Abstract
Pediatric distal forearm fractures, comprising 30% of musculoskeletal injuries in children, are conventionally diagnosed using radiography. Ultrasound has emerged as a safer diagnostic tool, eliminating ionizing radiation, enabling bedside examinations with real-time imaging, and proving effective in non-hospital settings. The objective of this study is to evaluate the diagnostic efficacy of ultrasound for detecting distal forearm fractures in the pediatric population. A systematic review and meta-analysis were conducted through a comprehensive literature search in PubMed, Scopus, Web of Science, and Embase databases until October 1, 2023, following established guidelines. Eligible studies, reporting diagnostic accuracy measures of ultrasound in pediatric patients with distal forearm fractures, were included. Relevant data elements were extracted, and data analysis was performed. The analysis included 14 studies with 1377 patients, revealing pooled sensitivity and specificity of 94.5 (95% CI 92.7–95.9) and 93.5 (95% CI 89.6–96.0), respectively. Considering pre-test probabilities of 25%, 50%, and 75% for pediatric distal forearm fractures, positive post-test probabilities were 83%, 44%, and 98%, while negative post-test probabilities were 2%, 6%, and 15%, respectively. The bivariate model indicated significantly higher diagnostic accuracy in the subgroup with trained ultrasound performers vs. untrained performers (p = 0.03). Furthermore, diagnostic accuracy was significantly higher in the subgroup examining radius fractures vs. ulna fractures (p < 0.001), while no significant differences were observed between 4-view and 6-view ultrasound subgroups or between radiologist ultrasound interpreters and non-radiologist interpreters. This study highlighted ultrasound’s reliability in detecting pediatric distal forearm fractures, emphasizing the crucial role of expertise in precisely confirming fractures through ultrasound examinations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distal forearm fractures in the pediatric population represent a significant share of musculoskeletal injuries, comprising around 30% of all fractures in children [1, 2]. The conventional diagnostic strategy predominantly involves radiography. However, this method presents notable limitations, including the potential for ionizing radiation exposure, the need for patient mobility during imaging, and challenges in identifying subtle fractures within the pediatric skeletal structure [3,4,5].
In recent years, ultrasound has emerged as a promising diagnostic tool for pediatric distal forearm fractures. Differing from conventional radiography, ultrasound offers a safer option for the pediatric population by eliminating ionizing radiation, which poses potential adverse effects [3, 6]. Its bedside applicability not only eliminates the need for patient transportation but also enables real-time imaging, potentially expediting the diagnostic process [7, 8]. Additionally, ultrasound presents advantages such as lower cost and higher availability [4, 9].
Recent studies have investigated the application of ultrasound in diagnosing pediatric forearm fractures, highlighting its capacity for dynamic, multi-planar visualization of both radial and ulnar cortices [10,11,12,13]. This dynamic capability effectively addresses challenges related to overlapping bone structures and provides advantages in identifying cortical disruptions and subperiosteal hematomas [7]. Moreover, the mobility of ultrasound facilitates bedside examinations, proving valuable in non-hospital settings and situations involving multiple-trauma patients [7, 8]. However, despite promising findings, the incorporation of diagnostic ultrasound into the clinical management of pediatric distal forearm fractures remains limited [4].
This study aims to conduct a meta-analysis on the diagnostic effectiveness of ultrasound in pediatric distal forearm fractures. Through a systematic review of the current literature, our objective is to offer insights into the viability of ultrasound as a diagnostic tool in the pediatric emergency setting.
Methods
This systematic review follows the guidelines outlined in the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement [14]. On October 1, 2023, a comprehensive literature search was conducted across four major databases: PubMed, Scopus, Web of Science, and Embase. Specific search terms were devised for each database, incorporating (“radius” OR “radial” OR “ulna” OR “ulnar” OR “forearm”) AND (“fracture*” OR “displace*”) AND (“sonograph*” OR “ultrasonograph*” OR “ultrasound” OR “POCUS”) AND (“pediatric*” OR “paediatric*” OR “child*” OR “neonat*” OR “infant*” OR “toddler*” OR “preschool” OR “pre-school” OR “juvenile” OR “young adult*”). Additionally, a thorough manual examination of references within the included studies ensured no relevant papers were inadvertently overlooked. The assessment process involved a detailed review of each article’s title, abstract, and/or full text. Two co-authors independently conducted this review, resolving uncertainties or ambiguities through consultation with a senior co-author. The AutoLit platform, developed by Nested Knowledge in St. Paul, Minnesota, USA, facilitated deduplication, screening, and data extraction.
All studies pertinent to the topic of interest, presenting at least one of the following diagnostic accuracy measures in pediatric patients (under 21 years old), were considered for inclusion: sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), likelihood ratio (LR), diagnostic odds ratio (DOR), and area under the receiver operating characteristic curve (AUC). No constraints were imposed on publication date, country of origin, patient characteristics, reference standard type, or study design. Non-English literature, case reports, case series with fewer than five eligible patients, conference abstracts, editorial comments, and review articles were excluded from the study.
The quality assessment of diagnostic accuracy studies-2 (QUADAS-2) tool was applied to evaluate the quality of included studies [15]. The four primary domains of the QUADAS-2 tool, including patient selection, index test, reference standard, and flow and timing, underwent independent assessment for potential bias and concerns regarding applicability. Evaluations for each domain were based on specific criteria outlined in the tool, such as the representativeness of the study population, blinding of test results, and completeness of outcome data. Ratings of “low,” “high,” or “unclear” were assigned to each domain to determine the overall rigor and reliability of the evidence synthesis.
Statistical analysis
The primary analytical approach utilized a random effects diagnostic test accuracy (DTA) model, specifically the bivariate model developed by Reitsma et al. [16]. Summary receiver operating characteristic (SROC) curves were generated using this bivariate meta-analysis data. For visualization purposes, study-specific estimates were relatively weighted in SROC plots based on the weights within the random effects univariate DOR model. AUC and its confidence interval (CI) for each subgroup were calculated using a 2000 sample bootstrapping technique based on the bivariate model [17].
To assess heterogeneity, the I2 metric was employed following the approach by Holling et al. [18]. A significant level for heterogeneity was considered for I2 confidence intervals above 25%, leading to further sensitivity analyses through the DOR univariate meta-analysis to identify and re-analyze potential outliers.
The study also investigated the influence of various covariates on the reported rates using subgroup meta-analysis and meta-regression techniques. Covariates included training status and roles of the individuals involved, image acquisition methods (either four or six views), and the age of patients. Considering the variability in reporting metrics, with some studies reporting by patient number and others by the number of bones scanned, these aspects were treated as covariates for further subgroup analyses. Subgroup comparisons were made between studies reporting on a patient-wise basis vs. those reporting on a bone-wise basis. Separate subgroup analyses were also conducted for studies reporting diagnostic accuracy metrics for fractures in the radius and ulna.
Fagan plots and LR scattergrams were utilized to assess the clinical applicability of findings. Positive LRs above ten signified suitability for confirmation, whereas negative LRs below 0.1 indicated exclusion suitability. Fagan nomograms were constructed for pre-test prevalences of 25%, 50%, and 75%, based on the bivariate Reitsma model, as detailed by Zwinderman et al. [19].
Publication bias was scrutinized using an adaptation of Egger’s regression test for DTA meta-analysis, involving the analysis of funnel plot asymmetry with 2000 sample bootstrapping, as recommended by Noma et al. [20].
All statistical procedures were conducted using R (version 4.2.1, R Foundation for Statistical Computing, Vienna, Austria), utilizing packages such as “Mada,” “MVPBT” [21], “dmetatools” [17], “Metafor” [22], and “meta” [23].
Results
Article screening and selection process
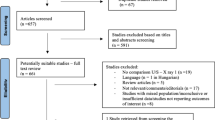
A systematic literature search employing a predetermined strategy identified 1570 articles. Upon removing duplicates, 746 papers underwent screening based on title and abstract. This screening process resulted in the exclusion of 718 articles, comprising 38 review articles, 19 editorials, 15 conference papers, 49 non-English articles, and 597 articles deemed irrelevant to the topic of interest. The full text of the remaining 28 papers was meticulously reviewed. After a thorough examination, 14 articles were excluded because they failed to report at least one diagnostic accuracy measure for ultrasound in the evaluation of pediatric distal forearm fractures. Ultimately, 14 articles meeting the inclusion criteria were identified and incorporated. The screening process and eligibility criteria adhered to PRISMA guidelines, with a flow diagram presented in Fig. 1.
Study and patient characteristics
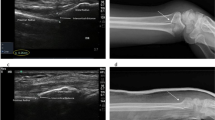
The analysis encompassed 14 studies involving a total of 1377 patients. The predominant methodology across these studies was prospective and single center. Distal forearm fractures were diagnosed using ultrasound, with radiography as the reference standard. Diagnostic criteria for fractures on ultrasound included the identification of cortical disruptions, protrusions, deviations, or hematomas. The studies utilized a diverse range of ultrasound equipment, with a linear transducer being the most commonly employed. Additionally, a 6-view imaging protocol was predominantly implemented. The ultrasound examinations were conducted by various professionals, such as traumatology residents, pediatric emergency physicians, nurses, and radiologists, each with varying levels of training in musculoskeletal ultrasound examination. Detailed sensitivity and specificity percentages, along with additional characteristics of the included studies, can be found in Table 1.
Quality assessment
The methodological quality of the incorporated studies is detailed in Table 2 and Supplementary Fig. 1. A notable risk of bias was observed, mainly related to the diversity in ultrasound performers’ training levels. Additionally, five studies lacked explicit clarification regarding the ultrasound criteria for diagnosing forearm fractures.
Meta-analysis
In the evaluation of pediatric distal forearm fractures across 14 studies, the pooled sensitivity and specificity were found to be 94.5 (95% CI 92.7–95.9) and 93.5 (95% CI 89.6–96.0), respectively (Fig. 2). The SROC curve demonstrated an AUC of 0.94 (95% CI 0.92–0.97) (Supplementary Fig. 2). Supplementary Fig. 3, depicting a scattergram of positive and negative likelihood ratios, suggests a high-performance level, ideal for both exclusion and confirmation purposes. According to the Fagan plot study, considering pre-test probabilities of 25%, 50%, and 75% for distal forearm fractures in children, the positive post-test probabilities were 83%, 44%, and 98%, while the negative post-test probabilities were 2%, 6%, and 15%, respectively (Supplementary Fig. 4).
Meta-regression and subgroup analyses
Additional examination involved meta-regression and subgroup assessments, focusing on various covariates.
-
Ultrasound performers’ training status
In studies where individuals with ultrasound training conducted the examinations, the sensitivity and specificity were 94.4% (95% CI 91.2–96.5) and 94.9% (95% CI 91.9–96.9), respectively. In contrast, studies with untrained performers showed sensitivity and specificity of 95.1% (95% CI 92.3–96.9) and 86.3% (95% CI 80.5–90.6), respectively (Fig. 3). The AUC of the SROC was 0.95 (95% CI 0.93–0.98) and 0.94 (95% CI 0.86–0.97) for studies with trained and untrained ultrasound performers, respectively. Analyzing with a bivariate model indicated significantly higher diagnostic accuracy in the subgroup with trained performers (p = 0.03), as depicted in Supplementary Fig. 5. Furthermore, post hoc analysis revealed notably higher specificity in this subgroup (p < 0.01).
Supplementary Fig. 6 illustrates a scattergram of positive and negative LRs for each subgroup.
Moderate heterogeneity was noted in studies with untrained ultrasound performers. A sensitivity analysis identified the study by Herren et al. [13] as a significant outlier. After excluding this study, the overall diagnostic accuracy and specificity remained significantly higher in the subgroup with trained ultrasound performers (Supplementary Figs. 7 and 8).
-
Ultrasound interpreter
In studies where radiologists interpreted the ultrasound, the sensitivity and specificity were 94.5% (95% CI 92.7–95.9) and 93.5% (95% CI 89.6–96.0), respectively. In studies with ultrasound interpreters other than radiologists, the sensitivity and specificity were 94.2% (95% CI 92.1–95.8) and 92.6% (95% CI 88.0–95.6), respectively (Fig. 4). The AUC of the SROC was 0.99 (95% CI 0.93–0.99) for studies with radiologist interpreter and 0.95 (95% CI 0.92–0.97) for studies with interpreters other than radiologists. The diagnostic accuracy did not differ significantly between the two subgroups (Supplementary Fig. 9).
-
Bone under examination (radius vs. ulna)
The sensitivity and specificity of ultrasound examination for detecting radius fractures were 97.1% (95% CI 94.2–98.6) and 94.1% (95% CI 85.8–97.7), respectively. Additionally, the sensitivity and specificity of ultrasound examination for detecting ulnar fractures were 78.9% (95% CI 61.6–89.7) and 97.7% (95% CI 94.6–99.0), respectively (Fig. 5). The AUC of the SROC was 0.98 (95% CI 0.94–0.98) for studies investigating radius fractures and 0.97 (95% CI 0.79–0.99) for studies investigating ulnar fractures. Utilizing a bivariate model, it was observed that the diagnostic accuracy was significantly higher in the subgroup examining radius fractures (p < 0.001), as illustrated in Supplementary Fig. 10. Additionally, a post hoc analysis revealed a notably higher sensitivity in this subgroup (p < 0.001).
Supplementary Fig. 11 displays a scattergram of each subgroup’s positive and negative LRs.
Considerable heterogeneity was observed in both subgroups. A sensitivity analysis was conducted to identify potential outliers and investigate the source of this heterogeneity. This analysis identified the study by Herren et al. [13] as a significant outlier. After excluding this study, the overall diagnostic accuracy and sensitivity remained significantly higher in the subgroup of studies investigating radius fractures. However, post hoc analysis revealed that the specificity of ultrasound for the ulna subgroup was significantly higher than the other subgroup (p < 0.01) (Supplementary Figs. 12 and 13).
-
Ultrasound views (4-view vs. 6-view)
The sensitivity and specificity of the 4-view ultrasound examination for detecting distal forearm fractures were 95.3% (95% CI 90.5–97.7) and 94.4% (95% CI 88.1–97.5), respectively. Additionally, the sensitivity and specificity of the 6-view ultrasound examination were 94.4% (95% CI 92.2–95.9) and 92.9% (95% CI 87.9–96.0), respectively (Supplementary Fig. 14). The AUC of the SROC was 0.96 (95% CI 0.92–0.98) for the 4-view subgroup and 0.94 (95% CI 0.92–0.97) for the 6-view subgroup. The diagnostic accuracy did not differ significantly between the two subgroups (Supplementary Fig. 15).
-
Reporting method (bone-wise vs. patient-wise)
The pooled sensitivity and specificity were examined in two subgroups. In studies reporting results on a bone-wise basis, the sensitivity was 93.8% (95% CI 90.04–96.1), and the specificity was 97.0% (95% CI 93.2–98.7). In contrast, in studies reporting results on a patient-wise basis, the sensitivity was 94.7% (95% CI 92.2–96.4), and the specificity was 90.6% (95% CI 86.3–93.6) (Supplementary Fig. 16). The AUC of the SROC was 0.97 (95% CI 0.92–0.98) for the bone-wise subgroup and 0.96 (95% CI 0.91–0.97) for the patient-wise subgroup. Utilizing a bivariate model, the diagnostic accuracy was observed to be slightly higher in the bone-wise subgroup (p = 0.07), as demonstrated in Supplementary Fig. 17. Furthermore, a post hoc analysis indicated notably higher specificity in the bone-wise subgroup (p = 0.04).
-
Age
In the meta-regression analysis, using a bivariate model to assess the impact of age, no significant influence of the mean age of the study samples was observed as a factor explaining heterogeneity (p = 0.53).
Funnel plot analysis
In Supplementary Fig. 18, paired funnel plots illustrating publication bias and the small study effect are presented. Importantly, the application of Egger’s regression analysis with 2000 bootstrapping revealed significant asymmetry (p = 0.23), suggesting evidence of potential publication bias or a small study effect.
Discussion
This systematic review and meta-analysis extend prior investigations to assess the diagnostic effectiveness of ultrasound in detecting distal forearm fractures in pediatric cases. This study reveals that ultrasonography exhibits a notable sensitivity and a high specificity in the detection of distal forearm fractures in pediatric patients. It proves to be highly accurate in positively identifying cases with fractures and effectively excluding those without. The pooled positive and negative LRs reported further underscore its reliability for both detection and exclusion purposes. These findings position ultrasonography as a valuable tool in clinically assessing distal forearm fractures in pediatrics, aiding healthcare practitioners in making well-informed decisions about patient care.
As an effective diagnostic tool for distal forearm fractures, ultrasonography leverages factors such as good image quality resulting from thin soft tissue and the short distance between the transducer and bone [6]. In contrast to radiography, ultrasonography enables the assessment of soft tissues, including muscle edema, tendons, and joint functions, providing exceptional spatial resolution and multiplanar imaging capabilities. Furthermore, ultrasonography proficiently localizes soft tissue interpositions between fracture fragments [7, 13]. Crucially, it adeptly addresses time constraints in emergency scenarios by facilitating rapid examinations. Ultrasonography eliminates the need for transporting patients to radiology suites and bypasses the subsequent wait for radiologist readings. This expedited process makes a substantial contribution to reducing the overall patient length of stay, effectively mitigating concerns associated with prolonged emergency department wait times [6]. The absence of ionizing radiation, coupled with the opportunity for families to view images during the initial physician visit, underscores the efficiency and patient-centric benefits of ultrasonography in diagnosing distal forearm fractures [7].
Research consistently indicates that ultrasound for detecting pediatric distal forearm fractures is less painful than radiographic imaging. In the study by Chaar-Alvarez et al., the pain score during ultrasound was significantly lower than during radiographic imaging [7]. This aligns with broader literature where patients consistently reported similar or lower pain scores for point-of-care ultrasound (POCUS) compared to X-ray [5]. Furthermore, in the study by Xo et al., the results suggest that pain with ultrasonography is unlikely to limit its use in this diagnostic context [9]. The minimal discomfort associated with POCUS can be attributed to its non-invasive nature, as all images can be obtained without requiring the child to move the affected extremity [5, 9]. This indicates that clinicians can reassure caregivers and children that ultrasonography is generally not a painful procedure.
Our findings indicate that the diagnostic accuracy of ultrasound did not significantly differ between the subgroups of radiologist interpreters and non-radiologist interpreters. However, a significantly higher diagnostic accuracy was observed in the subgroup with trained performers, particularly showcasing notably higher specificity. No difference was noted between trained and untrained individuals in terms of sensitivity. This suggests that ultrasound can effectively rule out distal forearm fractures in children regardless of the operator’s training level. Nevertheless, a crucial distinction emerges when confirming fractures, emphasizing the necessity of specific training. This underscores the importance of skill and expertise in accurately confirming fractures through ultrasound examination. Studies have reported that a standardized training duration of approximately 1 h is sufficient [25,26,27], indicating that the learning curve for bone ultrasonography is not excessively complex, at least for pediatric distal forearm fractures. The study by Galletebeitia Laka et al. demonstrates that a pediatric resident, even without prior POCUS experience, achieved diagnostic accuracy comparable to an experienced emergency department pediatrician after receiving basic training [3]. Similarly, Epema et al. demonstrated that inexperienced physicians can master POCUS of the forearm after a short training period [8]. Moreover, Chaar-Alvarez et al.’s findings confirm the accuracy of ultrasound as a diagnostic tool for nonangulated pediatric forearm fractures, even when reviewed by an experienced, blinded professional relying solely on ultrasound images for diagnosis. In contrast, unblinded bedside diagnoses by less experienced physicians were accurate but to a lesser extent. This indicates that having more ultrasound experience was more crucial and potentially less prone to misleading results than relying solely on additional bedside clinical information for making accurate diagnoses [7].
We noted a significant increase in diagnostic accuracy within the subgroup focused on examining radius fractures, with the analysis highlighting notably higher sensitivity in this category. This trend persisted even after the exclusion of an outlier study. However, upon removing this study, the specificity of ultrasound for the ulna subgroup was found to be significantly higher. Consequently, ultrasound demonstrates greater reliability in excluding radius fractures and proves more effective in confirming ulna fractures. This variability may be attributed to anatomical differences, operator experience and training, variability in patient positioning, characteristics of the study population, and differences in equipment/technology. Further investigation into these factors is necessary to gain a deeper understanding of the nuanced reasons behind the observed differences in diagnostic accuracy for fractures in distinct forearm bones in pediatric cases.
Although the current study’s findings highlighted the reliability of ultrasonography in detecting pediatric distal forearm fractures, it is crucial to acknowledge that this imaging modality may not be universally suitable, especially in cases involving patients with obesity or other factors affecting image quality. Consequently, clinical judgment should guide the choice of the most appropriate imaging modality for each individual patient. Additionally, it is worth noting that ultrasound operators might have been influenced by visible deformities or physical signs during image interpretation, potentially leading to an overestimation of ultrasound accuracy.
While this systematic review centered on the diagnostic utility of ultrasound in pediatric distal forearm fractures, questions about its role post-diagnosis—particularly its potential to inform surgical decisions and support follow-up assessments—remain unexplored. Understanding these aspects is crucial for advancing clinical practice and encourages further investigation into the broader utility of ultrasound in managing pediatric distal forearm fractures.
Conclusions
This study demonstrated the reliability of ultrasonography as an imaging modality for detecting distal forearm fractures in pediatric patients, exhibiting high sensitivity and specificity. Notably, trained performers displayed significantly higher diagnostic accuracy, particularly in terms of enhanced specificity, underscoring the importance of expertise in accurately confirming fractures through ultrasound examination. Further research should specifically address the observed differences in diagnostic accuracy of ultrasound between fractures in the radius and ulna.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Sinikumpu JJ, Nietosvaara Y (2021) Treatment of distal forearm fractures in children. Scand J Surg 110:276–280
Chen L, Kim Y, Moore CL (2007) Diagnosis and guided reduction of forearm fractures in children using bedside ultrasound. Pediatr Emerg Care 23:528–531
GalletebeitiaLaka I, Samson F, Gorostiza I, Gonzalez A, Gonzalez C (2019) The utility of clinical ultrasonography in identifying distal forearm fractures in the pediatric emergency department. Eur J Emerg Med 26:118–122
Mobasseri A, Noorifard P (2022) Ultrasound in the diagnosis of pediatric distal radius fractures: Does it really change the treatment policy? An orthopedic view. J Ultrason 22:e179–e182
Snelling PJ, Jones P, Keijzers G, Bade D, Herd DW, Ware RS (2021) Nurse practitioner administered point-of-care ultrasound compared with X-ray for children with clinically non-angulated distal forearm fractures in the ED: A diagnostic study. Emerg Med J 38:139–145
Ahmed AS, Abdelhady AE, McNicholl B (2018) Ultrasound as a diagnostic tool in paediatric distal forearm fractures. Ir Med J 111:836
Chaar-Alvarez FM, Warkentine F, Cross K, Herr S, Paul RI (2011) Bedside ultrasound diagnosis of nonangulated distal forearm fractures in the pediatric emergency department. Pediatr Emerg Care 27:1027–1032
Epema AC, Spanjer MJB, Ras L, Kelder JC, Sanders M (2019) Point-of-care ultrasound compared with conventional radiographic evaluation in children with suspected distal forearm fractures in the Netherlands: A diagnostic accuracy study. Emerg Med J 36:613–616
Poonai N, Myslik F, Joubert G et al (2017) Point-of-care ultrasound for nonangulated distal forearm fractures in children: Test performance characteristics and patient-centered outcomes. Acad Emerg Med 24:607–616
Ko C, Baird M, Close M, Cassas KJ (2019) The diagnostic accuracy of ultrasound in detecting distal radius fractures in a pediatric population. Clin J Sport Med 29:426–429
Eckert K, Ackermann O, Schweiger B, Radeloff E, Liedgens P (2012) Sonographic diagnosis of metaphyseal forearm fractures in children: A safe and applicable alternative to standard x-rays. Pediatr Emerg Care 28:851–854
Hedelin H, Tingström C, Hebelka H, Karlsson J (2017) Minimal training sufficient to diagnose pediatric wrist fractures with ultrasound. Crit Ultrasound J 9:11
Herren C, Sobottke R, Ringe MJ et al (2015) Ultrasound-guided diagnosis of fractures of the distal forearm in children. Orthop Traumatol Surg Res 101:501–505
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 6:e1000097
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH (2005) Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 58:982–990
Noma H, Matsushima Y, Ishii R (2021) Confidence interval for the AUC of SROC curve and some related methods using bootstrap for meta-analysis of diagnostic accuracy studies. Commun Stat Case Stud Data Anal Appl 7:344–358
Holling H, Böhning W, Masoudi E, Böhning D, Sangnawakij P (2020) Evaluation of a new version of I2 with emphasis on diagnostic problems. Commun Stat Case Stud Data Anal Appl 49:942–972
Zwinderman AH, Bossuyt PM (2008) We should not pool diagnostic likelihood ratios in systematic reviews. Stat Med 27:687–697
Noma H (2020) Discussion on “Testing small study effects in multivariate meta-analysis” by Chuan Hong, Georgia Salanti, Sally Morton, Richard Riley, Haitao Chu, Stephen E. Kimmel, and Yong Chen. Biometrics 76:1255–1259
Noma H (2023) MVPBT: R package for publication bias tests in meta-analysis of diagnostic accuracy studies. arXiv Available via: https://arxiv.org/abs/2209.07270. Accessed: October 20, 2023
Viechtbauer W (2010) Conducting meta-analyses in R with the metafor package. J Stat Softw 36:1–48
Balduzzi S, Rücker G, Schwarzer G (2019) How to perform a meta-analysis with R: A practical tutorial. Evid Based Ment Health 22:153–160
Williamson D, Watura R, Cobby M (2000) Ultrasound imaging of forearm fractures in children: A viable alternative? J Accid Emerg Med 17:22–24
Sinha TP, Bhoi S, Kumar S et al (2011) Diagnostic accuracy of bedside emergency ultrasound screening for fractures in pediatric trauma patients. J Emerg Trauma Shock 4:443–445
Ackermann O, Liedgens P, Eckert K et al (2001) (2010) Ultrasound diagnosis of juvenile forearm fractures. J Med Ultrason 37:123–127
Weinberg ER, Tunik MG, Tsung JW (2010) Accuracy of clinician-performed point-of-care ultrasound for the diagnosis of fractures in children and young adults. Injury 41:862–868
Acknowledgements
We acknowledge the application of ChatGPT, a language model created by OpenAI with the GPT-3.5 framework, which facilitated the refinement of language accuracy in the manuscript editing process. This collaborative effort resulted in heightened readability and improved linguistic quality. Nevertheless, the authors individually reviewed and edited the content as required, assuming complete accountability for the substance of the publication.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium. No funding was received from public, commercial, or not-for-profit sectors for this research.
Author information
Authors and Affiliations
Contributions
The project’s conception was shaped by the collaborative efforts of all authors. Ali Gholamrezanezhad, Pauravi S. Vasavada, and Jennifer H. Johnston provided valuable scientific insights during the revision phase. Amir Hassankhani, Melika Amoukhteh, and Delaram J. Ghadimi played pivotal roles in conducting database searches, extracting data, drafting, and critically revising the manuscript to include essential intellectual content. Payam Jannatdoust and Parya Valizadeh made significant contributions to data analysis and interpretation. The final manuscript underwent a thorough review by all authors and received unanimous approval.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Amir Hassankhani and Melika Amoukhteh are co-first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hassankhani, A., Amoukhteh, M., Jannatdoust, P. et al. A meta-analysis on the diagnostic utility of ultrasound in pediatric distal forearm fractures. Emerg Radiol 31, 213–228 (2024). https://doi.org/10.1007/s10140-024-02208-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-024-02208-2