Abstract
Purpose
The purpose of our study was to assess trends in the imaging of suspected appendicitis in adult patients in emergency departments of academic centers in Canada.
Methods
A questionnaire was sent to all 17 academic centers in Canada to be completed by a radiologist who works in emergency radiology. The questionnaires were sent and collected over a period of 4 months from October 2015 to February 2016.
Results
Sixteen centers (94%) responded to the questionnaire. Eleven respondents (73%) use IV contrast–enhanced computed tomography (CT) as the imaging modality of choice for all patients with suspected appendicitis. Thirteen respondents (81%) use ultrasound as the first modality of choice in imaging pregnant patients with suspected appendicitis. Eleven respondents (69%) use ultrasound (US) as the first modality of choice in patients younger than 40 years of age. Ten respondents (67%) use ultrasound as the first imaging modality in female patients younger than 40 years of age. When CT is used, 81% use non-focused CT of the abdomen and pelvis, and 44% of centers use oral contrast. Thirteen centers (81%) have ultrasound available 24 h a day/7 days a week. At 12 centers (75%), ultrasound is performed by ultrasound technologists. Four centers (40%) perform magnetic resonance imaging (MRI) in suspected appendicitis in adult patients at the discretion of the attending radiologist. Eleven centers (69%) have MRI available 24/7. All 16 centers (100%) use unenhanced MRI.
Conclusions
Various imaging modalities are available for the work-up of suspected appendicitis. Although there are North American societal guidelines and recommendations regarding the appropriateness of the multiple imaging modalities, significant heterogeneity in the first-line modalities exist, which vary depending on the patient demographics and resource availability. Imaging trends in the use of the first-line modalities should be considered in order to plan for the availability of the imaging examinations and to consider plans for an imaging algorithm to permit standardization across multiple centers. While this study examined the imaging trends specifically in Canada, there are implications to other countries seeking to streamline imaging protocols and determining appropriateness of the first-line imaging modalities.



Similar content being viewed by others
References
Skinner HG, Blanchard J, Elixhauser A (2014) Trends in emergency department visits, 2006–2011. HCUP Statistical Brief #179. Agency for Healthcare Research and Quality. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb179-Emergency-Department-Trends.pdf. Accessed 6 February 2016
Weiss AJ, Elixhauser A, Andrews RM (2014) Characteristics of operating room procedures in U.S. hospitals, 2011. HCUP Statistical Brief #170. Agency for Healthcare Research and Quality. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb170-Operating-Room-Procedures-United-States-2011.pdf. Accessed 6 February 2016
Flum DR, Koepsell T (2002) The clinical and economic correlates of misdiagnosed appendicitis: nationwide analysis. Arch Surg 137(7):799–804
Doria AS, Moineddin R, Kellenberger CJ et al (2006) US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology 241(1):83–94
American College of Radiology (2013) Appropriateness criteria: right lower quadrant pain—suspected appendicitis. ACR website.https://acsearch.acr.org/docs/69357/Narrative/. Accessed 15 Jan 2016
Canadian Association of Radiology (2012) CAR diagnostic imaging referral guidelines: gastrointestinal system. CAR website. http://www.car.ca/uploads/standards%20guidelines/car-referralguidelines-g-en_20120918.pdf. Accessed 15 Jan 2016
Drake FT, Florence MG, Johnson MG et al (2012) Progress in the diagnosis of appendicitis: a report from Washington State’s Surgical Care and Outcomes Assessment Program. Ann Surg 256(4):586–594
Heverhagen JT, Pfestroff K, Heverhagen AE, Klose KJ, Kessler K, Sitter H (2012) Diagnostic accuracy of magnetic resonance imaging: a prospective evaluation of patients with suspected appendicitis. J Magn Reson Imaging 35(3):617–623
Otero HJ, Ondategui-Parra S, Erturk SM, Ochoa RE, Gonzalez-Beicos A, Ros PR (2008) Imaging utilization in the management of appendicitis and its impact on hospital charges. Emerg Radiol 15(1):23–28
Keyzer C, Cullus P, Tack D, De Maertelaer V, Bohy P, Gevenois PA (2009) MDCT for suspected acute appendicitis in adults: impact of oral and IV contrast media at standard dose and simulated low-dose techniques. AJR 193(5):1272–1281
Alabousi A, Patlas MN, Sne N, Katz DS (2015) Is oral contrast necessary for multidetector computed tomography imaging of patients with acute abdominal pain? Can Assoc Radiol J 66(4):318–322
Pinto F, Pinta A, Russo A et al (2013) Accuracy of ultrasonography in the diagnosis of acute appendicitis in adult patients: review of the literature. Crit Ultrasound J 5(Suppl 1):S2
Parker L, Nazarian LN, Gingold EL, Palit CD, Hoey CL, Frangos AJ (2014) Cost and radiation savings of partial substitution of ultrasound for CT in appendicitis evaluation: a national projection. AJR 202(1):124–135
O’Malley ME, Alharbi F, Chawla TP, Moshonov H (2016) CT following US for possible appendicitis: anatomic coverage. Eur Radiol 26:532–538
Bouyou J, Gaujoux S, Marcellin L et al (2015) Abdominal emergencies during pregnancy. J Visc Surg 152(6 Suppl):105–115
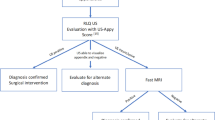
Ramalingam V, LeBedis C, Kelly JR, Uyeda J, Soto JA, Anderson SW (2015) Evaluation of a sequential multi-modality imaging algorithm for the diagnosis of acute appendicitis in the pregnant female. Emerg Radiol 22:125–132
Ditkofsky NG, Singh A, Avery L, Novelline RA (2014) The role of emergency MRI in the setting of acute abdominal pain. Emerg Radiol 21(6):615–624
Rice-Townsend S, Barnes JN, Hall M, Baxter JL, Rangel SJ (2014) Variation in practice and resource utilization associated with the diagnosis and management of appendicitis at freestanding children’s hospitals: implications for value-based comparative analysis. Ann Surg 259(6):1228–1234
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Appendices
Appendix 1. The questionnaire sent to respondents.
-
1.
Number of beds at your hospital :
-
A.
< 250
-
B.
250-500
-
C.
500
-
2.
What is the modality of choice for imaging of ALL patients with suspected appendicitis at your hospital:
-
A.
Unenhanced MDCT
-
B.
Contrast-enhanced MDCT
-
C.
US
-
D.
MRI
-
A.
-
3.
What is the modality of choice for imaging pregnant patients with suspected appendicitis at your practice:
-
A.
Unenhanced MDCT
-
B.
Contrast-enhanced MDCT
-
C.
US
-
D.
MRI
-
A.
-
4.
What is the modality of choice for imaging patients younger than 40 years of age with suspected appendicitis at your hospital:
-
A.
Unenhanced MDCT
-
B.
Contrast-enhanced MDCT
-
C.
US
-
D.
MRI
-
A.
-
5.
How is MDCT performed:
-
A.
Non-focused CT
-
B.
Focused CT
-
A.
-
6.
What is your oral contrast departmental protocol for MDCT in patients with suspected appendicitis?
-
A.
All patients
-
B.
No patients
-
C.
Patients with BMI less than 25
-
D.
We have no oral contrast departmental protocol
-
7.
What is your departmental protocol for US in patients with suspected appendicitis?
-
A.
Not performed
-
B.
Performed in all patients as first imaging test
-
C.
Performed as first test in female patients younger than 40 years old
-
D.
Used as problem-solving tool after MDCT
-
E.
Preference of referring physician
-
F.
We have no US departmental protocol
-
8.
Availability of US at your hospital:
-
A.
24/7
-
B.
8:00-17:00
-
C.
8:00-23:00
-
A.
-
9.
US performed by:
-
A.
US technologist
-
B.
Resident
-
C.
Attending radiologist
-
A.
-
10.
MRI in patients with suspected appendicitis is:
-
A.
Not performed
-
B.
Performed in all patients as first imaging test
-
C.
Performed as first test in patients younger than 40 years old
-
D.
Used as problem-solving tool after MDCT
-
E.
Performed at the preference of attending radiologist
-
F.
Performed at the preference of referring physician
-
11.
Availability of MRI:
-
A.
24/7
-
B.
8:00-17:00
-
C.
8:00-23:00
-
A.
-
12.
MRI protocol:
-
A.
Unenhanced
-
B.
Contrast-enhanced
-
A.
Appendix 2. Selected comments by respondents.
Seven respondents use MRI in pregnant patients only if US nondiagnostic. One respondent uses MRI as a problem-solving tool after CT in pregnant patients only. One respondent uses MRI performed as the first test in pregnant patients only. MRI is used in pregnant patients based on the preference of the attending radiologist or referring physician by one respondent.
One respondent uses US as a first-line test in patients younger than 40 years who do not have elevated BMIs. One respondent uses US as the first test in males less than 40 years. One respondent specified that they use US as the first choice in pediatric patients, pregnant patients, and thin adults.
One respondent uses IV contrast-enhanced MDCT in patients >40 or with large BMI
Rights and permissions
About this article
Cite this article
Tan, V.F., Patlas, M.N. & Katz, D.S. Imaging trends in suspected appendicitis—a Canadian perspective. Emerg Radiol 24, 249–254 (2017). https://doi.org/10.1007/s10140-016-1472-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-016-1472-4