Abstract
Purpose
Gastrointestinal perforation is a significant injury that originates mainly from gastrointestinal ulcers. It is associated with a high rate of morbidity and mortality. The height of the column of the air under the diaphragm can be used to estimate the amount of peritoneal soiling due to viscus perforation. This study aimed to determine the correlation between this estimate and the incidence of morbidity and mortality.
Methods
To achieve this aim, a prospective cohort study was conducted on 83 patients at Kasr al ainy hospital who, between March 2021 and March 2022, presented to the emergency department with free air under the diaphragm at chest X-ray and required surgical intervention for a perforated viscus. For each case, the amount of peritoneal soiling and the amount of air under the diaphragm as determined by a chest X-ray were recorded.
Results
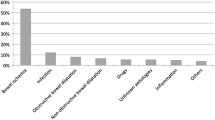
The mean air under the diaphragm in a plain erect chest X-ray was 1.78 ± 1.92 cm, and the mean amount of peritoneal soiling was 1201.83 ± 948.99 CC. There are positive correlations between the amount of air under the diaphragm as shown on an X-ray and the size of the perforation (p = 0.034), the amount of peritoneal soiling (p = 0.003), and the mortality (p = 0.013).
Conclusion
There was a statistically significant correlation between air under the diaphragm according to X-ray and the amount of peritoneal soiling in patients with a perforated viscus. This measure can be used as a sensitive tool to predict morbidity and mortality as more free air in the chest X-ray is associated with significant mortality. These results may enhance the decision making using sensitive and available tool of diagnosis.




Similar content being viewed by others
Data Availability
Data accessibility exists.
References
Brookes A, Chan YC, Fish R, Foo FJ, Hogan A, Konig T et al (2020) Emergency surgery. Cracking the Intercollegiate General Surgery FRCS Viva 2ème: a Revision Guide 11:317.
Weledji EP (2020) An overview of gastroduodenal perforation. Front Surg 7:573901. https://doi.org/10.3389/fsurg.2020.573901
Dugad DD, Mohanty DD, Mahobia DHS, Saha DA (2021) A comparative study of subcutaneous negative pressure versus simple closure of skin incision following surgery for hollow viscus perforation. Int J Surg Sci 5:269–271. https://doi.org/10.33545/surgery.2021.v5.i2e.706
Umapathi P (2018) Clinical study and management of peritonitis secondary to hollow viscous perforation. J Evol Med Dent Sci 7:3974–3979
Liu X, Sheng W, Gong Y, Gao W, Zhang B (2021) Negative surgical exploration in suspected gastrointestinal perforation: trend, preoperative predictors, and etiologies. Ann Transl Med 9:832. https://doi.org/10.21037/atm-20-8158
Cadena M, Solano J, Caycedo N, Gomez D, Vinck EE, Quiroga P et al (2019) Tension pneumoperitoneum: case report of a rare form of acute abdominal compartment syndrome. Int J Surg Case Rep 55:112–116. https://doi.org/10.1016/j.ijscr.2019.01.014
Grewal JS, Mayer S, Beaty J, Formaro D (2021) A rare case of spontaneous idiopathic pneumoperitoneum presenting as abdominal pain. Cureus 13:e15158. https://doi.org/10.7759/cureus.15158
Martins BAA, Galletti RR, dos Santos Neto JM, Mendes CN (2018) A case of perforated jejunal diverticulum: an unexpected cause of pneumoperitoneum in a patient presenting with an acute abdomen. Am J Med Case Rep 19:549–552
Joudeh LA, Newman MG (2018) Nonoperative management of pneumoperitoneum after colonoscopy. Taylor & Francis 31:465–466
Demiroluk S, Salihoglu ZIYA, Bozkurt P, Hayirlioglu M, Kose Y (2007) Effect of pneumoperitoneum on level of plasma potassium. Middle East J Anesthesiol 19:61–70
Grabowski JE, Talamini MA (2009) Physiological effects of pneumoperitoneum. J Gastrointest Surg 13:1009–1016. https://doi.org/10.1007/s11605-008-0662-0
Mularski RA, Sippel JM, Osborne ML (2000) Pneumoperitoneum: a review of nonsurgical causes. Crit Care Med 28:2638–2644. https://doi.org/10.1097/00003246-200007000-00078
Di Saverio S, Bassi M, Smerieri N, Masetti M, Ferrara F, Fabbri C et al (2014) Diagnosis and treatment of perforated or bleeding peptic ulcers: 2013 WSES position paper. World J Emerg Surg 9:45. https://doi.org/10.1186/1749-7922-9-45
Gu WJ, Wang F, Bakker J, Tang L, Liu JC (2014) The effect of goal-directed therapy on mortality in patients with sepsis-earlier is better: a meta-analysis of randomized controlled trials. Crit Care 18:1–10. https://doi.org/10.1186/s13054-014-0570-5
Hawramy TA, Mohammed DA, Tahir BH (2019) Serum amylase level measurement in acute abdominal pain. Kurd. J Appl Res 157–165.
Chen YY, Ko TY, Huang YF (2020) Pneumatosis intestinalis causing pneumoperitoneum. Dig Liver Dis 52:351. https://doi.org/10.1016/j.dld.2019.12.006
Alves Martins BA, Rodrigues Galletti R, Dos Santos Marinho, Neto J, Neiva Mendes C (2018) A case of perforated jejunal diverticulum: an unexpected cause of pneumoperitoneum in a patient presenting with an acute abdomen. Am J Case Rep 19:549–552. https://doi.org/10.12659/AJCR.909131
Kumar D, Cortés-Penfield NW, El-Haddad H, Musher DM (2018) Bowel perforation resulting in necrotizing soft-tissue infection of the abdomen, flank, and lower extremities. Surg Infect 19:467–472. https://doi.org/10.1089/sur.2018.022
Nouri D, Soleimanian Gj N, Ataei F, Mohammadi M (2021) Effects of sex, age, size and location of perforation on the sensitivity of erect chest X-ray for gastroduodenal perforation. Radiography 27:1158–1161. https://doi.org/10.1016/j.radi.2021.06.006
Chiu YH, Chen JD, Tiu CM, Chou YH, Yen DHT, Huang CI et al (2009) Reappraisal of radiographic signs of pneumoperitoneum at emergency department. Am J Emerg Med 27:320–327. https://doi.org/10.1016/j.ajem.2008.03.004
Zhang C, Harris A (2016) Approach to the imaging of abnormal intra-abdominal gas. European Congress of Radiology-ECR.
Hajibandeh S, Shah J, Hajibandeh S, Asim U, Purchase D, Maw A et al (2022) Erect chest X-ray is inadequately diagnostic and falsely reassuring in assessment of abdominal visceral perforation. Radiography 28:249–250. https://doi.org/10.1016/j.radi.2021.10.014
Shakya VC, Pangeni A, Karki S, Sharma LR (2021) Evaluation of Mannheim’s peritonitis index in prediction of mortality in patients with non-traumatic hollow viscus perforation peritonitis. J Nepal Health Res Counc 19:179–184. https://doi.org/10.33314/jnhrc.v19i1.3258
Sharma S, Kaneria R, Sharma A, Khare A (2019) Perforation peritonitis: a clinical study regarding etiology, clinical presentation and management strategies. Int Surg J 6:4455–4459. https://doi.org/10.18203/2349-2902.isj20195412
Malfertheiner P, Dent J, Zeijlon L, Sipponen P, Veldhuyzen Van Zanten SJO, Burman CF et al (2002) Impact of Helicobacter pylori eradication on heartburn in patients with gastric or duodenal ulcer disease—results from a randomized trial programme. Aliment Pharmacol Ther 16:1431–2142. https://doi.org/10.1046/j.1365-2036.2002.01285.x
Schubert ML, Peura DA (2008) Control of gastric acid secretion in health and disease. Gastroenterology 134:1842–1860. https://doi.org/10.1053/j.gastro.2008.05.021
Buck DL, Møller MH (2014) Influence of body mass index on mortality after surgery for perforated peptic ulcer. Br J Surg 101:993–999. https://doi.org/10.1002/bjs.9529
Søreide K, Thorsen K, Søreide JA (2014) Strategies to improve the outcome of emergency surgery for perforated peptic ulcer. Br J Surg 101:e51–e64. https://doi.org/10.1002/bjs.9368
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The authors declare that the approval of this study was obtained from our Institutional Research Ethics Committee. Code: MS-211–2021.
Statement for informed consent
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abosayed, A.K., Dayem, A.Y.A., Shafik, I. et al. Prognostic value of free air under diaphragm on chest radiographs in correlation with peritoneal soiling intraoperatively. Emerg Radiol 30, 99–106 (2023). https://doi.org/10.1007/s10140-022-02111-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-022-02111-8