Abstract
Purpose
The use of spectral Doppler, peak systolic velocity (PSV), and resistive index (RI) imaging criteria to improve the accuracy of acute appendicitis diagnosis is hypothesized.
Methods
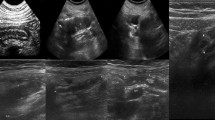
Graded compression ultrasound was performed for suspected patients. The spectral Doppler evaluation was conducted while observing the appendix. A total of 152 patients (82 males and 70 females, ages 4–63 years, mean age of 24.5 years) were examined using the spectral Doppler waveform between 2018 and 2019. RI and PSV values of patients with and without appendicitis were compared to histopathologic findings. SPSS 26 was used to analyze the data, including using descriptive statistics and measures of sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV).
Results
Appendicitis was confirmed in 95 patients (62.5%) and rejected in 57 patients (37.5%). For the diagnosis of appendicitis, the area under the curve (AUC) of receiver operating characteristic (ROC) for RI (0.92 with 95% confidence interval (CI): 0.88, 0.97; P = 0.001) and PSV (0.96, with 95% CI: 0.93, 1.00; P = 0.001) was calculated. The discriminatory RI ≥ 0.49 demonstrated high sensitivity (90.5%) and low specificity (86%), and the discriminatory PSV ≥ 9.6 cm/s had high specificity (94.7%) and sensitivity (94.7%) for appendicitis.
Conclusion
By incorporating spectral Doppler criteria into routine graded compression ultrasound, the diagnostic accuracy of acute appendicitis was increased. In comparison, high PSV and RI values of the appendix with a cut-off point of 9.6 cm/s and 0.49 differ significantly between positive and negative appendectomy patients.
Graphical abstract


Similar content being viewed by others
References
Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V (2012) Changing epidemiology of acute appendicitis in the United States: study period 1993–2008. J Surg Res 175(2):185–190. https://doi.org/10.1016/j.jss.2011.07.017
Austin-Page LR, Pham PK, Elkhunovich M (2020) Evaluating changes in diagnostic accuracy of ultrasound for appendicitis: does practice make perfect? J Emerg Med 59(4):563–572. https://doi.org/10.1016/j.jemermed.2020.06.001
Monsonis B, Mandoul C, Millet I, Taourel P (2020) Imaging of appendicitis: tips and tricks. Eur J Radiol 130:109165. https://doi.org/10.1016/j.ejrad.2020.109165
Cooper M, Jurgielewicz P, Welch K (2020) Diagnosis of acute uncomplicated appendicitis with point of care ultrasound in stable emergency department patient. Vis J Emerg Med 18(September 2019):2019–2020. https://doi.org/10.1016/j.visj.2019.100668
Benedetto G, Ferrer Puchol MD, LlavataSolaz A (2019) Suspicion of acute appendicitis in adults. The value of ultrasound in our hospital. Radiología (Engl Ed) 61(1):51–59. https://doi.org/10.1016/j.rxeng.2018.11.010
Lourenco P, Brown J, Leipsic J, Hague C (2016) The current utility of ultrasound in the diagnosis of acute appendicitis. Clin Imaging 40(5):944–948. https://doi.org/10.1016/j.clinimag.2016.03.012
Segev L, Segev Y, Rayman S, Nissan A, Sadot E (2016) The diagnostic performance of ultrasound for acute appendicitis in pregnant and young nonpregnant women: a case-control study. Int J Surg 34:81–85. https://doi.org/10.1016/j.ijsu.2016.08.021
Chan I, Bicknell SG, Graham M (2005) Utility and diagnostic accuracy of sonography in detecting appendicitis in a community hospital. Am J Roentgenol 184(6):1809–1812. https://doi.org/10.2214/ajr.184.6.01841809
Lehmann D, Uebel P, Weiss H, Fiedler L, Bersch W (2000) Sonographische darstellbarkeit der normalen und der entzundeten appendix-bei patienten mit rechtsseitigen unterbauchschmerzen. Ultraschall Med 21(3):101–106. https://doi.org/10.1055/s-2000-3788
Eng KA, Abadeh A, Ligocki C, Lee YK, Moineddin R, Adams-Webber T, Schuh S, Doria AS (2018) Acute appendicitis: a meta-analysis of the diagnostic accuracy of US, CT, and MRI as second-line imaging tests after an initial US. Radiology 288(3):717–727. https://doi.org/10.1148/radiol.2018180318
Körner H, Söndenaa K, Söreide JA, Andersen E, Nysted A, Lende TH, Kjellevold KH (1997) Incidence of acute nonperforated and perforated appendicitis: age-specific and sex-specific analysis. World J Surg 21(3):313–317. https://doi.org/10.1007/s002689900235
Raman SS, Lu DSK, Kadell BM, Vodopich DJ, Sayre J, Cryer H (2002) Accuracy of nonfocused helical CT for the diagnosis of acute appendicitis: a 5-year review. Am J Roentgenol 178(6):1319–1325. https://doi.org/10.2214/ajr.178.6.1781319
Wong SK, Chan LP, Yeo A (2002) Helical CT imaging and clinically suspected appendicitis: correlation of CT and histological findings. Clin Radiol 57(8):741–745. https://doi.org/10.1053/crad.2002.0950
Fuchs JR, Schlamberg JS, Shortsleeve MJ, Schuler JG (2002) Impact of abdominal CT imaging on the management of appendicitis: an update. J Surg Res 106(1):131–136. https://doi.org/10.1006/jsre.2002.6441
Miglioretti DL, Johnson E, Williams A, Greenlee RT, Weinmann S, Solberg LI, Feigelson HS, Roblin D, Flynn MJ, Vanneman N, Smith-Bindman R (2013) The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr 167(8):700. https://doi.org/10.1001/jamapediatrics.2013.311
Sodickson A, Baeyens PF, Andriole KP, Prevedello LM, Nawfel RD, Hanson R, Khorasani R (2009) Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology 251(1):175–184. https://doi.org/10.1148/radiol.2511081296
Pelin M, Paquette B, Revel L, Landecy M, Bouveresse S, Delabrousse E (2018) Acute appendicitis: factors associated with inconclusive ultrasound study and the need for additional computed tomography. Diagn Interv Imaging 99(12):809–814. https://doi.org/10.1016/j.diii.2018.07.004
Penticuff R, Jeffrey RB, Olcott EW (2021) Hyperechoic periappendiceal fat: evaluation of criteria for improving specificity in the sonographic diagnosis of appendicitis in pediatric patients. J Ultrasound Med 40(2):285–296. https://doi.org/10.1002/jum.15399
Partain KN, Patel A, Travers C, McCracken CE, Loewen J, Braithwaite K, Heiss KF, Raval MV (2016) Secondary signs may improve the diagnostic accuracy of equivocal ultrasounds for suspected appendicitis in children. J Pediatr Surg 51(10):1655–1660. https://doi.org/10.1016/j.jpedsurg.2016.03.005
Baldisserotto M, Peletti AB (2007) Is colour Doppler sonography a good method to differentiate normal and abnormal appendices in children? Clin Radiol 62(4):365–369. https://doi.org/10.1016/j.crad.2006.11.009
Stewart JK, Olcott EW, Jeffrey RB (2012) Sonography for appendicitis: nonvisualization of the appendix is an indication for active clinical observation rather than direct referral for computed tomography. J Clin Ultrasound 40(8):455–461. https://doi.org/10.1002/jcu.21928
Linam LE, Munden M (2012) Sonography as the first line of evaluation in children with suspected acute appendicitis. J Ultrasound Med 31(8):1153–1157. https://doi.org/10.7863/jum.2012.31.8.1153
Kessler N, Cyteval C, Gailix B, Lesnik A, Blayac PM, Pujol J, Bruel JM, Taourel P (2004) Appendicitis: evaluation of sensitivity, specificity, and predictive values of US, Doppler US, and laboratory findings. Radiology 230(2):472–478. https://doi.org/10.1148/radiol.2302021520
Ohba G, Hirobe S, Komori K (2016) The usefulness of combined B mode and doppler ultrasonography to guide treatment of appendicitis. Eur J Pediatr Surg 26(6):533–536. https://doi.org/10.1055/s-0035-1570756
Matthew Fields J, Davis J, Alsup C, Bates A, Au A, Adhikari S, Farrell I (2017) Accuracy of point-of-care ultrasonography for diagnosing acute appendicitis: a systematic review and meta-analysis. Acad Emerg Med 24(9):1124–1136. https://doi.org/10.1111/acem.13212
Quillin SP, Siegel MJ (1994) Appendicitis: efficacy of color Doppler sonography. Radiology 191(2):557–560. https://doi.org/10.1148/radiology.191.2.8153340
Quillin SP, Siegel MJ (1993) Color Doppler US of children with acute lower abdominal pain. Radiographics 13(6):1281–1293; discussion 1294. https://doi.org/10.1148/radiographics.13.6.8290724
Chan L, Shin LK, Pai RK, Jeffrey RB (2011) Pathologic continuum of acute appendicitis: sonographic findings and clinical management implications. Ultrasound Q 27(2):71–79. https://doi.org/10.1097/RUQ.0b013e31821b6eea
Shin LK, Jeffrey RB, Berry GJ, Olcott EW (2017) Spectral Doppler waveforms for diagnosis of appendicitis: potential utility of point peak systolic velocity and resistive index values. Radiology 285(3):990–998. https://doi.org/10.1148/radiol.2017162251
Ung C, Chang ST, Jeffrey RB, Patel BN, Olcott EW (2013) Sonography of the normal appendix: its varied appearance and techniques to improve its visualization. Ultrasound Q 29(4):333–341. https://doi.org/10.1097/RUQ.0b013e3182a2aa8e
Chang ST, Jeffrey RB, Olcott EW (2014) Three-step sequential positioning algorithm during sonographic evaluation for appendicitis increases appendiceal visualization rate and reduces CT use. Am J Roentgenol 203(5):1006–1012. https://doi.org/10.2214/AJR.13.12334
Kruskal JB, Newman PA, Sammons LG, Kane RA (2004) Optimizing Doppler and color flow US: application to hepatic sonography. Radiographics 24(3):657–675. https://doi.org/10.1148/rg.243035139
Pozniak MA, Zagzebski JA, Scanlan KA (1992) Spectral and color Doppler artifacts. Radiographics 12(1):35–44. https://doi.org/10.1148/radiographics.12.1.1734480
Incesu L, Yazicioglu AK, Selcuk MB, Ozen N (2004) Contrast-enhanced power Doppler US in the diagnosis of acute appendicitis. Eur J Radiol 50(2):201–209. https://doi.org/10.1016/S0720-048X(03)00102-5
Anandalwar SP, Callahan MJ, Bachur RG, Feng C, Sidhwa F, Karki M, Taylor GA, Rangel SJ (2015) Use of white blood cell count and polymorphonuclear leukocyte differential to improve the predictive value of ultrasound for suspected appendicitis in children. J Am Coll Surg 220(6):1010–1017. https://doi.org/10.1016/j.jamcollsurg.2015.01.039
Jaremko JL, Crockett A, Rucker D, Magnus KG (2011) Incidence and significance of inconclusive results in ultrasound for appendicitis in children and teenagers. Can Assoc Radiol J 62(3):197–202. https://doi.org/10.1016/j.carj.2010.03.009
Nielsen JW, Boomer L, Kurtovic K, Lee E, Kupzyk K, Mallory R, Adler B, Bates DG, Kenney B (2015) Reducing computed tomography scans for appendicitis by introduction of a standardized and validated ultrasonography report template. J Pediatr Surg 50(1):144–148. https://doi.org/10.1016/j.jpedsurg.2014.10.033
Patriquin HB, Garcier JM, Lafortune M, Yazbeck S, Russo P, Jequier S, Ouimet A, Filiatrault D (1996) Appendicitis in children and young adults: Doppler sonographic-pathologic correlation. Am J Roentgenol 166(3):629–633. https://doi.org/10.2214/ajr.166.3.8623640
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bakhshandeh, T., Maleknejad, A., Sargolzaie, N. et al. The utility of spectral Doppler evaluation of acute appendicitis. Emerg Radiol 29, 371–375 (2022). https://doi.org/10.1007/s10140-021-02010-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-021-02010-4