohde V, Abili M (2014) Continuation of medically necessary platelet aggregation inhibitors—acetylsalicylic acid and clopidogrel - during surgery for spinal degenerative disorders: results in 100 patients. Surg Neurol Int 5(8):S376–S379. https://doi.org/10.4103/2152-7806.139675
Antithrombotic Trialists’ Collaboration (2002) Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ (Clinical research ed) 324(7329):71–86. https://doi.org/10.1136/bmj.324.7329.71
Aono H, Ohwada T, Hosono N, Tobimatsu H, Ariga K, Fuji T, Iwasaki M (2011) Incidence of postoperative symptomatic epidural hematoma in spinal decompression surgery. J Neurosurg Spine 15(2):202–205. https://doi.org/10.3171/2011.3.SPINE10716
Bent N, Eckles L, Elliott N, Garner S, Fischer A, Hayre J, Jeong K, Kandaswamy P, Steel KM, Moore V, Naidoo B, O’Neill P, Owen L, Raynor M, Ray M, Rogers G, Royce J, Shaw B, Silvester J, Smith T, Staples N, Taylor L, Taske N, Tuvey D (2013) Appendix E methodology checklist: case-control studies. In: National Institute for Health and Care Excellence. https://www.nice.org.uk/process/pmg10/chapter/appendix-e-methodology-checklist-casecontrol-studies#checklist-4. Accessed 11 Mar 2017
Burger W, Chemnitius JM, Kneissl GD, Rücker G (2005) Low-close aspirin for secondary cardiovascular prevention—cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation—review and meta-analysis. J Intern Med 257(5):399–414. https://doi.org/10.1111/j.1365-2796.2005.01477.x
Chechik O, Thein R, Fichman G, Haim A, Ben TT, Steinberg EL (2011) The effect of clopidogrel and aspirin on blood loss in hip fracture surgery. Injury 42(11):1277–1282. https://doi.org/10.1016/j.injury.2011.01.011
Cuellar JM, Petrizzo A, Vaswani R, Goldstein JA, Bendo JA (2015) Does aspirin administration increase perioperative morbidity in patients with cardiac stents undergoing spinal surgery? Spine 40(9):629–635. https://doi.org/10.1097/BRS.0000000000000695
DiMinno MND, Prisco D, Ruocco AL, Mastronardi P, Massa S, Di Minno G (2009) Perioperative handling of patients on antiplatelet therapy with need for surgery. Intern Emerg Med 4(4):279–288. https://doi.org/10.1007/s11739-009-0265-0
Dina TS, Boden S, Davis D (1995) Lumbar spine after surgery for herniated disk: imaging findings in the early postoperative disk. Am J Roentgenol 164:665–671
Eubanks J (2016) Association between perioperative bleeding and aspirin use in spine surgery: a randomized, controlled trial. In: US National Library of Medicine: ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT02807441 . Accessed 10 May 2017
Gerstein NS, Schulman PM, Gerstein WH, Petersen TR, Tawil I (2012) Should more patients continue aspirin therapy perioperatively?: clinical impact of aspirin withdrawal syndrome. Ann Surg 255(5):811–819. https://doi.org/10.1097/SLA.0b013e318250504e
Glotzbecker MP, Bono CM, Wood KB, Harris MB (2010) Postoperative spinal epidural hematoma: a systematic review. Spine (Phila Pa 1976) 35(10):E413–E420. https://doi.org/10.1097/BRS.0b013e3181d9bb77
Hamamoto Y, Ogata T, Morino T, Hino M, Yamamoto H (2007) Real-time direct measurement of spinal cord blood flow at the site of compression: relationship between blood flow recovery and motor deficiency in spinal cord injury. Spine 32(18):1955–1962. https://doi.org/10.1097/BRS.0b013e3181316310
Harder S, Klinkhardt U, Alvarez JM (2004) Avoidance of bleeding during surgery in patients receiving anticoagulant and/or antiplatelet therapy: pharmacokinetic and pharmacodynamic considerations. Clin Pharmacokinet 43(14):963–981. https://doi.org/10.2165/00003088-200443140-00002
Harty J, McKenna P, Moloney D, D’Souza L, Masterson E (2007) Anti-platelet agents and surgical delay in elderly patients with hip fractures. J Orthop Surg 15(3):270–272. https://doi.org/10.1177/230949900701500304
Kang S-B, Cho K-J, Moon K-H, Jung J-H, Jung S-J (2011) Does low-dose aspirin increase blood loss after spinal fusion surgery? Spine J 11(4):303–307. https://doi.org/10.1016/j.spinee.2011.02.006
Kao FC, Tsai TT, Chen LH, Lai PL, Fu TS, Niu CC, Ho NYJ, Chen WJ, Chang CJ (2015) Symptomatic epidural hematoma after lumbar decompression surgery. Eur Spine J 24(2):348–357. https://doi.org/10.1007/s00586-014-3297-8
Korinth MC, Gilsbach JM, Weinzierl MR (2007) Low-dose aspirin before spinal surgery: results of a survey among neurosurgeons in Germany. Eur Spine J 16(3):365–372. https://doi.org/10.1007/s00586-006-0216-7
Kotilainen E, Alanen A, Erkintalo M, Valtonen S, Kormano M (1994) Magnetic resonance image changes and clinical outcome after microdiscectomy or nucleotomy for ruptured disc. Surg Neurol 41(6):432–440. https://doi.org/10.1016/0090-3019(94)90003-5
Kou J, Fischgrund J, Biddinger A, Herkowitz H (2002) Risk factors for spinal epidural hematoma after spinal surgery. Spine 27(15):1670–1673. https://doi.org/10.1097/01.BRS.0000018790.29835.35
Kreppel D, Antoniadis G, Seeling W (2003) Spinal hematoma: a literature survey with meta-analysis of 613 patients. Neurosurg Rev 26(1):1–49. https://doi.org/10.1007/s10143-002-0224-y
Lee JS, Son DW, Sung SK, Lee SW, Song GS (2016) Effects of discontinuance of preoperative anti-platelet medication in multi-level thoracolumbar spine surgery. Turkish Neurosurgery:1–6. https://doi.org/10.5137/1019-5149.JTN.18306-16.1
Liu Y, Li Y, Miao J (2016) Wound drains in posterior spinal surgery: a meta-analysis. J Orthop Surg Res 11(1):1–7. https://doi.org/10.1186/s13018-016-0351-8
Mantz J, Samama CM, Tubach F, Devereaux PJ, Collet J-P, Albaladejo P, Cholley B, Nizard R, Barré J, Piriou V, Poirier N, Mignon A, Schlumberger S, Longrois D, Aubrun F, Farèse ME, Ravaud P, Steg PG (2011) Impact of preoperative maintenance or interruption of aspirin on thrombotic and bleeding events after elective non-cardiac surgery: the multicentre, randomized, blinded, placebo-controlled, STRATAGEM trial†. BJA: Br J Anaesth 107(6):899–910. https://doi.org/10.1093/bja/aer274
McCunniff PT, Young ES, Ahmadinia K, Kusin DJ, Ahn UM, Ahn NU (2016) Chronic antiplatelet use associated with increased blood loss in lumbar spinal surgery despite adherence to protocols. Orthopedics 39(4):e695–e700. https://doi.org/10.3928/01477447-20160419-04
Modi HN, Lee DY, Lee S (2011) Postoperative spinal epidural hematoma after microscopic lumbar decompression. J Spinal Disord Tech 24(3):146–150. https://doi.org/10.1097/BSD.0b013e3181e1958e
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339(jul21 1):b2535. https://doi.org/10.1136/bmj.b2535
OCEBM Levels of Evidence Working Group (2011) The Oxford 2011 levels of evidence. Oxford Centre for Evidence-Based Medicine, In http://www.cebm.net/index.aspx?o=5653
Oscarsson A, Gupta A, Fredrikson M, Jarhult J, Nystrom M, Pettersson E, Darvish B, Krook H, Swahn E, Eintrei C (2010) To continue or discontinue aspirin in the perioperative period: a randomized, controlled clinical trial. Br J Anaesth 104(3):305–312. https://doi.org/10.1093/bja/aeq003
Park H-J, Kwon K-Y, Woo J-H (2014) Comparison of blood loss according to use of aspirin in lumbar fusion patients. Eur Spine J 23(8):1777–1782. https://doi.org/10.1007/s00586-014-3294-y
Park JH, Ahn Y, Choi BS, Choi K-T, Lee K, Kim SH, Roh SW (2013) Antithrombotic effects of aspirin on 1- or 2-level lumbar spinal fusion surgery. Spine 38(18):1561–1565. https://doi.org/10.1097/BRS.0b013e31829a84d2
Pauyo T, Verma N, Marwan Y, Aoude A, Khashan M, Weber MH (2017) Canadian consensus for the prevention of blood loss in spine surgery. Spine 42(1):E50–E55. https://doi.org/10.1097/BRS.0000000000001686
Soleman J, Baumgarten P, Perrig WN, Fandino J, Fathi A-R (2016) Non-instrumented extradural lumbar spine surgery under low-dose acetylsalicylic acid: a comparative risk analysis study. Eur Spine J 25(3):732–739. https://doi.org/10.1007/s00586-015-3864-7
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter J, Chan A-W, Churchill R, Hróbjartsson A, Kirkham J, Jüni P, Loke Y, Pigott T, Ramsay C, Regidor D, Rothstein H, Sandhu L, Santaguida P, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Whiting P, Higgins JP (2016) The Risk Of Bias In Non-randomized Studies – of Interventions (ROBINS-I) assessment tool ROBINS-I tool (stage I): at protocol stage. 1–22. https://doi.org/10.1136/bmj.i4919
Waly F, Alzahrani MM, Abduljabbar FH, Landry T, Ouellet J, Moran K, Dettori JR (2015) The outcome of using closed suction wound drains in patients undergoing lumbar spine surgery: a systematic review. Global Spine J 5(6):479–485. https://doi.org/10.1055/s-0035-1566288
Wilson DB Practical meta-analysis effect size calculator. https://www.campbellcollaboration.org/escalc/html/EffectSizeCalculator-SMD1.php
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was not required as presented data are anonymised and there is no risk of identification. This article does not contain any studies with human participants performed by any of the authors.
Informed consent
Consent was not obtained as presented data are anonymised and there is no risk of identification.
Electronic supplementary material
ESM 1
(PDF 126 kb)
Rights and permissions
About this article
Cite this article
Cheng, A., Poon, M.T.C. & Demetriades, A.K. Aspirin therapy discontinuation and intraoperative blood loss in spinal surgery: a systematic review. Neurosurg Rev 41, 1029–1036 (2018). https://doi.org/10.1007/s10143-018-0945-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-018-0945-1